Abstract
Objective: To explore how general practitioners (GPs) think and act when presented with new evidence in relation to planned home birth and a proposal to change information practices.
Design: Exploratory ethnographic study of GPs. The GPs were encountered one or more times during a two-year period, 2011–2013, while the author tried to set up formal focus group interviews. Dialogues about the evidence, personal experiences, values and other issues unavoidably occurred. Field notes were written concomitantly.
Setting: Danish GPs, primarily in Copenhagen.
Subjects: Fifty Danish GPs.
Results: The GPs reacted very differently, both spontaneously and later. Spontaneous reactions were often emotional involving private and professional experiences whereas later reactions were more influenced by rational deliberations. Approximately half the GPs (n = 18) who were asked whether they would personally hand out the local information leaflet about home birth were prepared to do so. The time lag between presentation of the evidence and the GPs’ decision to hand out the leaflets was up to one and a half year.
Conclusions: A significant number of GPs were prepared to change their information practices. However, for many GPs, the new evidence challenged previous perceptions, and ample time and resources for dialogue, deliberations and adaptation to local circumstances were required to accommodate change.
Implications: Changing information practices on a larger scale will require a systematic approach involving key stakeholders.
Current awareness•Patients and pregnant women should receive evidence-based information about possible choices of care – also in relation to place of birth.
Most important results•Doctors often find the new evidence supporting planned home birth counterintuitive and spontaneously react emotionally rather than rationally to the evidence.•The new evidence challenging previous views elicits fast, emotional reactions, later deliberate reflections, perhaps cognitive dissonance and, finally, for some, change in clinical practice.
Significance for the readers•The findings may be applicable to other fields where an evidence-based choice between an interventionist and a conservative approach is relevant.
Key Points
Introduction
Conflicts between the best available evidence and current clinical practice are not uncommon and even targeted information does not necessarily lead to changes in practice [Citation1–3]. It has been recommended to study the process of dissemination of evidence in more detail using qualitative methods [Citation1,Citation3]. In a recent systematic review of diffusion of innovation and evidence into practice the authors bemoaned that ‘most studies examine only a few barriers, and questions are primarily closed questions’ [Citation4]. In line with this the authors of a more recent narrative review of ‘knowledge translation’ recommended ‘research designs such as ethnograpy’ [Citation5]. And in a study that specifically reviewed ‘the literature describing and quantifying time lags in the health research translation process’ the authors concluded that ‘little is known about time lags’ and deplored that ‘much of the complexity […] are hidden in this preference for “averages”’. [Citation6]
An opportunity to study the process of dissemination of evidence in more detail using qualitative methods was offered by the increasingly stronger evidence in relation to home versus hospital birth when the updated Cochrane review on the topic was published [Citation7]. According to the review, planned home birth for low-risk women can be as safe as planned hospital birth, with fewer interventions and complications. The review concludes in the implication for practice section that ‘all countries should consider establishing home birth services with collaborative medical back up and offer low-risk pregnant women information about the available evidence and the possible choices’ [Citation7]. The conclusion is in line with the recently published NICE guidelines and a statement issued jointly by ‘The International Confederation of Midwives’ and the ‘International Federation of Gynaecology and Obstetrics’ [Citation8,9]. In the Danish clinical setting, the first pregnancy visit is with the GP; planned home birth and hospital birth are both options that are free of charge within the public health care system; and in both places midwives are the primary care givers [Citation10]. However, strong anecdotal evidence from women considering home birth suggests that few general practitioners tell pregnant women about the home birth option even though place of birth should be discussed at the first pregnancy visit [Citation10]. In a recent Canadian survey, family physicians similarly ‘reported discomfort with discussing home birth with their patients’ [Citation11].
In the implication for research section, the Cochrane review concludes that ‘it might be worthwhile to use qualitative methods to investigate how clinicians who advice women about place of birth think about home birth in relation to the evidence’ [Citation7]. The aim of this paper is to describe the first steps in this process using an open exploratory ethnographic method without using closed questions or focusing on preselected barriers.
Material and methods
Access to the field
This is an exploratory ethnographic field study that developed in an iterative manner. It is the first in a series of more structured qualitative studies with audio-recorded dialogues with individual GPs, audio-recorded teaching sessions of GPs in training, and other recorded sessions. Many of the findings have been presented along the way, internationally at the last three Nordic Congresses for General Practice and a WONCA meeting, and nationally at various scientific meetings in Danish.
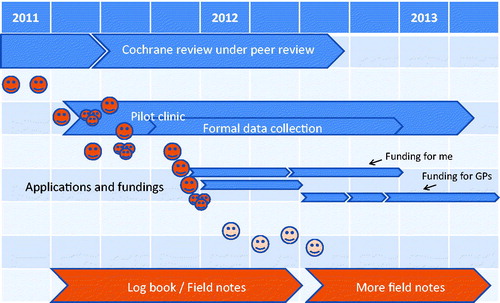
My access to the field, the community of Danish GPs, in relation to the timing of the publication of the evidence is illustrated in . Following initial contact to a couple of key GPs I knew from previous work, I was led to a GP who was currently head of a primary care clinic. I asked if she thought her partner GPs might be willing to participate and in the early summer 2011, I was invited to present my ideas at a meeting in the clinic. The meeting took place in September when the Cochrane Review [Citation7] was in production but not yet published. I summarized the state of the evidence, as it was presented in the review and subsequently mailed an html version of the review to the clinic. At the meeting, I handed out (a) a list of contraindications to home birth with the conditions in bold (mostly chronic diseases) that GPs should be looking for, (b) copies of the newly produced small home birth information leaflet for pregnant women considering home birth from the Royal hospital (which also acts as ‘local’ hospital in the area serviced by the clinic), and (c) copies of a draft one-page data collection sheet for the GPs to fill in after each first pregnancy consultation to document the information process and whether or not the home birth leaflet was handed out – in case they decided to join my project. A decision as to whether the GPs wanted to participate or not was not made at the meeting and I did not set up a deadline. Incidentally, I encountered some of the involved GPs in the House of General Practice at the Center of Health and Society, University of Copenhagen and had shorter or longer conversations with them. Following internal discussions, the clinic collectively decided to join the project and gradually started up. During the process, I got some first impressions of how GPs might react and I used these experiences from my collaboration with this pilot clinic in my application for funding to carry out the first of the above mentioned series of more structured qualitative studies (currently under revision for another journal) with the aim to investigate (i) what GPs ‘think about home birth in relation to the evidence [italics added]’ [Citation7] and (ii) whether they are prepared to act based on the new evidence in the sense that they would agree to inform pregnant women about home birth as an option. As I spoke with still more GPs, I decided to keep a logbook to keep track of names, events, comments, promises and decisions. Quickly the logbook turned into a sort of field notes.
Figure 1. Time line for field work and key events. The upper arrows indicate formal events: preparation, peer review and publication of updated Cochrane review; establishment of collaboration with a pilot clinic; and applications for funding. The darker faces indicate individual encounters with GPs (or groups of GPs) until submission of the first application; after submission, the number of encounters increased appreciably. The pale faces indicate discussions with qualitative researchers about getting access to do research in general practice. The arrows at the bottom indicate a project log book that transformed into a collection of field notes.
During that process, I presented my project ideas to a snowballing list of GPs, mainly key GPs with various relations to research, quality development, pre-, postgraduate and continuous medical education related to the House of General Practice; I also presented my ideas to a few GPs without any such roles. Most of the GPs happened to have very immediate comments, proposals and opinions. I received a lot of input that I recorded as field notes in my log book. Each field note had three entries: (a) date and event (e.g. someone’s anniversary reception, a planned meeting on another topic, an informal lunch conversation); (b) full names of those I had an interaction with, (c) the informative parts of the dialogue written down as closely as I could remember it. Most of the entries were written within 1–3 days.
Colleagues at the research unit who had previously carried out qualitative studies in general practice confirmed that it was a challenge to get access to the field and one researcher suggested to seize any opportunity for an encounter with GPs and forget about pre-planned sampling of specific GPs from specific areas or any expectation about well-planned, audio-taped interviews in quiet meeting rooms. This approach is supported by Adele Clarke who in her textbook on qualitative research states: ‘other approaches are always already available and may also be provocative and interesting’ [Citation12]. Thus, in addition to fully certified GPs working in central Copenhagen, also GPs from other regions, GPs in their last year of training and one very young ‘prospect’ have been interviewed or have in other ways provided input.
Material
The observations [Citation13], the partly structured dialogues, documents in the form of e-mail exchanges, transcribed audio recorded ‘re-enactments’ of conversations and extensions of particularly informative encounters form the main part of the data material presented in this paper. The following figures indicate the size of the material: By summer 2013, the field notes (excluding e-mails) constituted 58 pages of text, had approximately recorded 200 entries (sometimes involving more than one named GP, occasionally involved GPs that were active in research rather than in clinical practice, obstetricians, midwives and sometimes meetings with only GPs or mixed audiences). Eighteen of the encountered GPs had started informing their pregnant patients and handing out the leaflet, fewer had explicitly refused or excused. Five GPs had participated in prepared and structured, individual, audio-taped interviews one or more times in addition to one medical student immediately after her training at an obstetrical department in her last month of medical education as well as almost 20 GPs participating in three audio-taped meetings (four GPs at a meeting in their clinic; around a dozen GPs in their local guild, and two GPs who had voiced their very opposing views at a very brief public session at an arranged follow-up meeting), in total resulting in 47 pages of transcript.
Preconception and analytical strategy
My preconception, based on many years of employment in the Cochrane Collaboration and according to my application for funding, was that evidence does not sell itself and that even targeted information does not necessarily lead to changes in practice [Citation2,3]. The idea was that action research and a participatory dialogue process [Citation14] in the style of academic detailing might lead to changes [Citation15]. Based on the above-mentioned material, a pool of text was created for analysis. The audio-recorded events were transcribed verbatim by the author, the non-recorded encounters memorized and the most relevant parts of the dialogues in the encounters written down as verbatim as possible; finally informative parts of e-mail exchanges were extracted. All text was treated in the same way inspired by systematic text condensation [Citation16] and situational analysis. [Citation12] An overall impression of ‘how clinicians think’ was obtained during the field work, during the transcription process and while reading each chunk of text. Meaning units representing different aspects of the informants’ comments on the topic were identified and coded in the text. Coded groups were subsequently condensed. To guard against selectivity in the use of data, the most important observations have been presented directly to some of the informants along the way and at scientific meetings open to all informants. Standard computer programs for text editing were used during the process; text was printed out, marked with various colours, notes and headings, copied and pasted into new documents, and reorganized several times.
Research ethics
This type of research does not require institutional ethical approval in Denmark. All audio recorded informants were informed that (i) they could regret at any time, (ii) that I would delete the recorded conversation immediately if they did so, and (iii) that their input would be anonymized if published. Some of the informants that provided useful input through e-mail were similarly asked for permission to be quoted anonymously. One informant withdrew an already given consent. The retraction was accepted and the input not used. [Citation17]
Results
The collected data showed that GPs reacted very differently to the presented evidence and my proposal to consider a change in what information was given to pregnant women. Below the reactions are grouped into (i) spontaneous reactions that were often emotional involving private and professional experiences and (ii) reflective reactions that were influenced by rational deliberations.
Spontaneous reactions
‘Blood and drama’
The most dramatic type of reaction often occurred as soon as the word ‘homebirth’ was mentioned and before any details of the project or the evidence had been presented. GPs with these reactions gave very explicit and detailed descriptions of births in which there was severe bleeding; mothers were dramatically transferred from birthing rooms to operational theaters; and several babies were close to death:
GP1: The mother just continued to bleed and all of a sudden it went really fast; more than 1.5 l at no time. It had been contained in the uterus. Everything had been normal; a third time mother, two previous births without any problems. And then it happened. Apparently some residual placenta with an artery; that just continued to bleed like hell. It took 12-16 hours, a shift, and just over 20 liters of blood before they gave up and drove [from the local hospital] to [the more specialized] hospital because it simply could not be stopped. It had bled so heavily right from the beginning that we had to provide both blood and plasma within the first half hour. And half an hour is a long time. She had lost more than half of her blood volume, almost (sic!)
The dramas mostly originated in the GPs’ specialist training in hospitals and obstetric departments but a few involved babies who were transferred from home birth. Often the story was told with a loud and very dramatic tone of voice. These GPs believed that it could not in any way be safe or even ‘sane’ to plan a home birth.
Asking for more details
In contrast, a more welcoming type of spontaneous reaction was from GPs who invited me to give more details about the project and the evidence:
Me: Have you had time to read the material that I sent?
GP2: Yes, I have read the application quickly.
Me: Any questions?
GP2: Yes, can it be correct that the women are comparable in the home and hospital groups?
Me: (… I give my long standard explanation …).
GP2: [seems skeptical of the credibility of my claim but then suddenly (and surprisingly) states]: I have heard many of the arguments because one of my friends is a midwife who is very fond of home birth.
And a little later:
GP2: But what about fetal monitoring? Do midwives simply use this (GP shows a wooden Pinard stethoscope)? Doctors just love to add some technology! Are midwives able to do continuous electronic fetal heart rate monitoring at home?
GPs who asked for more information often held various leadership roles in the Danish GP community but not always.
Personal history
Some GPs had personally considered home birth as an option with one saying confidentially:
GP3: I actually wanted to give birth at home to my second child but my husband was too afraid; but that is of course a long time ago.
Order of reactions in groups
On the few occasions where the exchanges took place in larger groups, it was always the most dramatic reactions that were voiced first and these were often followed by additional dramatic stories. Only if time allowed did more moderate participants give voice to their view towards the end of these spontaneous or otherwise time-limited gatherings.
Reflective reactions
Reflective comments happened after I had presented the evidence and answered questions which took 10–30 minutes.
Willingness to change
Depending on the circumstances, a few GPs fairly quickly changed their minds and were positive about the safety of home births:
GP4: Well, what you have just told me has caused me to change my view of things, I would say.
Me: That is exactly what makes this research project difficult because I would indeed have liked to have your comments and statements on tape.
GP4: Then you have to write it down immediately.
Conflicting thoughts
For others the evidence convinced their minds but not their hearts:
Me: When you say you’ve stopped your crusade against home birth, but strongly would advise against it, what has changed then?
GP1: That I mention the possibility now. As neutral as I can.
GP5: So do I.
Me: And if the woman then asks: What would you choose yourself?
GP1: So I would say: Never ever! Under no circumstances!
Me: OK. I think that is rather brilliant, that you actually do mention it.
GP5: Yes (with strong, audible exhalation)!
Me: Quite daring of you! (GP5 laughs). If you really feel like: “Oh my God, this is insane!” (everyone bursts out laughing and there is alot of noise).
GP1: You actually had some pretty hard core evidence!
GP5: (laughing): You had a good point; I’ll admit that. You can’t just say, if you consider yourself some sort of specialist, then you can’t just say (still laughing): “Yeah, yeah, evidence… Stuff that!” either, eh?
GP1: Mmm.
GP5: But I still have a personal opinion … you know … I try to mention it, completely neutral, but if they ask what I think … and they often do, I have to tell them my honest opinion.
Barriers to change
For a few it seemed – for practical reasons – too great a barrier to consider making any changes in clinical practice:
GP6: As I said, we have promised each other in the clinic that we would not undertake projects of any kind this year, as we have a great need to implement the initiatives we have been working on for the last 2 years. We discussed your project and agree that the aspect is interesting. We do not have the time needed to read the articles, implement the procedure in the clinic …, and participate in the subsequent interview.
In this group were those GPs who had reacted spontaneously but even after reflecting remained sceptical, either giving more negative personal experiences, questioning the validity of the statistics, or adding specific questions:
GP6: As I told you, I personally have some barriers which it would take a lot to overcome. This is purely my own perspective - not applicable for the entire clinic. When reading the abstracts, I can see that “risk rate” at home birth versus hospital birth is comparable. However, what I find most interesting is: What is the prognosis for mother and child in cases where things go wrong, i.e. what does it mean to have a complication at home vs hospital? What are the long-term prognoses for those children who end up in intensive care from home versus those coming in intensive care from a hospital ward? My common sense tells me that the long-term prognosis should be poorer for a home birth, where there is no pediatrician on call, no possibility for transfusion following blood loss, etc. I cannot see this aspect in the articles that we discussed, but perhaps it is stated in the article itself and just not in the abstract?
Patterns among those open to change
Interestingly, those who at first had responded with a listening attitude often were gatekeepers or people who turned out to have had a positive attitude prior to my presentation of the evidence because the idea about home birth was not unfamiliar. One had, for example, lived some years in the Netherlands, another had worked as a doctor in a small hospital and attended a few births (and added: ‘I'm glad a midwife was present’), and a third said:
GP7: Many years back … as a friend of the house, I attended a home birth.
Timing of changes
Some GPs made a pledge to change clinical practice within an hour or two; for other GPs it took more than a year to decide to hand out the local home birth leaflet. An example of the first occurred when I was invited to present the evidence to a local group of GPs. At the end of the meeting, I asked if any of them might be interested in joining the project; six of the present 12–14 GPs requested a package of information leaflets. Most other GPs had weeks or months to consider making a change before I met them again and, when asked, accepted to receive a package of local leaflets, hand them out and inform about the option of home birth. Three key GPs that as part of their roles had been presented to my project plans and the evidence very early on, had supported my project ideas throughout, and who also saw pregnant women in their own clinics did not spontaneously change their own information practice until I asked them directly more than a year later.
Discussion
Summary
The GPs in this study reacted differently to the presented evidence about home birth and to my proposal to consider a change in information to pregnant women, both between GPs and for GPs individually over time. For many GPs, the Cochrane review did challenge previous perceptions. Ample time and resources for dialogue, deliberations and adaptation to local circumstances were required for them to accommodate to change and some never changed.
Strengths and weaknesses
Due to challenges getting access to the field, I decided to make field notes and use ethnographic methods instead of the planned audio-taped focus group interviews. A major advantage of this change was the opportunity to observe and register very spontaneous reactions without interruptions to ask for permission to audio record, to find a quiet place, to discuss expected duration of interview, etc.; interruptions that might well inhibit the expression and observation of spontaneous reactions. Also having the structured research question for the systematic focus group interviews at the back of my head during the less structured encounters was an advantage as was the ability to follow reactions mature over time which was not included in the original plan. Furthermore, having met, by chance, the GP who pioneered the introduction of EBM into Danish general practice years ago may well have been of invaluable help when I re-introduced myself into the field. On the other hand, being an outsider probably helped avoid ‘conceptual blindness’, as familiarity of the ‘insider’ ‘may dominate the process of data analysis and prevent novel insights’ [Citation18]. Had I been a GP interviewing fellow GPs, it might well have been problematic to obtain sufficient distance from the topic being investigated [Citation18]. The methods, findings and interpretations have so far been well received among fellow scientists increasing the likelihood that the knowledge will be ‘used and make a difference [my translation]’[17, p. 183]. Following a scientific presentation among GPs active in research and/or clinical practice, one stated ‘All the reactions are known to me doing research in a similarly tabooed area: cancer screenings among adults’, whereas other researchers, on e.g. infectious diseases or dementia, commented on the relevance of the classification into spontaneous and reflective reactions for their own research. Overall, I have attempted to describe my methods in sufficient detail to make my approach transparent, my findings intelligible, and my proposed interpretations plausible.
On the other hand, I am a novice in the field of qualitative research, I had substantial difficulties accessing the field, and the study developed in an iterative manner which overall made it challenging to sharply delimit the aim of the present paper from the aims of the other qualitative studies and to write the methods section. To my knowledge, no papers have described the types of biases that may be expected or has been observed when a statistician is studying clinicians in an area he has a fairly good knowledge about. The peer reviewers of this paper have not pointed to any obvious directions of any such bias. It is hard to imagine that no bias exists and it is definitely a weakness of this study that the direction or nature of any such bias seems not to have been described previously. The selection and structuring of the interactions presented in the results section would probably be different, had another researcher done part or all of the work and it may be seen as weakness that the study was not carried out by a researcher more experienced in carrying out and reporting ethnographic research under challenging conditions. However, no presentation, selection or interpretation of the interactions, not even from the most qualified qualitative researcher would be ‘the truth’. It is a bit like point estimates with confidence intervals in quantitative studies – they are not ‘the truth’ either.
Comparison with existing literature
There ‘is no comprehensive understanding or theory as to how choices are made by physicians’ [Citation19] nor has the subject of choice and decision making in general ‘received proper scholarly attention among anthropologists’ [Citation20]. However, the presence of spontaneous reactions along with more delayed reactions is in line with the work of Daniel Kahneman who described human decision-making as driven by two systems: System 1 that is fast, intuitive and emotional, and System 2 that is slower, more deliberative and more logical [Citation21]. Intuitions often come first and reasoning follows to either support that intuition [Citation22,23] or, ideally, challenge it. Personal backgrounds seemed, however, to influence both spontaneous and delayed reactions. The first two listed types of spontaneous reaction were the most common. The type of reactions that highlight dramatic, clinical experiences was typically System 1: ‘Fast, automatic, frequent, emotional, stereotypic, subconscious’ [Citation24]. However, these reactions may also be seen as experienced clinicians doing their best to explain ‘real life situations’ to an ivory tower researcher, in this case a statistician. The second, more welcoming, type of reaction was often from gatekeepers or people who later turned out to have personal or professional experiences with home birth. Thus they did not experience any conflict between previous experiences and the new evidence.
In cases where the project had challenged GPs’ previous conceptions, their immediate reactions were followed by more deliberate considerations that either lead to a decision to change their clinical practices or to additional questions about the validity or sufficiency of the presented or available evidence. These reactions are in line with the theory of cognitive dissonance as described by Festinger [Citation25]. If GPs feel that their own clinical experiences are in conflict with the research evidence, they may either increase the value of their own experiences to a level where the degree of ‘blood and danger’ blocks out the value of the scientific evidence, or they may decrease the value of the scientific evidence. Festinger argued, however, that such cognitive dissonance could also be a driver for change. This is what happened for those GPs who accepted to join the second part of the project and chose to inform pregnant women about the home birth option. But for some GPs, as illustrated by the audio-recorded re-enactment with GP1 and GP5, the cognitive dissonance between the scientific evidence and their personal experiences continued as is evident in their use of swearing, heavy breathing, laughs, extreme case formulations and emphasis in the utterances indicating a high level of emotional distress.
A place to look for similar findings regarding how clinicians think is the two books both named ‘How doctors think’ [Citation26,27]. However, the books mainly cover clinical reasoning, a specific type of thinking that typically ‘occurs [in] situations involving patient and […] health care provider[s]’ [Citation28]. ‘Other essential modes of thought such as … evaluation of evidence, creative thinking, … critical reflection’ [Citation28] and other types of thinking ‘away from the patient’ is probably more relevant for the research aim of the present paper: ‘to investigate how clinicians […] think about home birth in relation to the evidence’ [Citation7]. ‘Clinicians and scientists alike need multiple thinking strategies, such as critical thinking, clinical judgment, diagnostic reasoning, deliberative rationality, scientific reasoning, […] and so on’ [Citation28]. The findings of the current paper shed some light on how clinicians think outside the clinical encounter. Groopman noted that ‘On average, a physician will interrupt a patient describing her symptoms within eighteen seconds [… and i]n that short time […] decide on the likely diagnosis and best treatment’ [Citation26]; this way of thinking seems to some extent to spill over to encounters outside the clinic.
Gabbay and le May studied decision-making among GPs within the clinic. [Citation29] The decision-making in the pilot clinic in the present study took place behind closed doors, so my findings cannot be directly compared to their findings. However, my findings illustrate types of individual thinking that take place before a decision is arrived at in the micro-community of GPs in a surgery. Gabbay and le May later pointed out that ‘mindlines inevitably vary’ and there is ‘the risk of ill-founded mindlines being shared uncritically, undermining good practice’. [Citation30]
The present study supplements the most recent systematic reviews on diffusion of evidence [Citation4–7] with a more open qualitative approach. It suggests that many GPs evaluate the evidence on home births in the strong light of the many high-risk births they have seen in hospitals and that this in turn results in various degrees of cognitive dissonance and contributes some potential reasons for variations among clinicians with respect to the timing of their readiness to change practice. It also supplements the findings of an older, more extensive systematic review in which the authors state that even ‘evidence-based innovations undergo a lengthy period of negotiation among potential adopters, in which their meaning is discussed, contested and reframed.’ [Citation31] In line with Festinger’s general theory and my findings they add that ‘such discourse can increase or decrease the innovation’s perceived relative advantage’ [Citation31]. In line with my findings, they also found strong direct evidence that innovations not ‘compatible with the intended adopters’ values, norms, and needs’ are less readily adopted.
Conclusions
Using ethnographic methods, this study demonstrated that new evidence challenging previous views may elicit fast, intuitive emotional reactions [Citation21] and upon more deliberate reflections may lead to cognitive dissonance [Citation25]. It also illustrates types of individual thinking that take place before a decision is arrived at in the micro-community of GPs in a surgery [Citation29] and that fast clinical reasoning [Citation26–28] may spill over to decision-making outside the clinic encounters. Thus the present study contributes some potential reasons for variations among clinicians with respect to the timing of their readiness to change practice. The study also contributes on a micro level to the sought understanding [Citation4,Citation6] of what happens during the ‘lengthy period[s] of negotiation’ [Citation31] leading to delays and lack of diffusion, dissemination and implementation of evidence. The findings may not be universally applicable, but selected findings were recognized by researchers in, for example, screening and infectious diseases – areas where dogmas like ‘better safe than sorry’ and ‘prevention is better than cure’ are not always necessarily true.
Ethical approval
This type of research does not require institutional ethical approval in Denmark.
Notes on contributor
Ole Olsen is a Senior Researcher at The Research Unit for General Practice and Section of General Practice, University of Copenhagen, Copenhagen, Denmark.
Acknowledgements
Thanks to The Research Unit for General Practice, University of Copenhagen for offering office facilities and many useful collegial discussions and advice. I am particularly grateful to emeritus associate professor and GP Klaus Witt who supported my project right from the start and paved my way into the field.
Disclosure statement
The author declares that he has no conflicts of interests.
Additional information
Funding
References
- Greenhalgh T, Howick J, Maskrey N. Evidence Based Medicine Renaissance Group. Evidence based medicine: a movement in crisis? BMJ. 2014;348:g3725
- Gülmezoglu AM, Langer A, Piaggio G, et al. Cluster randomised trial of an active, multifaceted educational intervention based on the WHO Reproductive Health Library to improve obstetric practices. BJOG. 2007;114:16–23.
- Thorp J. O', Evidence-based medicine-where is your effectiveness? BJOG. 2007;114:1–2.
- Cochrane LJ, Olson CA, Murray S, et al. Gaps between knowing and doing: understanding and assessing the barriers to optimal health care. J Contin Educ Health Prof. 2007;27:94–102.
- Greenhalgh T, Wieringa S. Is it time to drop the 'knowledge translation' metaphor? A critical literature review. J R Soc Med. 2011;104:501–509.
- Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med. 2011;104:510–520.
- Olsen O, Clausen JA. Planned hospital birth versus planned home birth. Cochrane Database Syst Rev. 2012;9:CD000352.
- National Institute for Health and Care Excellence. Intrapartum care: care of healthy women and their babies during childbirth (Clinical Guideline 190); 2014. [cited 2015 Jan 22]. Available from: http://www.nice.org.uk/guidance/CG190/chapter/1-Recommendations#place-of-birth.
- International Federation of Gynecology and Obstetrics. A call for the European Union to honour its commitment to fundamental human rights for women and to halt, in the European countries where it exists, the criminalisation of midwifery; 2012. Available from: http://www.figo.org/sites/default/files/120306%20ICM%20FIGO%20statement.pdf.
- Sundhedsstyrelsen [National Board of Health]. Anbefalinger for svangreomsorgen [Recommendations for pregnancy care]. Copenhagen: Sundhedsstyrelsen. [cited 2015 Jan 22]; 2013. Available from: http://sundhedsstyrelsen.dk/publ/publ2009/CFF/gravide/svangreomsorgen.pdf.
- Vedam S, Schummers L, Stoll K, et al. The Canadian Birth Place Study: describing maternity practice and providers' exposure to home birth. Midwifery. 2012;28:600–608.
- Clarke AE. Situational analysis: grounded theory after the postmodern turn. Thousand Oaks (CA): Sage; 2005.
- Rubow C. Samtalen: Interviewet som deltagerobservation [The dialogue: The interview as participant observation]. In K. Hastrup editor, Ind i verden: Grundbog i antropologisk metode. Copenhagen: Hans Reitzel; 2003. p. 227–244.
- Stensland P, Malterud K. New gateways to dialogue in general practice. Development of an illness diary to expand communication. Scand J Prim Health Care. 1997;15:175–179.
- Althabe F, Buekens P, Bergel E, et al. A behavioral intervention to improve obstetrical care. N Engl J Med. 2008;358:1929–1940.
- Malterud K. Systematic text condensation: a strategy for qualitative analysis. Scand J Public Health. 2012;40:795–805.
- Malterud K. Kvalitative metoder i medisinsk forskning (3. utgave). [Qualitative methods in medical research] Oslo: Universitetsforlaget; 2011.
- Coar L, Sim J. Interviewing one's peers: methodological issues in a study of health professionals. Scand J Prim Health Care. 2006;24:251–256.
- Eaglstein WH. Evidence-based medicine, the research-practice gap, and biases in medical and surgical decision making in dermatology. Arch Dermatol. 2010;146:1161–1164.
- Boholm Å, Henning A, Krzyworzeka A. Anthropology and decision making: an introduction. Focaal – J Glob Hist Anthropol. 2013;65:97–113.
- Kahneman D. Thinking, fast and slow. New York: Farrar Straus & Giroux; 2011.
- Haidt J. The emotional dog and its rational tail: a social intuitionist approach to moral judgment. Psychol Rev. 2001;108:814–834.
- Zajonc RB. Feeling and thinking. Am Psychol. 1980;35:151.
- Wikipedia contributors. Thinking, Fast and Slow. Wikipedia, The Free Encyclopedia; 2013. [cited 2013 Jul 30]. Available from http://en.wikipedia.org/w/index.php?title=Thinking,_Fast_and_Slow&oldid =644907523.
- Festinger L. Cognitive dissonance. Sci Am. 1962;207:93–107.
- Groopman J. How doctors think. Boston, MA: Mariner Books; 2011.
- Montgomery K. How doctors think: clinical judgment and the practice of medicine. 1st Ed. New York: Oxford University Press Inc; 2012.
- Benner P, Hughes RG, Sutphen M. Chapter 6 clinical reasoning, decision making, and action: thinking critically and clinically. In Hughes RG, editor. Patient safety and quality: an evidence-based handbook for nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008.
- Gabbay J, le May A. Evidence based guidelines or collectively constructed “mindlines?” Ethnographic study of knowledge management in primary care. BMJ. 2004;329:1013.
- Gabbay J, le May A. Mindlines: making sense of evidence in practice. Br J Gen Pract. 2016;66:402–403.
- Greenhalgh T, Robert G, Macfarlane F, et al. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82:581–629.
