Abstract
Aim: Describe the 3- and 6-month outcomes and perceptions of older adults who participated in a HOP-UP-PT clinical trial. Methods: A questionnaire was administered to HOP-UP-PT participants to garner frequency of self-reported falls, healthcare utilization, perceptions of interventions, and fiscal considerations 3- and 6- months after program completion. Results: 76 total respondents, mean age 77 (SD = 7) years and 75% female. A fall was reported by 12% and 16%, additional therapy needs by 16% and 17%, and hospitalization by 3% and 6% at the 3- and 6-month encounters, respectively. Respondents agreed or strongly agreed to positive benefits of the HOP-UP-PT interventions as follows: exercise (71%, 69%), wearable activity monitor (59%, 59%), automated blood pressure monitor (78%, 87%), and improved nutrition (48%, 41%). Respondents were willing to contribute 10% of program cost and 93% supported insurers covering the cost gap. Conclusion: HOP-UP-PT participants had positive outcomes and perceptions in after program participation.
Introduction
As the number of U.S. adults over 65 years of age continues to grow, burdens related to physical restrictions, functional limitations, and medical conditions will increasingly impact society.Citation1 There is an urgent need to address the needs of this age demographic, as more than 10,000 adults are projected to age into this population daily over the next decade.Citation1 Prior evidence suggests that there is benefit to individuals and society when older adults are provided with the tools to age safely in place and remain active in their homes and community.Citation2 Cise et al. reported that older adults perceive “successful aging-in-place” (SAIP) to include acceptance, independence, happiness, enjoyment, stable physical and cognitive abilities, as well as a safe environment to live in.Citation3 Understanding these perceptions is essential to individualize and refine priorities for optimal SAIP for this age demographic.
Long-term care placement, such as assisted living facilities and nursing homes, can occur after falls, injuries from falls, fear of falling, and decreased strength, agility and balance.Citation4 Three million older adults are treated in the emergency room annually for injuries related to falls including broken bones and head injuries, according to the Center for Disease Control and Prevention (CDC).Citation5 Medical treatment following these injuries is estimated to cost $50 billion annually in the United States (U.S.).Citation6 Additionally, a fear of falling can produce negative sequelae including immobility, reduced physical activity, functional dependence, and serious injury which can compound the risk of a future fall.Citation6,Citation7 Physical therapist (PT) led preventative programs and healthcare interventions have demonstrated growing evidence for their value in aging community-dwelling populations.Citation8–10 Specifically, programs with an emphasis on addressing risks associated with unsuccessful SAIP and intervening early when risks are identified, also known as an upstream approach to care, have proven beneficial.Citation10
Higher rates of emergency room visits, hospitalizations, medical expenditures, and noncompliance have been identified among those who are homebound or less able to leave their home.Citation7 Musich et al. suggest that upstream-focused screening and care coordination for homebound older adults is warranted, but the authors described resource limitations that reduce the ability to deliver in-home interventions. One upstream-focused program that has demonstrated progress in mitigating this barrier, HOP-UP-PT (Home-Based Older Persons Upstreaming Prevention Physical Therapy), has evidence supporting the use of a senior community center referral directly to a PT in combination with a multimodal approach to assessments and interventions can reduce fall risk.Citation10 HOP-UP-PT program participants are referred to PTs from their local community senior center staff after a risk of functional decline or a fall is identified.Citation10 Specifically, the HOP-UP-PT clinical trial reported improvement in fall risk metrics among community dwelling older adult participants and an 8-fold decrease in falls among the participants identified with the highest fall risk.Citation10
During an earlier observational study of the HOP-UP-PT program, a follow up telephone questionnaire was conducted 1-3 months after program participation to gain insight into the potential long term impact of the program.Citation9,Citation11 Wilson et al. identified early positive trends associated with program participation which included benefits from the wearable activity tracker, Otago Exercise Program, automated blood pressure monitor, home modifications, and nutritional recommendations.Citation11 Of the 18 participants in the pilot study, five indicated a willingness to pay for a portion of the prevention focused HOP-UP-PT program out of pocket, while 13 indicated they would not pay any program expenses.Citation11 When asked thought on an appropriate price point for this program (anticipate cost $1200-$1500), nine participants stated $0, one participant stated over $500, one participant stated it should be covered by insurance, and the remaining participants indicated between $100 and $300.Citation11 Given the promising trends identified in long-term follow up of the observational study, implementation of a modified questionnaire using a new cohort of HOP-UP-PT participants enrolled in a statewide randomized controlled trial (RCT) with intent to capture impact data from a larger population is warranted. Therefore, the purpose of this study was to describe the 3- and 6-month self-reported outcomes and perceptions of older adults who participated in a statewide HOP-UP-PT clinical trial.
Methods
Research design
After securing Oakland University Institutional Review Board approval (# 912215) a prospective descriptive survey design study using older adults who had completed the HOP-UP-PT program was initiated.
Participant sampling
144 adults greater than or equal to 65 years of age were invited to enroll in the HOP-UP-PT program beginning in March 2019 as a component of a RCT. After completing the HOP-UP-PT program arm of that study, participants were reviewed for additional inclusion/exclusion (described later in the methods) to participate in a 3- and 6-month telephone questionnaire follow up which is the data described in this study.
The 144 HOP-UP-PT program participants were referred from representatives of community centers serving six Michigan communities: Auburn Hills, Novi, Pittsfield, Saline, St. Clair Shores, and VanBuren County-Paw Paw. HOP-UP-PT program inclusion criteria were as follows; 1) individuals greater than or equal to 65 years old, 2) at risk for decline in community dwelling status due to physical, socioeconomic, or community-related barriers, and 3) willingness to participate in a free home-based program provided by a licensed PT. Individuals were excluded from the study if; 1) they received PT services within the past two months at home, in a hospital, rehabilitation center, nursing home, or outpatient practice setting, 2) had been admitted to a hospital within prior two months, 3) were currently receiving palliative or hospice care, or 4) the initial evaluation by the licensed PT suggested that the person’s medical status would not permit safe PT interventions without further medical work up.
Upon completion of the program, older adults who participated in the HOP-UP-PT program between March 2019 and August 2020 were offered the opportunity to participate in a telephone questionnaire at two separate time intervals after program completion, 3- and 6- months. In addition to meeting initial eligibility criteria for participating in the HOP-UP-PT program, this follow-up questionnaire required participants to have completed seven of the nine program visits and not have disenrolled prior to completing the HOP-UP-PT program. Participants were excluded if initial contact was not successful after three telephone calls and did not respond to an email correspondence (if available). Support for the 144-participant sample size of the RCT is detailed elsewhere.Citation10 However, 94 (65%) of the 144 individuals enrolled in the RCT met the inclusion criteria for this arm of the study.
HOP-UP-PT program overview
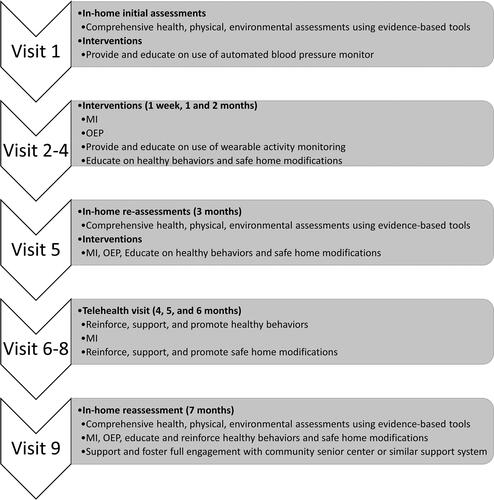
HOP-UP-PT program participation entailed six in-home visits and three telerehabilitation visits which were all conducted by licensed PTs. During program participation each older adult received a series of evidence-based health, physical, and environmental assessments to quantify their health and psychosocial status.Citation12 After these assessments, HOP-UP-PT participants received individualized programming aimed at facilitating positive health behaviors and reducing falls and fall risk. The older adult was provided with an automated blood pressure monitor (Omron HEM-712C Automatic Inflation Blood Pressure Monitor; Omron Corporation, Kyoto, Japan) and wearable activity tracker (Fitbit Alta; Fitbit, Inc, San Francisco, CA). Key program interventions included: 1) recommending home modifications identified during the HOME FAST assessment,Citation13 2) the Otago Exercise Program which has evidence of its use to reduce falls in older community dwelling older adults,Citation14 and 3) motivational interviewingCitation15 which is a counseling style aimed at eliciting positive health behavior change. An overview of the HOP-UP-PT programming including frequency, timing, and location of visits, assessments and interventions is provided in with a detailed outlined available in an open access publication by Arena et al.Citation10
Questionnaire instrument
The telephone questionnaire instrument used in this study was modified from a tool previously reported in a study by Wilson et al. 2020.Citation11 The questionnaire (Appendix A) includes 21-questions with four primary topic areas aimed at ascertaining post program experience related to 1) fall occurrence and outcomes (questions 1-3),Citation16 2) healthcare received after HOP-UP-PT participation (questions 4-6), 3) perceptions of HOP-UP-PT interventions and equipment (questions 7-16), and 4) perceptions of financial implications for HOP-UP-PT future use (questions 17-20). Question 21 was an open-ended question asking for general feedback regarding their opinion of the program.
The following modifications and additions were made to the questions comprising the original questionnaire described by Wilson et al. as was recommended by the original creators to enrich the face validity of the instrument:Citation111) modification to questions of fall occurrences and number of falls after completion of the HOP-UP-PT program, 2) addition of health care utilization after the HOP-UP-PT program, specifically inquiring about physical therapy and hospitalizations, 3) modification to questions of perceptions of equipment and interventions provided during HOP-UP-PT program, and 4) addition of questioning on respondents willingness to pay for and estimated participant contributions to the cost of the HOP-UP-PT program.
Procedures
Data collection was conducted by six investigators that were trained using a uniform interview script and questionnaire process (Appendix A). Additionally, a prior HOP-UP-PT participant who was not part of this potential participant pool served to simulate a questionnaire telephone call to validate uniformity of data collection among the investigators. Each of the six data collector was assigned to conduct the telephone surveys with HOP-UP-PT participants referred from one of the six participating community centers. Data collectors were informed by the principal investigator via email when a participant completed their last HOP-UP-PT program visit and the corresponding 3- and 6- month phone calls were scheduled if the participant consented. Telephone questionnaires were conducted from December 2019 until March 2021. Upon completion of the phone questionnaire, data was de-identified, coded, and entered on a spreadsheet.
Data analysis
Descriptive statistics were calculated to include measures of median age, as well as frequency counts and percentages for gender, age, and responses to all questions from the 3- and 6- month telephone questionnaires. For any missing data resulting from a respondent choosing to omit a response, data analysis was adjusted to exclude missing data in the frequency count. Statistical analysis was performed using Statistical Analysis Software version 9.4 for Windows (SAS Institute, Cary, North Carolina).
Results
Participant demographics
Ninety-four HOP-UP-PT program participants were contacted for potential inclusion. Of these, 76 (81%) provided responses to the 3-month survey and 71 (76%) responded to the 6-month survey. The mean age was 77 (SD = 7) years and 75% identified as a female. Although attempts to invite each prior HOP-UP-PT program participant meeting the inclusion criteria occurred, some individuals did not participate due to phone number disconnections, lack of availability, unwillingness to participate, not answering calls, and other unknown reasons.
Questionnaire outcomes
Fall occurrence and outcomes
When asked about fall occurrence, 12% (n = 9) of respondents reported 1-2 falls at the 3-month survey encounter, compared to the 6-month questionnaire at which 11.4% (n = 8) of respondents reported 1-2 falls, 2.9% (n = 2) reported 3-4 falls, and 1.4% (n = 1) reported having 5-6 falls. In other words, 15.5% of respondents reported a fall at 6-months. details these responses and the corresponding course of action reported by the respondent who responded affirmatively to a fall event. Of those reporting a fall, reasons included tripping over an obstacle, missing a step on a flight of stairs, falling while transitioning to standing from a seated position, and losing balance while standing on an unstable object such as a chair or a boat. Of those who sought medical attention, their reasons for doing so included a “jammed” finger, a dislocated shoulder, bruises, cuts that required stitches, and a fractured hip. Of the 84.5% of individuals that reported no falls in the 6-months after the program, respondents reported that they felt stronger, and they could go up and down stairs or stand up from a chair more easily.
Table 1. Fall frequency and reported medical actions.
Health care received after HOP-UP-PT intervention
In response to the question “Have you attended any type of physical therapy since the HOP-UP-PT Program Ended?” 16% (n = 13) responded yes at the 3-month questionnaire and 17% (n = 17) responded yes at the 6-month questionnaire. When asked “Have you been hospitalized since the study ended?” 3% (n = 2) and 6% (n = 4) responded yes at the 3- and 6- month questionnaires, respectively. In response to the question “Have you been in contact with or visited your local community or senior center since the study ended?” 57% (n = 45) and 45% (n = 32) responded yes at the 3- and 6-months questionnaires, respectively. It is notable that 13 of the 3-month telephone questionnaires were completed prior to the March 13, 2020, State of Michigan stay-at-home orders brought about by the COVID-19 pandemic with the remaining questionnaires completed after that statewide mandate was enacted. Therefore, senior community centers and physical therapy clinics, which were considered non-essential establishments, were closed. The authors recognize this may have impacted participant responses to some questions.
Perceptions of HOP-UP-PT interventions and equipment
outlines the responses from respondents regarding the benefits of the wearable activity monitor, automated blood pressure monitor, nutrition, and exercises. When asked if they experienced any issues with the Fitbit™ or wearable activity tracker, respondents noted that concerns which included battery malfunctions, lack of Wi-Fi, the screen being too small to accurately read the data, and spontaneous equipment shutoffs as barriers. Additionally, at 3-months and 6-months, 3% and 8% of respondents reported seeking a physician evaluation for a self-identified blood pressure issues with medication dosage adjustments and reduced salt consumption the recommended actions. Issues performing exercises were reported by 19% (3-months) and 22% (6-months) of respondents with barriers identified as incurring a recent injury, poor balance or balance exercise being too challenging, laziness, and lack of motivation and/or time. When respondents were asked how many times a week they exercised using the definition of “at least 30 minutes of moderate-intensity or 20 minutes of vigorous-intensity”, 32% (3-months) and 50% (6-months) responded with more than 4 times a week, 9% (3-months) and 17% (6-months) responded with 4 times a week, 17% (3-months) and 23% (6-months) responded with 3 times a week, 12% (3-months) and 13% (6-months) responded with twice a week, 4% (3-months) and 0% (6-months) responded with once a week, and 8% (3-months) and 14% (6-months) replied that they did not exercise at all during the week.
Table 2. Perceptions of benefit and continued adherence to program interventions.
Home safety modifications recommended by the PTs while enrolled in the program were completed after program completion by 29% (3-month) and 30% (6-month) of respondents. Examples of the reported modifications included removing rugs, cleaning clutter off the floor, utilizing night lights, and installing grab bars in the shower. Additionally, 20% (3-months) and 32% (6-months) of respondents reported being able to perform a new activity after program participation. Examples of new activities included walking longer distances, using stairs, standing up from a chair, and bending over to pick something up from the floor without losing balance.
Perceptions of financial implications for HOP-UP-PT
When asked about their willingness to pay for the HOP-UP-PT program, 65% and 72% of respondents indicated they would be willing to pay out of pocket to cover some expenses associated with the program at 3- and 6-months, respectively. Similarly, when asked about financial ability to cover the expenses of the program, 74% (3-months) and 69% (6-months) of respondents indicated they would be able to cover a portion of the program expenses. However, 95% (3-months) and 93% (n = 66) of the 6-month questionnaire respondents either agreed or strongly agreed that the HOP-UP-PT program should be covered by an insurer (i.e., Medicare) or another source (i.e., healthcare provider). details the responses to the question of an appropriate price point to pay out of pocket for the HOP-UP-PT program. It is notable that participants were not provided with the actual program cost which is estimated to be $1,500.
Table 3. Participants responses to appropriate price point for the HOP-UP-PT program.
Discussion
The purpose of this study was to describe the 3- and 6-month self-reported outcomes and perceptions of older adults who participated in a statewide HOP-UP-PT clinical trial. Positive trends were identified among HOP-UP-PT program participants at the follow-up surveys regarding fall occurrence and outcomes, healthcare received and community engagement following the program, perceptions of interventions and equipment, and financial outcomes that could have an impact on an older adult’s ability to age safely in place.
Fall occurrence and outcomes
The HOP-UP-PT program focuses on preventative factors related to fall risk such as balance, home safety, and blood pressure. As these factors may contribute to a fall, proactively addressing these issues within the scope of the program may have contributed to the decrease in fall rates as compared to the national average.Citation17 Specifically, Michigan adults over 65 years have reported annual fall rates of 28.8-39.9% ; whereas, only 16% of HOP-UP-PT participants reported falling during the six months after program participation.Citation18 When comparing the reported fall rates identified by this study’s respondents at 6-months after program completion to the fall rates reported prior to beginning the clinical trial (51.4% for the experimental group and 47.2% for the control group)Citation10 reduced fall occurrences during the 6-months after program completion are further supported. The outcomes and perceptions of this study suggest that by incorporating individualized balance exercises, optimizing the built environment toward reduced fall risks, and engaging in conversations about healthy lifestyles, long term fall efficacy may be positively impacted. It is further notable that HOP-UP-PT participants were referred from community-based senior centers to PTs instead of the more traditional medical or healthcare system-initiated referral mechanism. The positive outcomes of this study support the use of direct access referrals for preventative focused fall prevention programming to PTs.
Healthcare received and community engagement after HOP-UP-PT participation
When compared to the $28.9 billion dollars Medicare spent in 2015 on expenses for non-fatal falls, HOP-UP-PT programming could have a major impact on reducing cost savings to insurance companies and hospitals.Citation17,Citation19 Although not formally assessed in this study, it is plausible it was beneficial to the study participants to have some self-directed activities during the pandemic mandated stay-at-home orders which occurred in the latter half of the studies data collection phase. Due to the increased risk of severe disease and fear of contracting COVID-19 among older adults, there is a possibility that this study’s participants may have deferred healthcare services that would have normally required hospitalization prior to the pandemic. Additionally, temporary closure of many ambulatory care physical therapy clinics in Michigan may have also reduced the participants ability to seek care in these settings. Furthermore, while it is assumed most study participants were attending local community senior center at the onset of study participation, but less than half reported continued engagement, closure of community senior centers due to the COVID-19 pandemic may be a possible contributor to the decline in affirmative responses. However, further examination of these outcomes when there is confirmation of a COVID-19 endemic is warranted.
Perception of HOP-UP-PT interventions and equipment
Greater than half of respondents reported that the wearable activity monitor was beneficial. This was lower than expected when compared to the Wilson et al. study which reported 100% of the participants agreed and strongly agreed to the benefit of this device.Citation11 It is possibly that the lower percentage of respondents agreeing or strongly agreeing may be an outcome of technology issues including battery failure and inaccurate activity monitor readings identified by this studies respondents; thereby, contributing to a more unfavorable opinions regarding the equipment. Furthermore, respondents stated technological challenges as a factor to stopping use of the wearable activity tracker following the in-home visits.
More than three quarters of the survey respondents reported the automated blood pressure cuff to be beneficial. This was higher than the 72% reported during the Wilson et al. study.Citation11 Notably, respondents reported that, in collaboration with their physicians, abnormal blood pressure measures identified during in home monitoring resulted in treatable hypotension or hypertension diagnoses. The ease of use of this consumer-friendly assessment device and its vital importance in screening for abnormal blood pressure readings may contribute to its reported benefit among respondents.
Nearly three quarters of respondents reported that the exercises were beneficial, which is lower when compared to the 94% from the pilot study.Citation11 Additionally, respondent comment included gaining new skills including improved ability to walk longer distances, ascend and descend stairs, maintain balance during daily activities, and physical strength as a direct outcome of HOP-UP-PT program participation. These findings are significant when considering that fall risk factors include impaired activities of daily living, weakness, and balance deficits.Citation20 Mitigating declining in the aforementioned fall risk factors can result in a positive impact upon tasks required to live independently. Therefore, the HOP-UP-PT program could ultimately help seniors safely and successfully age in place. Rationale for the differences among the perceptions of benefit from the exercises between the pilot study results and current study results are unknown and will require further exploration.
Perceptions of financial implications for future implementation
While eligibility for insurance payment associated with the HOP-UP-PT program remains under investigation, the full program is estimated to be $1,500. This includes the professional fees, an automated blood pressure cuff, and a wearable activity monitor. The average cost of an older adult fall with an associated emergency room visit is greater than $2,900 and can exceed $38,000 if a hospitalization is required.Citation21
While most survey respondents reported a willingness to share in the program cost burden, the majority indicated a 10% contribution on their behalf was appropriate. Nearly all survey respondents indicated cost sharing with their medical insurer or provider would be an important aspect of this program moving forward. There is an established but underutilized mechanism within the framework of Medicare that may be utilized in billing for reimbursement of PT care provided in the home of non-homebound individuals. However, this mechanism reimburses as a rate adequate to cover overhead costs in an ambulatory care setting but does not account for travel costs and travel time costs required between visits in the home healthcare practice setting. Therefore, this reimbursement model is not sustainable for clinics and agencies to adopt as a viable care model and is therefore not routinely utilized.
According to Liang, Moore, and Soni, Medicare and Medicaid account for a majority of hospital costs per yearCitation21 and it is estimated that $50 billion is spent on non-fatal falls from adults 65 years and older and $754 billion on fatal falls in 2015.Citation22,Citation23 According to the CDC costs that are included in these estimates are, “fees for hospital and nursing home care, doctors and other professional services, rehabilitation, community-based services, use of medical equipment, prescription drugs, and insurance processing.”Citation5 Furthermore, Michigan rates as one of the costliest states for falls, spending upwards of $4 million per year on falls for older adults.Citation18 Given the significant growth trajectory of the population over 65 years, clinical gains brought about by programs such as HOP-UP-PT could result in substantial cost savings and reduce personal burden to older adults and their caregivers.
Study limitations
A limitation of this study includes not all prior participants could be interviewed due to the inability to reach the individuals by phone, respondent not being clear about what was being asked, and unclear or vague answers to some questions. Furthermore, as the respondents were aware the investigators were recording their responses, they may have altered responds to give a more positive impression of how they were doing/performing (i.e., the Hawthorne Effect).Citation24 Furthermore, selection bias may have occurred during recruitment as only participants who wished to participate provided their responses to the study. Finally, the survey did not include questions to garner data on the percentage of participants who continued to wear the Fitbit device or use the blood pressure monitor after the program ended; however, this but would be useful in future study iterations and design.
Future research
Future research should include a sample from a wider variety of geographical regions and with intentions toward examining needs of populations residing in varied climates, rural, suburban, and urban regions, and with varied socioeconomic levels to demonstrate generalizability of the outcomes of this study. Additionally, future research aimed at determining if individuals’ fall counts correlate with negative self-reported survey outcomes and examining healthcare utilization rates before, during, and after the HOP-UP-PT program is warranted to examine the program’s impact on cost as compared to age-matched peers. Furthermore, examination of annual health care costs for study participants during a period before and after the program would be of benefit. Finally, initiating the HOP-UP-PT program and then examining the program outcomes following a Medicare preventative health visit is warranted.
Conclusion
A PT-led, individualized, and prevention focused program delivered in the home of an older adult reduced fall occurrences and demonstrated sustained engagement with positive health behaviors and self-monitoring among those identified as at risk for physical decline or frailty. While older adults expressed satisfaction with the program and the associated outcomes, the amount they were willing and able to pay was approximately 10% of the actual program cost; therefore, exploration of insurer reimbursement is needed to support and sustain the positive outcomes brought about by preventative health programming in this population.
Supplemental Material
Download MS Word (16.9 KB)Acknowledgments
The authors thank Edward Peterson, PhD, Lori Boright, PT, DPT, DScPT, Rachel Shippy, SPT, Deb Colling, the participating Michigan Senior Centers, and the 2018 Michigan Health Endowment Fund -Healthy Aging Award.
Declaration of interests
Availability of data and materials
The deidentified individual participant datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Disclosure statement
SA and CW are co-principals of HOP-UP-PT, LLC. No financial transactions have occurred within HOP-UP-PT, LLC to date; however, there is a possibility for future fiscal viability thereby producing a potential financial conflict of interest. They declare no personal conflicts. VC, ME, LK and MS declare no financial or personal conflicts; however, did complete this work as students in the Doctor of Physical Therapy program at Oakland University.
Ethics approval and consent to participate
Human Subject Institutional Review Board Approval was obtained from Oakland University (# 912215). Written informed consent for study participation was obtained from all the participants in accordance with the tenets of the Declaration of Helsinki, and no stipend was provided.
Competing interests
The authors have no competing interests to declare.
Additional information
Funding
References
- Wick JY. Aging in place: our house is a very, very, very fine house. Consult Pharm. 2017;32(10):566–574. doi:10.4140/TCP.n.2017.566.
- Soriano TA, DeCherrie LV, Thomas DC. Falls in the community-dwelling older adult: a review for primary-care providers. Clin Interv Aging. 2007;2(4):545–553. doi:10.2147/CIA.S1080.
- Cise A, Cise AC, Lindquist L, Cameron K. Successful aging in place: seniors’ reflections and perspectives about what constitutes successful aging. J Am Med Directors Assoc. 2018;19(3):B30. doi:10.1016/j.jamda.2017.12.091.
- Centers for Disease Control and Prevention. Important facts about falls. https://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Published 2017. Accessed June 3, 2021.
- Centers for Disease Control and Prevention. Cost of older adult falls. https://www.cdc.gov/falls/data/fall-cost.html. Published 2020. Accessed March 4, 2021.
- Greenberg SA. Analysis of measurement tools of fear of falling for high-risk, community-dwelling older adults. Clin Nurs Res. 2012;21(1):113–130. doi:10.1177/1054773811433824.
- Musich S, Wang SS, Hawkins K, Yeh CS. Homebound older adults: prevalence, characteristics, health care utilization and quality of care. Geriatr Nurs. 2015;36(6):445–450. doi:10.1016/j.gerinurse.2015.06.013.
- Wilson CM, Arena SK, Adcock K, Colling D. A home-based older person upstreaming prevention physical therapy (HOP-UP-PT) program utilizing community partnership referrals. Home Healthc Now. 2019;37(2):88–96. doi:10.1097/NHH.0000000000000716.
- Arena SK, Wilson CM, Peterson E. Targeted population health utilizing direct referral to home-based older person upstreaming prevention physical therapy from a community-based senior center. Cardiopulm Phys Ther J. 2020;31(1):11–21. doi:10.1097/CPT.0000000000000131.
- Arena SK, Wilson CM, Boright L, Peterson E. Impact of the HOP-UP-PT program on older adults at risk to fall: a randomized controlled trial. BMC Geriatr. 2021;21(1):520. doi:10.1186/s12877-021-02450-0.
- Wilson C, Arena SK, Starceski R, Swanson K . Older adults’ outcomes and perceptions after participating in the HOP-UP-PT program: a prospective descriptive study. Home Healthc Now. 2020;38(2):86–91. doi:10.1097/NHH.0000000000000843.
- STEADI: Algorithm for FallRisk Screening, Assessment, and Intervention. Center for Disease Control and Prevention. https://www.cdc.gov/steadi/materials.html. Published 2017. Accessed January 28, 2019.
- Mackenzie L, Byles J, Higginbotham N. Reliability of the Home Falls and Accidents Screening Tool (HOME FAST) for identifying older people at increased risk of falls. Disabil Rehabil. 2002;24(5):266–274. doi:10.1080/09638280110087089.
- Campbell AR. Otago Exercise Program to Prevent Falls in Older Adults. Otago Medical School, University of Otago. https://www.livestronger.org.nz/assets/Uploads/acc1162-otago-exercise-manual.pdf. Accessed January 25, 2021.
- Pignataro RM, Huddleston J. The use of motivational interviewing in physical therapy education and practice: empowering patients through effective self-management. J Phys Ther Educ. 2015;29(2):62–71. doi:10.1097/00001416-201529020-00009.
- Kathryn D. Roby and Charlotte Steniger Qualidigm. Introduction to OASIS-D. Centers for Medicare and Medicaid Services. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HomeHealthQualityInits/Downloads/August_2018_HH_QRP_Overview_of_Changes_to_OASIS-D_without_answers.pdf
- Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical costs of fatal and nonfatal falls in older adults. J Am Geriatr Soc. 2018;66(4):693–698. doi:10.1111/jgs.15304.
- Centers for Disease Control and Prevention. Older Adult Falls Reported by State. https://www.cdc.gov/falls/data/falls-by-state.html. Published 2020. Accessed December 5, 2021.
- Center for Disease Control and Prevention. Preventing Falls: A Guide to Implementing Effective Community-Based Fall Prevention Programs. 2nd ed. National Center for Injury Prevention and Control. https://www.cdc.gov/homeandrecreationalsafety/pdf/falls/FallPreventionGuide-2015-a.pdf. Published 2015. Accessed February 6, 2021.
- Kamel HK, Vamc CJZ. Falls’ guidelines and osteoporosis assessment. J Am Geriatr Soc. 2002;50(6):1167–1168. doi:10.1046/j.1532-5415.2002.502831.x.
- Liang L, Moore B, Soni A. National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2017: Statistical Brief #261; 2006. http://www.ncbi.nlm.nih.gov/pubmed/32833416.
- Haddad YK, Bergen G, Florence CS. Estimating the economic burden related to older adult falls by state. J Public Health Manag Pract. 2019;25(2):E17–E24. doi:10.1097/PHH.0000000000000816.
- Centers for Disease Control and Prevention. WISQARSTM — Web-based Injury Statistics Query and Reporting System. https://www.cdc.gov/injury/wisqars/index.html. Published 2020. Accessed February 6, 2021.
- McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: New concepts are needed to study research participation effects. J Clin Epidemiol. 2014;67(3):267–277. doi:10.1016/j.jclinepi.2013.08.015.