Abstract
Objective: A validated measure to gather patient feedback on physicians’ empathy is not available in Swedish. The objective for this study was to examine the psychometric characteristics of a Swedish version of the Consultation and Relational Empathy (CARE) measure (widely used in English).
Design, setting and patients: The CARE measure was translated into Swedish and tested on 554 unselected patients visiting physicians in two primary care clinics in northwestern Stockholm, Sweden.
Main outcome measures: Adequate translation, as well as reliability and validity of the Swedish CARE measure.
Results: The Swedish CARE measure seemed to demonstrate high acceptability and face validity when consulting a physician. The mean CARE score 41.5 (SD 8.9) over all 10 item was not significantly influenced by seasonality, age or gender. Scores were somewhat negatively distributed, but corrected item-total correlations were high (0.86–0.91) suggesting homogeneity. Internal reliability was very high (Cronbach’s alpha 0.975). Factor analysis implied a one-dimensional structure with factor loadings between 0.89 and 0.93.
Conclusions: The Swedish CARE measure appears to be psychometrically valid and reliable enough in physicians.
Introduction
Empathy is considered to be a fundamental component in all therapeutic relationships [Citation1], and is regarded as a crucial aspect of the patients' perception of the quality of care [Citation2]. An empathic approach has been linked with better clinical outcomes and more efficient care [Citation3,Citation4].
Health authorities increasingly demand the implementation of a patient-centered approach [Citation5]. There is a need of instruments that adequately provide information and give feedback to clinicians to enable them to improve and develop their skills. According to Epstein et al. [Citation6], patient-centered care has six aspects that can be measured: (1) fostering healing relationship; (2) exchanging information; (3) responding to emotions; (4) managing uncertainty; (5) making decisions; and (6) enabling self-management. These aspects are congruent with the concept of clinical empathy, as reported by Stepien and Bearnstien [Citation7]. According to them, clinical empathy is composed of four different components: (1) emotive, the ability to imagine patients’ emotions and perspectives; (2) moral, the physician’s internal motivation to empathize; (3) cognitive, the intellectual ability to identify and understand patients’ feelings and perspectives; and (4) behavioral, the ability to communicate understanding of those emotions and perspectives back to the patient. However, using the term ‘components’ might be misleading, as empathy also could be described as the totality of the experience in a consultation setting, which should be kept in mind when interpreting the construct validity of measurement instruments [Citation8]. There are some existing scales that are used for patient evaluation of a broad range of specific aspects of general practice care, e.g. the EUROPEP instrument [Citation9]. The Consultation and Relational Empathy measure (CARE) at issue here is designed to more specific measure the relational skills of the caregiver, from the patient’s point of view, avoiding judging any instrumental skills [Citation10]. Of an unselected group of primary care patients (n = 3044) in a large performance study of the CARE measure 76% have endorsed the scale as very relevant in association to the consultation experience [Citation10]. The scale is well implemented and widely used for appraisal, revalidation and audit of general practitioners in the UK [Citation11,Citation12]. It has also been validated and translated into various languages and is being used by researchers in Europe, US, Canada, China and Japan [Citation13–18]. The CARE measure has also shown predictive validity in terms of patient outcomes [Citation19,Citation20].
There is a lack of an individual feedback instrument regarding relational empathy in Swedish, hence, the aim of this study was to translate the CARE measure into Swedish and to study its psychometric characteristics in a Swedish primary health care setting, and also to study if there where any differences in answer pattern due to age, gender or season.
Material and methods
Study design and participants
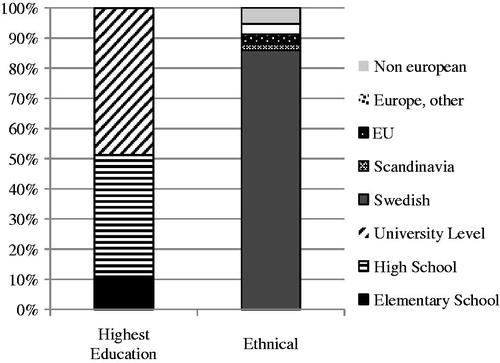
Study participants were recruited from two public service general practices in northwestern Stockholm, located within 3.5 kilometers from one another in residential neighborhoods, comprising patients with similar socioeconomic background and ethnical composition (). The directors agreed to let their practices be part of the study.
Figure 1. Demographic data. It refers to the population of the communities predominantly served by the two practices. Statistics regard 2012. (http://www.tmr.sll.se/Global/Dokument/Statistik/planprognoser/0123%20J%c3%a4rf%c3%a4lla.pdf and http://www.statistikomstockholm.se/index.php/omradesfaktax/).
In September 2013, 342 out of 1626 visitors (21.0%) and in December the same year, 212 out of 1720 visitors (12.3%) answered the CARE measure which was 16.6% of all the visits. In total, (both practices combined) 20 specialists, 6 residents and 1 internal physician were working at that time.
Information about the study was posted on the walls and in the reception areas. All patients that came to the practices were asked to complete an anonymous and non-compulsory survey after their visit, irrespective of which caregiver they had met. The surveys were distributed by the receptionist or laboratory personnel to the patients, as they registered their arrival to the practice.
The surveys were collected in a locked mailbox at the exit.
Inclusion and exclusion criteria
The survey was only offered in Swedish, hence the patient needed to be able to read and understand Swedish. Accompaniers of children, either unwilling or unable to read and write, were allowed to answer for the child, how the accompanier perceived the consultation. Exclusion criteria: non-Swedish speaking, adult illiteracy and incomplete survey.
Description of the CARE measure
The CARE measure was originally developed by Dr. Stewart Mercer et al. at the Departments of General Practice in Glasgow University and Edinburgh University [Citation21]. The scale comprises 10 questions measuring empathy in the setting of the therapeutic rapport during a one-on-one consultation between a clinician and a patient (). The scoring system for each item uses a 5 point Likert Scale ranging from ‘poor’ to ‘excellent’, generating values between 1 and 5. There is also a choice ‘does not apply’. The scale developers allow up to two ‘does not apply’ responses or missing values, and recommend replacing these values with the average score for the remaining items, a mean-item score. A questionnaire with more than two missing or non-applicable responses is to be excluded from analysis. The scale score ranges from 10 to 50 [Citation10,Citation21].
Table 1. Questions in the CARE measure.
Translation of the CARE measure
The translation of the scale was conducted according to Streiner and Norman [Citation22]. Two different bilingual (Swedish/English) persons with Swedish as a mother tongue translated the scale to Swedish. The translations were then back-translated into English by two other bilingual persons with English as a mother tongue, who were not familiar with of the original CARE measure or its purpose. An analysis group has compared the original and the two back-translated scales, aiming at eliminating any differences between the separate versions. This first draft of the Swedish version was tested with a pilot group of 11 persons in different age categories (17–88 years of age, mean age 50.36 ± 24.10), sex (7 women and 5 men), and with different nationalities (7 Swedish, 1 Czech, 1 Spanish, 1 Finnish and 1 Iraqi), all Swedish speaking. All persons were interviewed regarding the choice of language and comprehension of the different items in the scale. A few comments implied that the questions were excessively lengthy and complicated, with too many variations in the explanatory descriptions under each item. The majority, however, found the questionnaire generally easy to understand. Based on their feedback minor wording modifications were made. This final draft (see Supplementary material) was retested again on 5 Swedish speaking persons (2 Swedish, 1 Iraqi, 1 Spanish and 1 Italian) not finding any more adjustments to be made.
Statistical considerations
Data analysis: validity and reliability
We analysed the scale using a similar approach with classical test theory that was used when the original scale and other translations of the scale were tested for validity and reliability [Citation11,Citation13,Citation14,Citation21,Citation23]. It is recommended that sample size exceed a minimum of 400 subjects to able reliability studies [Citation16] and the minimum of 200 subjects to able a reliable factor analysis [Citation13]. IBM SPSS statistics version 22 was used for the statistical analyses of Cronbach’s alpha and to perform factor analysis. STATA 12.1 and SPSS 22.0 were used to supply descriptive data.
Acceptability and face validity
Mercer et al. [Citation10], Mercer and Murphy [Citation21], Fung et al. [Citation13] and Aomatsu et al. [Citation14] have examined the patients’ endorsement of the scale and demonstrated that patients find the content of very high importance regarding the consultation experience – findings well-correlated with the relatively low amount of ‘non-applicable’ (NA) or missing (M) answers. The option ‘Does not apply’ may be marked when finding the item irrelevant to the consultation; thus low amounts of NA/M answers represent the fact that the patients find the item relevant. The acceptability and face validity of the Swedish CARE measure was hence assessed by the number of non-applicable or missing scores (NA/M) for each of the 10 items ().
Reliability and internal consistency
Cronbach’s α was computed to assess internal reliability and to determine whether removal of any of the 10 items affected the consistency (). An alpha in the range of 0.70–0.90 indicates acceptable to good internal consistency [Citation22]. An alpha higher than 0.90 indicates redundancy, that several questions ask the same thing but in slightly different ways. Homogeneity was examined by corrected item-total correlations, where a value above 0.20 is seen as a predictor of high correlation [Citation22]. Exploratory factor analysis was performed to examine the structure of correlations among the measured variables to identify underlying latent constructs (i.e. factors, ).
Results
Collected questionnaires
A total of 554 questionnaires were collected during two weeks in September and two weeks in December 2013 in both practices, representing around 16.6% of all visits and covered patients between 2 and 93 years (mean 54.8 SD (20.0), 65.9% female, 34.1% male. Overall, 31.9% (177/554) of the questionnaires were incomplete (). In spite of this, our sample size was about the recommended number which requirements for reliability studies (n = 400) [Citation23] and factor analysis (n = 200) [Citation24].
Table 2. Descriptive data on response pattern. Responses on the 10 items in the Swedish Consultation and Relational Empathy (CARE) measure in the study participants (n = 554). The table displays, for each item, the number and proportion of study participants who scored respective response option (Poor, Fair, Good, Very Good and Excellent), the number and proportion of study participants who had data ‘Not applicable’ and ‘Missing’. The table also displays the Total number of study participants per item.
Table 3. Frequency for number of participants with incomplete records in 1–10 items by reason, i.e. missing data and not applicable.
Table 4. Reliability, homogeneity and factor loadings for the Swedish CARE measure (≤2 M/NA variables).
Acceptability and face validity
High acceptability and face validity was indirectly implied at least in this self-selected population as the majority of respondents answered all or at least 8 out of 10 items ().
Performance of the CARE measure
Summary scores ranged from 10 to 50, and mean from 1 to 5, with negatively distributed data, see . Overall, somewhat 40% to 50% scored the maximum score for almost all items, demonstrating a ceiling effect. The frequency of endorsement for each item was skewed towards the three highest ratings (good, very good and excellent) for each item. An increase of scores at even numbers 30, 40 and 50 reflects a well-known bias of rating scales known as the halo effect, implying that items are rapidly rated on the basis of a global impression rather than paying attention to the individual item, thus reducing the accuracy of the measurement [Citation22].
Computing the mean CARE score for the mean over all items within the questionnaires gave a mean of 41.5 (SD 8.9). The scale demonstrated similar performance when tested during different seasons (September: 42.0 (8.5) compared to December: 40.8 (9.3), p = .13). Neither age (not shown) nor gender (men: 40.6 (9.5), women: 42.0 (8.5) p = .08) influenced the results in a significant way.
Internal reliability, homogeneity and factor analysis
Corrected item-total correlations were high (0.86–0.91) suggesting prominent homogeneity. Internal reliability was very high (Cronbach’s alpha 0.975) and slightly reduced when eliminating any of the items. Factor analysis implied a one-dimensional structure with factor loadings between 0.88 and 0.93 ().
Discussion
We have translated the CARE measure into Swedish and carried out a pilot study to examine its psychometric characteristics in a primary care setting in Sweden, demonstrating similar performance-data as the original scale and earlier translations [Citation10,Citation13,Citation14].
We can assume that the patients who answered the CARE measure, found it to be relevant when consulting a physician, by the low amount of non-applicable/missing (NA/M) responses for items 1–8, indirectly reflecting a high acceptability and face validity, at least in this self selected population. One limitation of the study is that the sample may not have been representative of the practice population, given the rather low response rate. The most likely reason for the low response rates is that the reception staff stopped handing out the measure when they got busy.
Our results are similar to earlier work when rating physicians on the scale (beside the low response rate, as earlier studies have had response rates of 70%) [Citation10,Citation13,Citation14,Citation23], however, our study did not demand the patients to rate the questions in grade of relevance, which may be considered a weakness. We would also like to bring to mind some important aspects of empathy that are not totally covered by patient-rated experience measures, e.g. the interactive empathic process between patient and caregiver. Here videoing consultations could be an alternative, but such approach is quite time-consuming and not easily integrated into routine care. However, the CARE measure was developed based on a widely accepted definition of relational empathy, and its contents co-produced with patients and practitioners, before being validated against the gold standards of the time [Citation10,Citation21], and correlates well with objectively measured aspects of patient-centeredness [Citation25].
The mean value for encounters with physicians (41.66 ± 8.48) is very similar to the mean (40.8 ± 8.8) obtained in performance data regarding the original scale [Citation10]. A pronounced negative skewness with a distinct ceiling effect, likewise found in earlier work [Citation10,Citation23] and the obvious halo effects around even scores limit the informative value of the measure. A strong negative skew is commonly found when rating other people [Citation22], so that the average individual is rated well above average, negatively influencing the precision of the measure.
The amount of NA/M answers is very low for items 1–3 and 5–8 ranging between 0.2 and 2.2%. There is a larger amount of NA/M answers for question 4 (Being interested in you as a whole person…) (7.2%), and especially 9 (Helping you take control…) (18.6%) and 10 (Making a plan of action with you…) (19.9%), in line with earlier work [Citation5,Citation21,Citation22]. Excluding question 9 and 10, only around 2% of the answers are found to be NA/M in our sample, congruent with Mercer et al.’s findings [Citation10].
The reasons for the high amount of NA/M answers for items 9 and 10 are unclear. The outcomes may reflect an avoidance of addressing the subject and hence poor caregiver skills. Our material shows similar results to earlier work [Citation10,Citation13,Citation14], regarding internal consistency with very high values for Cronbach’s alpha in our sample, alongside very high inter-item correlations. These values may represent redundancy in the choice of items. In combination with the comments on iteration and complicated wording, this poses the question of possible item-reduction without losing any content validity. Wirtz et al. [Citation15] by using Rasch analysis have demonstrated that item 10 contains abundant information, and is not indicative of the otherwise one-dimensional construct of the CARE scale. They speculate that item 10 rather reflects shared decision making, instead of physician empathy and propose to leave out item 10 when investigating relational empathy in research purposes. There are other studies that are in line with Wirtz et al.’s [Citation15] Rasch analysis. Kersten et al. [Citation26] show that a large part of variance (82%) was explained by the first factor (fit to the Rasch model). Still, the ‘low-response’ items are important to investigate further, related to clinical settings.
Our factor analysis supports the unidimensionality of the scale, and also item 9 and 10 loaded a bit surprisingly clearly into one major factor. The high inter-item correlation values achieved in this material might mirror the fact that our study population is rather homogenous, and studies need to be pursued in different socioeconomic settings. Supporting the reliability of the scale, we find no significant impact on the scale when administering it on different occasions and seasons.
Limitations: One limitation of the current study is the selection of study population. Including primary health care centers from rural areas, and from different regions of Sweden would have been preferable. Another limitation is that other variables such as socioeconomic status where not included in the questionnaire, but would have been useful. In e.g. Mercer et al. [Citation10], a wide-range of additional variables were collected which allowed a much fuller description of the sample and the relationship with the CARE measure scores.
Future directions
Larger studies are warranted to establish reference values appropriate in Swedish settings, and to determine if the scale can be used to measure the impact of interventions aiming at improving physician empathy. It would also be valuable to analyze unidimensionality and redundancy in the Swedish CARE scale with item response theory methods, such as Rasch analysis.
Conclusion
We have established a Swedish version of the CARE Measure and tested it in a primary care setting in an urban area in Sweden. The CARE measure appears to be valid and reliable in our sample and has an overall performance that mirrors the original scale. Further studies including more diverse populations and in depth psychometric analysis are warranted.
Notes on contributors
Karin Crosta Ahlforn is a GP at Täby Centrum Doktorn and affiliated to the Center for Social Sustainability, Karolinska Institutet, Stockholm, Sweden.
Eva Bojner Horwitz, PhD, PhT, and Reg DMT, is a researcher at the Department of Public Health and Caring Sciences, Uppsala University, and at the Department of Clinical Neuroscience and at Center for Social Sustainability, both Karolinska Institute, Stockholm Sweden.
Walter Osika, MD, PhD is associate professor at the Department of Clinical Neuroscience, Karolinska Institutet and at the Center for Social Sustainability, Karolinska Institute, Stockholm Sweden.
IPRI_Osika_et_al_Supplemental_Content.docx
Download MS Word (13.9 KB)Acknowledgements
Ethical approval was obtained for the study (Dnr 2013/941-31/4 Central Ethical Review Board in Stockholm, Sweden). The authors thank the staff at Barkarby and Spånga general care practices for enabling the data collection and Dr. Alberto Crosta and Dr. Jan Kowalski for providing excellent help with statistical analysis.
Disclosure statement
No potential conflict of interest was reported by the authors.
Funding
Ekhaga Foundation, The Knight Yard Clinic.
References
- Reynolds WJ, Scott B. Empathy: a crucial component of the helping relationship. J Psychiatr Ment Health Nurs. 1999;5:363–370.
- Mercer SW, Reynolds WJ. Empathy and quality of care. Br J Gen Pract. 2002;52:9–13.
- Rakel D, Barrett B, Zhang Z, et al. Perception of empathy in the therapeutic encounter: effects on the common cold. Patient Educ Couns. 2011;85:390–397.
- Di Blasi Z, Harkness E, Ernst E, et al. Influence of context effects on health outcomes: a systematic review. Lancet. 2001;10:757–762.
- The Swedish Agency for Health and Care Services Analysis; [cited 2014 March 10]. http://www.vardanalys.se.
- Epstein RM, Fiscella K, Lesser CS, et al. Why the nation needs a policy push on patient-centered health care. Health Affairs (Millwood). 2010;8:1489–1495.
- Stepien KA, Baernstein A. Educating for empathy. A review. J Gen Intern Med. 2006;21:524–530.
- Rudebeck CE. The doctor, the patient and the body. Scand J Prim Health Care. 2000;18:4–8.
- Wensing M, Vedstedt P, Kersnik J, et al. Patient satisfaction with availability of general practice: an international comparison. Int J Qual Health Care. 2002;14:111–118.
- Mercer SW, McConnachie A, Maxwell M, et al. Relevance and practical use of the Consultation and Relational Empathy (CARE) Measure in general practice. Fam Pract. 2005;22:328–334.
- Murphy DJ, Bruce DA, Mercer SW, et al. The reliability of workplace-based assessment in postgraduate medical education and training: a national evaluation in general practice in the United Kingdom. Adv in Health Sci Educ. 2009;14:219–232.
- The CARE Measure web site. Nursing, Midwifery and Allied Health Professions Research Unit; [cited 2014 May 25]. http://www.caremeasure.org.
- Fung CSC, Hua A, Tam L, et al. Reliability and validity of the Chinese version of the CARE measure in a primary care setting in Hong Kong. Fam Pract. 2009;26:398–406.
- Aomatsu M, Abe H, Abe K, et al. Validity and reliability of the Japanese version of the CARE measure in a general medicine outpatient setting. Fam Pract. 2014;1:118–126.
- Wirtz M, Boecker M, Forkmann T, et al. Evaluation of the ‘‘Consultation and Relational Empathy’’ (CARE) measure by means of Rasch-analysis at the example of cancer patients. Patient Educ Couns. 2011;82:298–306.
- Neumann M, Wirtz M, Bollschweiler E, et al. Determinants and patient-reported long-term outcomes of physician empathy in oncology: a structural equation modelling approach. Patient Educ Couns. 2007;69: 69–75.
- Fung C, Mercer SW. A qualitative study of patients' views on quality of primary care consultations in Hong Kong and comparison with the UK CARE measure. BMC Fam Pract. 2009;10:10
- Mercer SW, Fung C, Chan F, et al. The Chinese-version of the CARE measure reliably differentiates between doctors in primary care: a cross-sectional study in Hong Kong. BMC Fam Pract. 2011.
- Mercer SW, Jani B, Wong SY, et al. Patient enablement requires physician empathy: a cross-sectional study of general. Practice consultations in areas of high and low socioeconomic deprivation in Scotland. BMC Fam Pract. 2012;13:6.
- Mercer SW, Higgins M, Bikker AM, et al. General practitioners’ empathy and health outcome: prospective observational study of consultations in areas of high and low deprivation. Ann Fam Med. 2016;14:117–124.
- Mercer SW, Maxwell M, Heaney D, et al. The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy based consultation process measure. Fam Pract. 2004;21:699–705.
- Streiner DL, Norman GR. Health measurement scales: a practical guide to their development and use. 4th ed. New York (NY): Oxford University Press; 2008.
- Mercer SW, Murphy DJ. Validity and reliability of the CARE measure in secondary care. Clin Gov Int J. 2008;13:269–283.
- Fabrigar LR, Wegener DT. Exploratory factor analysis. New York (NY): Oxford University Press; 2012.
- Lundy JM, Bikker A, Higgins M, et al. General practitioners’ patient-centredness and responses to patients’ emotional cues and concerns: relationships with perceived empathy in areas of high and low socioeconomic deprivation. J Compassion Health Care 2015;2:2.
- Kersten P, White PJ, Tennant A. The consultation and relational empathy measure: an investigation of its scaling structure. Disabil Rehabil. 2012;34:503–509.
