ABSTRACT
As COVID-19 converges with loneliness and addiction epidemics in the US, both public health and mental health experts forecast dramatic increases in substance use and mental health conditions. This cross-sectional study evaluated relationships of loneliness with depression, anxiety, alcohol use, and drug use during COVID-19, and assessed perceived increases in these symptoms in young adults. Between April 22 and May 11, 2020, 1,008 participants ages 18–35 were recruited through social media to a one-time, online anonymous survey. Symptomatology was assessed using six scales. Perceived changes since COVID-19 were evaluated using 5-point Likert scales. Forty-nine percent of respondents reported loneliness scores above 50; 80% reported significant depressive symptoms; 61% reported moderate to severe anxiety; 30% disclosed harmful levels of drinking. While only 22% of the population reported using drugs, 38% reported severe drug use. Loneliness was associated with higher levels of mental health symptomatology. Participants reported significant increases across mental health and substance use symptoms since COVID-19. While direct impacts of COVID-19 could only be calculated with pre-pandemic assessments of these symptoms, estimates indicate elevated psychosocial symptomatology and suggest that symptoms could have worsened since the pandemic. Findings underscore the importance of prevention and intervention to address these public health problems.
Introduction
On March 11, 2020 the World Health Organization declared the novel SARS COV2 (COVID-19) a global pandemic, and by April 11, 2020 the US had the most confirmed cases and deaths in the world. This domestic public health crisis is heightened by the collision of the COVID-19 pandemic with the addiction (Volkow Citation2020) and loneliness (Cacioppo and Cacioppo Citation2018; Murthy Citation2017) epidemics that have affected the US for the past years. Public health practitioners and mental health experts (Galea, Merchant, and Lurie Citation2020; Holmes et al. Citation2020; Ornell et al. Citation2020; Panchal et al. Citation2020; Rehm et al. Citation2020) have raised concerns about the potential effects of COVID-19 and anticipated repercussions of social restrictions on wellbeing and mental health disorders, predicting increases in loneliness, anxiety, depression, and substance use.
Even before imposed COVID-19 social restrictions, loneliness had been gaining attention as a public health crisis. Distinct from objective social isolation and solitude, loneliness is the feeling of lacking needed social connections (Hawkley and Cacioppo Citation2010), and has been associated with depression, suicidality, substance abuse (Lamis, Ballard, and Patel Citation2014), and cognitive decline, as well as overall health and mortality (Hawkley and Cacioppo Citation2010). Despite their widespread use of social platforms, young adults comprise the group with highest prevalence of loneliness (Cigna International Citation2018; Hawkley and Cacioppo Citation2010; Murthy Citation2017), drawing attention to the need for preventive interventions and an active repositioning of the nation’s social trajectory in order to mitigate increasing social disconnection.
In the face of global concern about the mental health effects of COVID-19, specifically in adolescents and young adults (Fegert et al. Citation2020), few studies have sought to document and characterize loneliness and mental health wellbeing and problems in the young adult population. To date, only anxiety, post-traumatic stress disorder, and depression have been documented among college students in China and the US (Cao et al. Citation2020; Chang, Yuan, and Wang Citation2020; Huckins et al. Citation2020). Recent reports on loneliness during COVID-19 have yielded controversial results, and differences between subpopulations evaluated (Killgore et al. Citation2020; Luchetti et al. Citation2020; Sutin, Luchetti, and Terracciano Citation2020). Consequently, the prevalence and potential worsening of loneliness, substance abuse, and other mental health symptoms in young adults remain important to assess, especially while bracing for an anticipated post-COVID “social recession” (Gabbatt Citation2020). This study assessed levels of loneliness, anxiety, depression, and alcohol and drug use during the COVID-19 pandemic in a sample of young adults across the United States (US), and examined associations between loneliness and these mental health conditions.
Methods
Study sample
This cross-sectional study used a web-based survey to capture loneliness and psychosocial symptomatology in young adults during COVID-19. Between April 22 and May 11, 2020, 1,008 participants were recruited through postings on social media and networking sites (Instagram, Facebook, LinkedIn, and Twitter) via an anonymous link to the Qualtrics (Qualtrics Citation2020) survey. The link was also distributed to US colleges and universities through standard newsletters or student association Facebook pages. Eligibility included being 18– 35 years of age and residing in the US. Participant consent was obtained electronically prior to beginning the survey. Median survey completion time was 16 minutes, and participants received a 20 USD eGift card. This study was approved by the University of Miami Institutional Review Board, and all data were collected and maintained on Qualtrics and stored on a Box secure server. Several features ensured that the survey was not being completed by a bot, such as the use of Completely Automatic Public Turing test to tell Computers and Humans Apart (CAPTCHA) prior to submitting the survey responses and prior to requesting compensation.
Measures
The 126-item survey assessed mental health symptomatology and other behaviors and covariates using validated measures. Demographic questions included age, gender, highest level of education, number of people living in the household, and city and state of residence at the time of the assessment.
Loneliness was assessed using the UCLA Loneliness Scale (version 3) (Russell, Peplau, and Cutrona Citation1980), a 20 item self-report questionnaire that evaluates subjective feelings of loneliness and social isolation. Participants rated items on a 4-point Likert scale ranging from 1 (never) to 4 (often). Items were summed to create a score ranging from 20 to 80, with higher scores being indicative of greater loneliness. The internal consistency of the UCLA in this sample was acceptable (Cronbach’s alpha = 0.81).
Substance use behaviors were evaluated using the Alcohol Use Disorder Identification Test (AUDIT) and the Drug Abuse Screening Test (DAST-10). The AUDIT is a 10-item self-report questionnaire developed by the World Health Organization to identify individuals whose alcohol consumption could be hazardous for their health (Saunders et al. Citation1993). Participants rated items on a 5-point Likert scale, indicating amount (0 to 10 drinks or more), frequency (never to daily or almost daily), and indication of problems caused by alcohol (yes or no). Items were summed to create a score ranging from 0 to 40. A score of 1–7 indicates low-risk consumption, 8–15 suggests risky or hazardous drinking, and a score of more than 15 is likely to indicate high-risk drinking and alcohol dependence. The internal consistency of AUDIT in this sample was good (Cronbach’s alpha = 0.91). The DAST-10 is a self-report screening test that provides a quantitative index of the degree of consequences related to drug abuse (Skinner Citation1982). Participants rated items yes or no, with positive responses corresponding to 1 point. Items were summed to create a score ranging from 0 to 10. A score of 1–2 represents low-level problems related to drugs, 3–5 represents moderate problems, 6–8 represents substantial problems, and 9–10 represents severe problems. The Cronbach’s alpha in this sample was 0.92.
Anxiety and Depression were assessed using the Generalized Anxiety Disorder (GAD-7) Questionnaire and the Center for Epidemiologic Studies Depression scale (CES-D-10). The GAD-7 is a 7-item self-report screening tool that assesses presence and severity of Generalized Anxiety Disorder (Spitzer et al. Citation2006). Participants rated frequency of problems on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). Items were summed to create a score, with scores of 5, 10, and 15 being the cutoff points for mild, moderate, and severe anxiety, respectively. The Cronbach’s alpha in this sample was 0.80. The CES-D-10 is a 10-item self-report measure that assesses the frequency of symptoms of depression (Andresen et al. Citation1994). Participants rated frequency of symptoms on a 4-point scale from 0 (rare or none of the time) to 3 (most or almost all the time). Items were summed to create a score from 0 to 30, with higher scores representing greater depressive symptoms. A score of 10 or more indicates the presence of significant depressive symptoms. The internal consistency of CES-D in this sample was acceptable (Cronbach’s alpha = 0.75).
Several covariates were also measured. Social connectedness was assessed using the revised, and further extracted, Social Connectedness Scale (SC-15), a 15 item self-report measure that assesses individuals’ sense of social belonging (Lee, Draper, and Lee Citation2001). Participants responded on a 6-point Likert scale on 5 positive and 10 negative items regarding their sense of social belonging from 1 (strongly disagree) to 6 (strongly agree). Items were summed to create a score from 20 to 120, with higher scores reflecting stronger sense of social connectedness. The internal consistency of SC-15 in this sample was acceptable (Cronbach’s alpha = 0.80).
Other environmental and personal factors that may affect psychosocial symptoms and behaviors were also assessed, including living situation, enrollment in school, and education level. We also asked for self-report practices of communication via technology, assessing the method (phone, internet, social media), level (monthly, weekly, daily, hourly, or all the time), and intent of use (for work, for disengaged personal use, or to connect with friends).
To capture a pre-post indication as to the degree of change of behaviors and symptoms, one question following each scale asking participants to compare pre-COVID experiences and behaviors to experiences and behaviors since COVID-19 was declared a pandemic on March 11, 2020 using a Likert scale indicating that symptoms decreased a lot, decreased slightly, remained the same, increased slightly, or increased a lot. To mitigate feelings of discomfort in disclosing certain feelings or symptoms, each item provided an option of “prefer not to answer.”
Monte Carlo simulations using MPlus (Muthén and Muthén Citation2018) revealed a sample as small as n = 155 would have 90% power to uncover a standardized coefficient of.25, a small to moderate effect.
Analysis
All participants who completed the survey were included in analyses. Percentages and frequencies were computed for each scale variable and covariates. As every item required a response to complete the survey, missing data was in the form of “prefer not to answer” selected as an option. To conservatively manage this, responses to scales were included if at least half of their scale items were disclosed, giving a value of the mean of available items if they were marked as “prefer not to answer.” Missing data was less than 1% of the sample for all items except for gender and school status. For these items, the first survey rollout missed them, and we immediately amended it to include them. These responses resulted in 29% of these variables missing. Because the missing data was not based on participant decision, we considered them as missing at random.
To assess the relationship between levels of loneliness and other symptoms and behaviors, Pearson correlation coefficients were calculated between UCLA score and other indicators. To characterize relationships in pre-COVID and post-COVID behaviors and psychosocial symptomatology, correlation coefficients were again calculated for reported changes in feelings of loneliness and changes in other feelings, behaviors, and symptoms. The reported changes in feeling loneliness were further examined to assess coinciding changes in other behaviors and symptoms.
Analyses were conducted on all scales as continuous variables as well as by categories of clinical significance. Differences in the mean scores for each of the scales were assessed using ANOVA and T-tests across each of the demographic variables and by categorical score increments. These analyses were performed using SAS University Edition (SAS Citation2015), and two-tailed p-values less than 0.05 were considered significant.
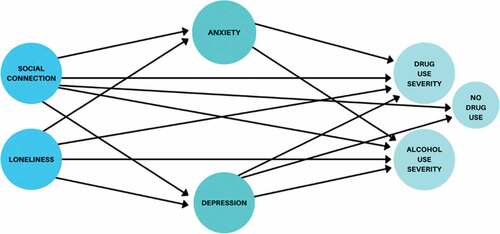
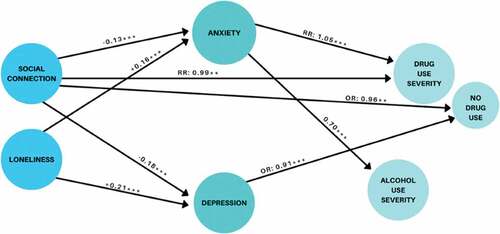
To evaluate how loneliness and social connectedness are related to our outcomes (anxiety, depression, alcohol use, drug use), a path model with proposed directional effects () was created using structural equation modeling in Mplus. This model included direct effects of both loneliness and social connectedness on depression, anxiety, alcohol use, and drug use as well as indirect effects of loneliness and social connectedness on alcohol and drug use working through anxiety and depression. Additional control variables in this model for the four outcomes were employment loss, age, gender, ethnicity and race (Black, Hispanic), education, number in household, and social connectedness. The DAST scale was modeled as a Poisson distributed count variable with zero inflation. To include all participants, even when some data were missing, the expectations-maximization algorithm was used in Mplus. Tests of mediation are made using delta-method standard errors on the products of the two pathways making up each of the indirect effects (MacKinnon Citation2008) between both loneliness and social connectedness and alcohol and drug use through both anxiety and depression. To examine potential reciprocal effects, additional models also examined reversed effects of alcohol and drug use effects on anxiety and depression. Akaike’s Information Criteria (AIC) was used to compare model fit (Akaike Citation1974). Models with lower values of the AIC indicate better fit of that model to the data than models with higher AIC.
Results
Demographic characteristics of the respondents and mean sum scores for UCLA, AUDIT, DAST, CES-D, GAD, and SC-15 can be found in . The median age of respondents was 28 years (IQR 26–31) with 86% of the population being above 23 years. Fifty-one percent of the population reported being males (292 responses missing), and 91% not enrolled in school (296 responses missing). Most of the respondents were white (76%), followed by blacks (10%), and 24% reported being Hispanic. Most respondents (63%) were living with 2 or 3 people at the time of the survey.
Table 1. Sample demographic characteristics and mean scores by category
The mean score on the UCLA Loneliness Scale was 49.54 (SD 7.9), with 49% of the population reporting scores above 50 (see ). The mean score for the AUDIT was 9.36 (SD 7.9). Most respondents (80%) reported drinking alcohol, with 30% reporting AUDIT scores above 16, revealing harmful and dependent levels of drinking. Nineteen percent of respondents reported binge drinking at least weekly and 44% reported binging at least monthly. The mean DAST-10 score was 1.04 (SD 2.3), with 22% of the sample reporting drug use, and 38% of the users scoring above 5, indicating substantial and severe drug use. The mean score for the GAD-7 was 10.44 (SD 4.4), and 62% of the sample reported scores of 10 or above, revealing moderate (45%) and severe (17%) anxiety (Spitzer et al. Citation2006). Mean score for the CES-D was 13.69 (SD 5.1), with 79% scoring 10 or above, indicating the presence of “significant depressive symptoms” (Andresen et al. Citation1994). The mean score for the SC-15 was 53.55 (SD 9.9), with 65% falling within the middle quintile. Pearson correlation coefficients revealed associations between the UCLA Loneliness Scale and the AUDIT (correlation coefficient of 0.20, p< .0001), the DAST-10 (correlation coefficient of 0.14, p< .0001), the GAD-7 (correlation coefficient of 0.47, p <.0001), the CES-D (correlation coefficient of 0.55, p <.0001), and the SC-15 (correlation coefficient of −0.71, p <.0001). Detailed scores by scoring category are presented in .
Table 2. Score frequencies, scale correlations, and mean sum score by category
Many participants reported that their feelings of loneliness (65%), alcohol use (48%), drug use (44%), anxiety (62%), and depression (64%) had increased, while experiencing a decrease in feelings of connectedness (53%), since COVID-19 was declared a pandemic. This is despite reported increases of media and technology usage, wherein 56% said their usage increased during COVID-19. Furthermore, reported level of change in loneliness was associated with changes in alcohol use (correlation coefficient of 0.07, p< .05), anxiety (correlation coefficient of 0.38, p< .0001), depression (correlation coefficient of 0.32, p< .0001), and feelings of connectedness (correlation coefficient of −0.06, p< .05). Most participants reporting an increase in feelings of loneliness also indicated an increase in drinking (58%), drug use (56%), anxiety (76%), and depression (78%), and a decrease in feelings of connectedness (58%).
Structural equation modeling revealed that loneliness and social connectedness were each directly related to both anxiety (UCLA score β:0.16, p < .0001, SC-15 score β = −0.13, p < .0001) and depression (UCLA score β: 0.21, SC-15 score β = −0.18, p < .0001), and anxiety is directly related to both alcohol use severity (GAD-7 score β: 0.70, p < .0001) and drug use severity (GAD-7 score β: 0.05, p < .0001) (see and supplemental figure). There were significant indirect effects of both loneliness (positive) and social connectedness (negative) working through anxiety on both alcohol and drug use severity. There was an indirect effect of loneliness on DAST-zero inflation, leading to less chance of zero-inflation (i.e., more likely to use drugs). Alternative models evaluating the effects of alcohol and drug use on anxiety and depression revealed worse fit than our first proposed model (AIC (Alcohol & Drugs → Anxiety & Depression) = 35,246.1, AIC (Anxiety & Depression → Alcohol & Drugs) = 35,217.6).
Discussion
This study documents elevated levels of loneliness, depression, anxiety, alcohol use, and drug use among young adults during COVID-19. An alarming 49% of respondents reported a great degree of loneliness with scores of above 50 (with a mean score of 49.93 for 18–25-year-olds and 48.22 for 26–34-year-olds). Almost 80% reported significant depressive symptoms, and 61% reported moderate (45%) to severe (17%) anxiety. Participants disclosed harmful or dependent levels of drinking (30%), with 44% reporting binge drinking at least monthly. And while only 22% of the sample reported using drugs, 38% of users reported severe drug use. These results reveal heightened levels compared to previously documented prevalence of loneliness (mean scores of 48.87 for 18–25-year-olds and 44.92 for 26–34-year-olds on the UCLA Loneliness Scale) (Bruce et al. Citation2019), anxiety (6.2% reporting scores of some type of anxiety disorder) (Kessler et al. Citation2012), and depression (7.7% of adults with depression) (Brody, Pratt, and Hughes Citation2018). Comparisons with Monitoring the Future data also reveal higher prevalence in alcohol use (29.3% reporting use in the past month) and binge drinking (25% college-age students and non-students reporting binge drinking) (Schulenberg et al. Citation2019). Participants reported significant decreases in social connectedness and significant increases in loneliness and across their substance use and mental health symptoms since COVID-19. It is possible that social restrictions imposed during COVID-19 have affected young adult social connectedness, and may have affected levels of loneliness, substance use, and mental health symptoms.
This study documents levels of loneliness, anxiety, depression, and alcohol and drug use, and confirms associations occurring between the symptoms, which may also be seen in pre-pandemic times, and by further evaluating their relationship with the use of clinical measures. This study serves in identifying maladaptive symptoms and possibly disorders among young adults being hit hard by the restrictions put in place to control the novel Coronavirus. The study captures well-defined co-occurrence of several clinical symptoms and behaviors among US young adults, during a short window of the nationwide stay-at-home ordinance.
This study met several methodological limitations. First, cross-sectional data precludes inference of cause-effect relationships. Structural equations models, however, do hypothesize directionality of relationships. We did assess one alternative where causality ran from substance use to mental health (anxiety and depression), which did not fit the data as well as our hypothesized model where directionality ran from mental health to substance use. Nevertheless, there are likely reciprocal relationships among these variables that only longitudinal data could uncover. Second, pre-post self-reported symptoms may be biased by social desirability and by lack of recall on participant state prior to COVID-19. Third, comparisons with studies of pre-pandemic symptomatology meet limitations in comparable samples, instrumentation, and reporting due to the epidemiologic nature of available studies, and only offer a glimpse of how prevalence of clinically significant thresholds may be different than before COVID-19 began. Fourth, missing data on gender and school enrollment decrease reliability of associations of these variables with observed results. However, missingness did not involve the individual and occurred at random. Finally, though our sample includes individuals from every continental US state and captures a wide scope of age, race, ethnicity, household, income, and education across the young adult range, the information is not entirely generalizable. For example, whites (76%) and those with a degree (49% Bachelors; 10% Masters) were overrepresented as compared to the general population. Generalizability is further impeded as internet recruitment may be pulling from a sample seeking online connection and thus lonelier than the average young adult.
The mental health consequences of COVID-19 and a call for prevention and early intervention have been highlighted previously, including predictions of a global mental health catastrophe with exacerbated symptoms among the vulnerable (Izaguirre-Torres and Siche Citation2020). The current study confirms the need for this call to action, a necessary step to reduce the burden of disease and the state of mental health during COVID-19, especially in the context of an already fragile mental health system in the US (Auerbach and Miller Citation2020). Findings reiterate the demand for attention to the loneliness epidemic in the US (Murthy Citation2017) and underscore the importance of prevention and intervention on young adults. Several strategies have been described to address loneliness, such as social support and connectedness, and include the importance of correcting maladaptive social cognition. Evidence-based interventions involving mindfulness have been described as having a role in enhancing resiliency and promoting physical, emotional, and social wellbeing. International studies have emphasized the importance of responding to collegiate students via sustaining online delivery of coursework, increasing counseling services, and deploying outreach through telehealth services. For young adults not engaged in school, aggressive patient outreach by primary care physicians should be used to ensure screening and intervention, also via telehealth. Access to psychological help coupled with the development and dissemination of brief online contact-based interventions that encourage healthy lifestyles (e.g., physical exercise, balanced diet) are important (Amsalem, Dixon, and Neria Citation2020). Empowering self-support groups and sustained engagement with updated, reliable information about the outbreak is necessary. Social prescribing, which draws from and promotes usage of community resources, also shows promise of improving social and psychological wellbeing. This could be positioned to then encourage service to others, bringing social comfort and reward as a result of connecting with others in need. These efforts and others can help to alleviate the problems of loneliness and its manifestations; yet it may take an integrated, multi-faceted, and concerted approach, rooted, and supported by mental health prevention and wellbeing promotion (Campion et al. Citation2020), boosted by workforce development and research on intervention development, to readdress these trajectories.
The convergence of the COVID-19 pandemic and the loneliness and addiction epidemics in the US is here to stay. Addressing mental health and substance use problems in young adults, both during and after the COVID-19 pandemic, is an imperative. These young adults are the future of our nation’s social fabric, and as we invest in developing the sense of cohesion and social connectedness in these generations, we can address social and physical resiliency in our communities at large.
Contributors
VEH and RDS conceived the study and secured funding for this project. VEH supervised as RDS executed survey creation and dissemination. RDS completed data extraction process. VEH screened and selected relevant studies, and all authors critically appraised included studies. DJF and RDS completed data analysis. DJF created and tested statistical models. VEH drafted the first version of the manuscript and RDS created the figures and tables. All authors interpreted the findings and edited, finalized, and approved of the final version of the manuscript.
Study registration
ClinicalTrials.gov #NCT044440098.
Supplemental Material
Download MS Word (134.9 KB)Acknowledgments
We thank John Reynolds for his assistance in the systematic literature search. We want to thank the Biostatistics Collaborating Consulting Core, funded by the BERD program of the Miami Clinical and Translational Sciences Institute (CTSI 2.0 NIH Award No (UL1TR002736)), for its support in sample size and power calculations.
Disclosure statement
All authors declare no competing interests.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website.
Additional information
Funding
References
- Akaike, H. 1974. A new look at the statistical model identification. IEEE Transactions on Automatic Control 19 (6):716–23. doi:10.1109/TAC.1974.1100705.
- Amsalem, D., L. B. Dixon, and Y. Neria. 2020. The coronavirus disease 2019 (COVID-19) outbreak and mental health: Current risks and recommended actions. Journal of the American Medical Association Psychiatry. doi:10.1001/jamapsychiatry.2020.1730.
- Andresen, E. M., J. A. Malmgren, W. B. Carter, and D. L. Patrick. 1994. Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine 10 (2):77–84. doi:10.1016/S0749-3797(18)30622-6.
- Auerbach, J., and B. F. Miller. 2020. COVID-19 exposes the cracks in our already fragile mental health system. American Journal of Public Health 110 (7):969–70. doi:10.2105/AJPH.2020.305699.
- Brody, D. J., L. A. Pratt, and J. P. Hughes. 2018. Prevalence of depression among adults aged 20 and over: United States, 2013–2016. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Accessed June 24, 2020. https://www.cdc.gov/nchs/data/databriefs/db303.pdf.
- Bruce, L. D., J. S. Wu, S. L. Lustig, D. W. Russell, and D. A. Nemecek. 2019. Loneliness in the United States: A 2018 national panel survey of demographic, structural, cognitive, and behavioral characteristics. American Journal of Health Promotion 33 (8):1123–33. doi:10.1177/0890117119856551.
- Cacioppo, J. T., and S. Cacioppo. 2018. The growing problem of loneliness. The Lancet 391 (10119):426. doi:10.1016/S0140-6736(18)30142-9.
- Campion, J., A. Javed, N. Sartorius, and M. Marmot. 2020. Addressing the public mental health challenge of COVID-19. The Lancet Psychiatry 7 (8):657–59. doi:10.1016/S2215-0366(20)30240-6.
- Cao, W., Z. Fang, G. Hou, M. Han, X. Xu, J. Dong, and J. Zheng. 2020. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research 287:112934. doi:10.1016/j.psychres.2020.112934.
- Chang, J., Y. Yuan, and D. Wang. 2020. Mental health status and its influencing factors among college students during the epidemic of COVID-19. Nan fang yi ke da xue xue bao= Journal of Southern Medical University 40 (2):171–76. doi:10.12122/j.1673-4254.2020.02.06.
- Cigna International. 2018. Cigna U.S. loneliness index. Accessed June 18, 2020. https://www.cigna.com/static/www-cigna-com/docs/about-us/newsroom/studies-and-reports/combatting-loneliness/loneliness-survey-2018-full-report.pdf.
- Fegert, J. M., B. Vitiello, P. L. Plener, and V. Clemens. 2020. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health 14:1–1. doi:10.1186/s13034-020-00329-3.
- Gabbatt, A. 2020. ‘Social recession’: How isolation can affect physical and mental health. The Guardian, March 18. Accessed September 18, 2020. https://www.theguardian.com/world/2020/mar/18/coronavirus-isolation-social-recession-physical-mental-health.
- Galea, S., R. M. Merchant, and N. Lurie. 2020. The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. Journal of the American Medical Association Internal Medicine 180 (6):817–18. doi:10.1001/jamainternmed.2020.1562.
- Hawkley, L. C., and J. T. Cacioppo. 2010. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine 40 (2):218–27. doi:10.1007/s12160-010-9210-8.
- Holmes, E. A., R. C. O’Connor, V. H. Perry, I. Tracey, S. Wessely, L. Arseneault, C. Ballard, H. Christensen, R. C. Silver, I. Everall, et al. 2020. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry 7 (6):547–60. doi:10.1016/S2215-0366(20)30168-1.
- Huckins, J. F., A. W. DaSilva, W. Wang, E. Hedlund, C. Rogers, S. K. Nepal, J. Wu, M. Obuchi, E. I. Murphy, M. L. Meyer, et al. 2020. Mental health and behavior of college students during the early phases of the COVID-19 pandemic: Longitudinal smartphone and ecological momentary assessment study. Journal of Medical Internet Research 22 (6):e20185. doi:10.2196/20185.
- Izaguirre-Torres, D., and R. Siche. 2020. Covid-19 disease will cause a global catastrophe in terms of mental health: A hypothesis. Medical Hypotheses 143:109846. doi:10.1016/j.mehy.2020.109846.
- Kessler, R. C., M. Petukhova, N. A. Sampson, A. M. Zaslavsky, and H. U. Wittchen. 2012. Twelve‐month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatry Research 21 (3):169–84. doi:10.1002/mpr.1359.
- Killgore, W. D., S. A. Cloonen, E. C. Taylor, and N. S. Dailey. 2020. Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Research 290:113117. doi:10.1016/j.psychres.2020.113117.
- Lamis, D. A., E. D. Ballard, and A. B. Patel. 2014. Loneliness and suicidal ideation in drug‐using college students. Suicide and Life-Threatening Behavior 44 (6):629–40. doi:10.1111/sltb.12095.
- Lee, R. M., M. Draper, and S. Lee. 2001. Social connectedness, dysfunctional interpersonal behaviors, and psychological distress: Testing a mediator model. Journal of Counseling Psychology 48 (3):310. doi:10.1037/0022-0167.48.3.310.
- Luchetti, M., J. H. Lee, D. Aschwanden, A. Sesker, J. E. Strickhouser, A. Terracciano, and A. R. Sutin. 2020. The trajectory of loneliness in response to COVID-19. American Psychologist 75 (7):897–908. doi:10.1037/amp0000690.
- MacKinnon, D. P. 2008. Introduction to statistical mediation analysis. Routledge.
- Murthy, V. 2017. Work and the loneliness epidemic. Harvard Business Review. Accessed June 21, 2020. https://hbr.org/cover-story/2017/09/work-and-the-loneliness-epidemic.
- Muthén, . K., and B. Muthén. 2018. Mplus. The comprehensive modelling program for applied researchers: User’s guide.
- Ornell, F., H. F. Moura, J. N. Scherer, F. Pechansky, F. Kessler, and L. von Diemen. 2020. The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Research 289:113096. doi:10.1016/j.psychres.2020.113096.
- Panchal, N., R. Kamal, K. Orgera, C. Cox, R. Garfield, L. Hamel, C. Muñana, and P. Chidambaram. 2020. The implications of COVID-19 for mental health and substance use. Kaiser Family Foundation. Accessed June 18, 2020. https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/.
- Qualtrics. 2020. Qualtrics development company. Provo, UT. Retrieved from: https://www.qualtrics.com
- Rehm, J., C. Kilian, C. Ferreira‐Borges, D. Jernigan, M. Monteiro, C. D. Parry, Z. M. Sanchez, and J. Manthey. 2020. Alcohol use in times of the COVID 19: Implications for monitoring and policy. Drug and Alcohol Review 39 (4):301–04. doi:10.1111/dar.13074.
- Russell, D., L. A. Peplau, and C. E. Cutrona. 1980. The revised UCLA loneliness scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology 39 (3):472–80. doi:10.1037//0022-3514.39.3.472.
- SAS. 2015. SAS/IML® 14.1 user’s guide. Cary, NC: SAS Institute Inc.
- Saunders, J. B., O. G. Aasland, T. F. Babor, J. R. De la Fuente, and M. Grant. 1993. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption‐II. Addiction 88 (6):791–804. doi:10.1111/j.1360-0443.1993.tb02093.x.
- Schulenberg, J., L. Johnston, P. O’Malley, J. Bachman, R. Miech, and M. Patrick. 2019. Monitoring the future national survey results on drug use, 1975–2018: Volume II, college students and adults ages 19–60. Accessed June 25, 2020. http://monitoringthefuture.org/pubs.html#monographs.
- Skinner, H. A. 1982. The drug abuse screening test. Addictive Behaviors 7 (4):363–71. doi:10.1016/0306-4603(82)90005-3.
- Spitzer, R. L., K. Kroenke, J. B. W. Williams, and B. Löwe. 2006. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine 166 (10):1092–97. doi:10.1001/archinte.166.10.1092.
- Sutin, A. R., M. Luchetti, and A. Terracciano. 2020. Has loneliness increased during COVID-19? Comment on “Loneliness: A signature mental health concern in the era of COVID-19”. Psychiatry Research 291:113295. doi:10.1016/j.psychres.2020.113295.
- Volkow, N. D. 2020. Collision of the COVID-19 and addiction epidemics. Annals of Internal Medicine 173 (1):61–62. doi:10.7326/M20-1212.