Abstract
Objective: The aim of this study was to assess the relationship between self-rated health (SRH) and the American Heart Association’s (AHA) concept of ideal cardiovascular health (CVH) among female municipal employees. Studies about the association are scarce, even though AHA recommends to use SRH status surveys in clinical practice and research settings of CVH.
Design: Cross-sectional study conducted in 2014.
Setting: SRH was assessed with a one-item question and the data of seven ideal CVH measurements (nonsmoking, body mass index <25.0 kg/m2, healthy diet, physical activity at goal, blood pressure <120/80 mmHg, cholesterol <5.18 mmol/l and glucose (HbA1c < 6.0%)) was gathered with a physical examination, laboratory tests, medical history and self-administrated questionnaires.
Subjects: A total of 725 female subjects from 10 work units of the city of Pori, Finland.
Main outcome measures: SRH and ideal CVH.
Results: Of the study subjects, 28.8% reported ill-health (poor/fair SRH). The sum of ideal CVH metrics was positively associated with good SRH driven by favorable health behaviors (nonsmoking, normal body mass index, healthy diet and physical activity). A linear decrease in the prevalence of 0–2 ideal CVH metrics, and a linear increase in 5–7 metrics was associated with better SRH. Nonsmoking and normal weight were the most potent indicators of good SRH in multivariate analysis.
Conclusions: Most of the subjects with 0–3 of the seven CVH metrics at ideal level were dissatisfied with their health. Since unhealthy lifestyle factors accumulate mainly to people feeling ill-health, the value of SRH is worth recognizing especially in primary health care.
Introduction
In drive for a cost-effective healthcare, it is important to sort quickly patients needing more profound medical interventions. Frequently, the physician starts the appointment with a question: ‘How do you feel?’. This simple question is a powerful health measure based on the patient´s subjective assessment of his/her health status. Self-rated health (SRH) is linked to cardiovascular disease (CVD) morbidity and mortality [Citation1–3] as well as to all-cause mortality [Citation1,Citation4,5].
Non-communicable diseases (like CVDs, cancers, chronic respiratory diseases and diabetes) are the leading cause of death globally and closely linked to health behaviors [Citation6]. Adoption of healthy lifestyle is associated with good SRH [Citation7–11], better mental health [Citation8], as well as reduction of chronic disease burden [Citation12]. The American Heart Association (AHA) has named poor SRH as a risk factor and health outcome of cardiovascular health (CVH), but the potential of SRH is not widely realized yet [Citation13].
AHA has created a concept of ideal CVH comprising of ideal health factors (blood pressure <120/80 mmHg, total cholesterol <5.18 mmol/l, fasting blood glucose <5.55 mmol/l) and ideal health behaviors (nonsmoking, normal body mass index (BMI), healthy diet and physical activity at goal) [Citation14]. The aim of this concept is to improve CVH by 20% while reducing CVD mortality and improving CV risk factors in the US population by 20% by the year 2020. Having several ideal CVH metrics is known to be associated with reduced all-cause and CVD-related mortality [Citation15,16] and incident CVD [Citation16,17]. The ideal CVH is also related to non-CVD outcomes such as fewer psychosocial risk factors [Citation18], increased optimism [Citation19] and lower health care costs [Citation20].
Studies investigating the relationship of SRH and the ideal CVH are scarce. We hypothesized that the sum of ideal CVH, as an indicator of lifestyle and CVD risk, would associate with the general SRH among working-aged women.
Materials and methods
Participants and study design
PORTAAT (PORi To Aid Against Threats) is a longitudinal study conducted among employees of the city of Pori (83,497 inhabitants in 2014) in Southwest Finland. This study population comprised workers from 10 work units, which were selected by the chief of the municipal welfare unit of Pori. An invitation and study information letters were sent to 2570 employees as an email attachment by the managers of the work units. Information events were also organized for employees. Altogether 836 employees (104/369 males, 732/2201 females) consented to participate in the PORTAAT study. There were no exclusion criteria. Seven participants did not answer the SRH question, and thus, the analytic sample in this study was 725 female employees working in libraries (n = 22), museums (n = 33), technical management (n = 80), social services (n = 195) and health care units (n = 395).
Measures
Self-rated health (SRH)
SRH was assessed with the question: ‘How satisfied are you with your health?’. The response scale ranged in the Likert scale from 1 (very dissatisfied) to 5 (very satisfied). This question and response scale is based on the WHO’s Quality of Life questionnaire (WHOQOL-BREF) [Citation21]. Even though the wording and the scale of one-item assessment of SRH vary across surveys, it has shown to be reliable and valid [Citation4,Citation22,Citation23]. Due to the low rate of very dissatisfied persons (9/725, 1.2%), we combined the very dissatisfied and dissatisfied groups as poor, and used four categories (poor, fair, good and excellent) to evaluate SRH.
The seven ideal cardiovascular health metrics
Smoking status was assessed by a questionnaire. Nonsmoking was defined as having never smoked or having quit smoking >12 months ago.
Height and weight were measured by a study nurse with the subjects in a standing position without shoes and outer garments. Weight was measured to the nearest 0.1 kg with calibrated scales and height to the nearest 0.5 cm with a wall-mounted stadiometer. Body mass index (BMI) was calculated as weight (kg) divided by the square of height (m2). The ideal BMI was <25.0 kg/m2.
Physical activity was assessed using a questionnaire that asked the frequency and duration of physical activities in a typical week. Ideal physical activity was defined as engaging in ≥150 minutes per week of moderately intense activities or ≥75 min per week of vigorously intense activities or ≥150 min per week of moderately + vigorously intense activities [Citation14].
Information concerning diet was collected with a food–frequency questionnaire. Daily consumption of fruits, vegetables, whole grains, unsaturated dietary fats and white meat (poultry, fish) at least three times a week were considered to be a healthy diet. Intake of the ideal level of each dietary component was scored with one point, from a range of 0–5. The dietary CVH metric was categorized as ideal, if a dietary score of 4–5 was achieved [Citation14].
Blood pressure was measured by a study nurse with an automatic validated blood pressure monitor with subjects in a sitting posture, after resting for at least 5 min. In the subjects whose arm circumference was >32 cm, a larger cuff was used. Two readings, taken at intervals of at least two minutes, were measured, and the mean was used in the analysis. The ideal level was an untreated blood pressure of <120 mmHg systolic and <80 mmHg diastolic.
Laboratory tests were determined in blood samples, which were obtained after at least 8 hours of fasting. Total cholesterol was measured enzymatically (Architect c4000/c8000). The ideal level was an untreated total cholesterol <5.18 mmol/l. Glucose tolerance was measured with glycated hemoglobin (HbA1c) which was analyzed using high-performance liquid chromatography method, HPLC, (Tosoh HLC-723G7 (G7)). The AHA metric uses fasting plasma glucose (<5.55 mmol/l) to determine normoglycemia; however, we used HbA1c because of its property of giving an indication of glycemia over several preceding weeks rather than at a single time point [Citation24]. Normoglycemia was defined as HbA1c < 6.0% (<42 mmol/mol) [Citation25].
The seven ideal CVH metrics were grouped into three categories: poor (0–2 ideal CVH metrics), intermediate (3–4 ideal CVH metrics) and ideal (5–7 ideal CVH metrics) level of cardiovascular health [Citation18].
Other measures
With self-administrated questionnaires and medical records, information was gathered about diseases diagnosed by a physician, years of education, marital status (cohabiting or not) and quality of sleep (good or not good). Alcohol consumption was assessed with the 3-item Alcohol Use Disorders Identification Test (AUDIT-C) with a cutoff of 5 points for harmful drinking [Citation26]. The participants’ financial satisfaction was assessed with the question ‘I have to spare expenditures’ (yes or no).
We assessed the worker´s ability to participate in work with the question ‘What is your current work ability compared to lifetime best?’. This first item of widely used Work Ability Index [Citation27] is named Work Ability Score (WAS) and has a 0–10 response scale, where 0 represents ‘completely unable to work’ and 10 ‘work ability at its best’. Reference values for WAS are suggested as for Work Ability Index; poor (0–5 points), moderate (6–7 points), good (8–9 points), excellent (10 points) [Citation28]. WAS has a strong association with the Work Ability Index and is trustworthy in evaluating work ability [Citation29].
Informed consent
The study protocol and consent forms were reviewed and approved by the Ethics Committee of the Hospital District of Southwest Finland. All participants provided written informed consent for the project and subsequent medical research.
Statistical analysis
Statistical significance for the hypothesis of linearity across categories of SRH and ideal CVH metrics were evaluated by using the Cochran–Armitage test or generalized linear models (analysis of variance and logistic models). In the case of violation of the assumptions (e.g. non-normality), a bootstrap-type test was used. A multivariate logistic regression model was used to investigate factors related to the good or excellent SRH. All analyses were performed using STATA 14.1 (StataCorp LP, College Station, TX).
Results
We evaluated 725 female employees (mean age 48 ± 10 years). shows the characteristics of the study subjects according to categories of SRH. Poor or fair health was reported by 209/725 (28.8%) and good or excellent health by 516/725 (71.2%) of the subjects. WAS, financial satisfaction, good quality of sleep, lower BMI, healthy diet, lower diastolic BP and HbA1c were associated with better SRH.
Table 1. Characteristics of the study subjects according to categories of self-rated health.
Of the study subjects, 25.2% had 5–7 CVH metrics, 53.1% had 3–4 metrics and 21.7% had 0–2 metrics at the ideal level. The presence of any chronic disease, especially diabetes, hypertension, CHD, musculoskeletal disorders and depression, had a negative relationship with SRH.
Most of the subjects with 0–3 of the seven CVH metrics at ideal level were dissatisfied with their health, when adjusted for age and years of education. ()
Figure 1. The distribution of categories of self-rated health according to the sum of ideal CVH metrics.
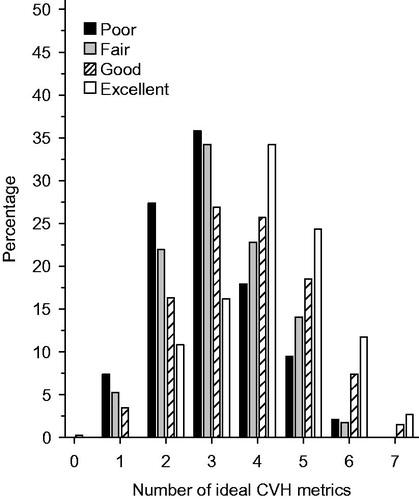
A linear decrease in the prevalence of 0–2 ideal CVH metrics, and a linear increase in 5–7 metrics was associated with better SRH. The prevalence of 3–4 health metrics was quite stable across the categories of SRH ().
Figure 2. The prevalence of ideal CVH metrics in self-rated health categories [Poor (P), Fair (F), Good (G), Excellent (E)].
![Figure 2. The prevalence of ideal CVH metrics in self-rated health categories [Poor (P), Fair (F), Good (G), Excellent (E)].](/cms/asset/595c5532-a8d6-4b09-9fb9-5853e5534637/ipri_a_1397299_f0002_b.jpg)
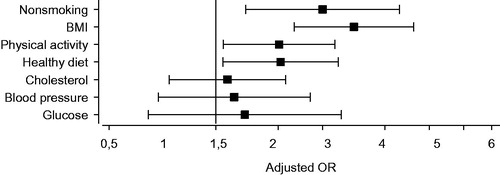
Participants satisfied with their health were more likely to have ideal health behaviors and ideal health factors than participants who were dissatisfied of their health. Only ideal BP and glucose levels were not related to SRH in the fully adjusted model ().
Table 2. Ideal cardiovascular health metrics according to categories of self-rated health.
In multivariate analysis, good/excellent SRH was associated with nonsmoking [odds ratio (OR) 2.00 (95% CI: 1.22–3.30)], normal BMI [OR 2.45 (95% CI: 1.66–3.61)], physical activity at goal [OR 1.51 (95% CI: 1.05–2.17)] and healthy diet [OR 1.52 (95% CI: 1.05–2.22)] when adjusted for age, years of education, cohabiting, alcohol consumption and number of chronic diseases ().
Discussion
This study demonstrates that the sum of ideal CVH metrics is positively associated with good SRH driven by the positive relationship of health behaviors (nonsmoking, normal BMI, healthy diet and physical activity).
For the strengths of our study, we can attribute that anthropologic measures were conducted by trained medical staff, and objective indicators of physical health were used. With many occupational groups involved in the study, we can generalize the results widely to female employees. This study has also some limitations. The cross-sectional nature of our study disallows us to conclude the causality of lifestyle factors and one-item SRH. Also, stress or anxiety were not measured as potential confounding factors. Moreover, a healthy worker effect is possible, because in this study, subjects out of workforce were not studied. Only 33.3% of the invited female employees participated in the PORTAAT study. According to the personnel report 2014 of the city of Pori [Citation30], the mean age of 48 years and the mean education level of the study participants were comparable to the means of the entire personnel of the city.
Our study confirms previous study results about the relationship between one-item SRH and health behaviors. Smoking [Citation7–8,Citation10,Citation31] and overweight [Citation7,Citation31] have been shown to associate with poor SRH. Maintaining normal weight usually requires healthy diet and adequate exercise. Lack of adherence to dietary [Citation7–8,Citation10,Citation31] guidelines has a negative, whereas physical activity [Citation7–8,Citation10,Citation31,32] has a positive relationship with SRH. Also in our analysis, healthy diet and adequate exercise were significant predictors of good/excellent SRH. Importantly, Tsai et al. [Citation31] have reported that the more healthy behaviors the better the single-item SRH, especially among adults with CVD or diabetes.
To the best of our knowledge, only Allen et al. [Citation11] have previously shown that one-item SRH is better among those with more ideal CVH metrics. Our results add new information about how strongly each CVH metric predicts SRH in working-aged women. Normal BMI is the most potent indicator of good self-reported well-being and nonsmokers rate their health twice as good as current smokers. These two health behaviors are also the most protective metrics against a loss of ideal CVH profile through middle age [Citation33]. According to the present study, ideal plasma cholesterol, glucose or blood pressure levels do not predict good SRH. Thus, one-item SRH seems to distinguish persons with unhealthy lifestyle which may contribute to many diseases, not only CVD.
In our study population of female employees, 29% reported ill-health (poor/fair SRH). The majority of them reached only to 0–3 of the seven ideal health metrics. These subjects also had more diagnosed diseases and cardiovascular risk factors, as well as poorer quality of sleep, diet and physical activity level than subjects feeling good or excellent. Thus, health care providers might warrant increased attention with holistic approach for those reporting poor SRH taking into consideration the physiological, psychological and social factors as well as health education. Noteworthy for primary and occupational health care is that among employees reporting ill-health in our study population, the average WAS (scale 0–10) was only 7. Good SRH has also been reported to predict return to work after long-term sickness [Citation34].
Lifestyle-related diseases are on the rise and adoption of unhealthy habits and people living longer may be among the potential explanations. While healthy habits are known to associate with better SRH [Citation7–11,Citation31,32], the mechanism is unclear. Reporting poor SRH has been speculated to depict hidden symptoms, risk factors or diseases, which could convey to future health outcomes [Citation2,Citation35]. It is thought that SRH captures aspects of health that more guided questionnaires cannot [Citation35]. The ideal CVH, as an indicator of lifestyle and CVD risk, is linked to optimism [Citation19], which is also suggested to explain SRH, so that optimistic people would rate their health higher than pessimistic people [Citation36]. Stress and anxiety may also be confounders or mediators of SRH due to the physiologic consequences of adapting to repeated stress [Citation37]. These psychosocial factors are also risk factors for CVD and can often be real barriers for lifestyle changes. Finding reasons for low subjectively experienced health could lead to targeted risk factor interventions and could be the key for attaining better health behaviors with favorable CVH outcomes later.
For a clinical practitioner, valuable information about health and well-being from the patient’s point of view can be obtained by simply asking ‘How satisfied are you with your health?’. This one-item SRH can be used as a substitute for time-consuming health-related quality of life questionnaires in the hectic office of primary care physician. Our results provide evidence that one-item SRH, as a simple, quick and inexpensive method, helps to recognize persons at risk of poor health. Targeting resources to those feeling ill-health, over those reporting good/excellent SRH with probable healthy lifestyle, could save time and effort of clinicians and reduce costs of healthcare. The potential of SRH lies in the rational clinical decision-making, cost-effective targeting of the healthcare resources and better surveillance of disease burden [Citation13].
Conclusions
The sum of ideal CVH metrics is positively associated with good SRH driven by favorable health behaviors (nonsmoking, normal BMI, healthy diet and physical activity). Since also unhealthy lifestyle factors accumulate mainly to people feeling ill-health, the value of SRH is worth recognizing especially in primary and occupational health care.
Notes on contributors
Veera Veromaa, MD, specializing GP in Family Medicine, University of Turku and Turku University Hospital, Turku, Finland and Central Satakunta Health Federation of Municipalities, Harjavalta, Finland.
Hannu Kautiainen, BA, biostatistician in Folkhälsan Research Center, Helsinki, Finland and Unit of Primary Health Care, Kuopio University Hospital, Kuopio, Finland.
Markus Juonala, MD, PhD, Professor inDepartment of Internal Medicine, University of Turku and Division of Medicine, Turku University Hospital, Turku, Finland.
Ansa Rantanen, MD, GP in Health Centre of Salo, Salo, Finland.
Päivi E Korhonen, MD, PhD, Professor in Institute of Clinical Medicine, Family Medicine, University of Turku and Turku University Hospital, Turku, Finland.
Disclosure statement
The authors declare that there are no conflicts of interest.
Additional information
Funding
References
- Benjamins M, Hummer R, Eberstein I, et al. Self-reported health and adult mortality risk: an analysis of cause-specific mortality. Soc Sci Med. 2004;59:1297–1306.
- Mavaddat N, Parker R, Sanderson S, et al. Relationship of self-rated health with fatal and non-fatal outcomes in cardiovascular disease: a systematic review and meta-analysis. PLoS One. 2014;9:e103509.
- Barger SD, Cribbet MR, Muldoon MF. Participant‐reported health status predicts cardiovascular and all‐cause mortality independent of established and nontraditional biomarkers: evidence from a representative US sample. J Am Heart Assoc. 2016;5:e003741.
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37.
- DeSalvo KB, Bloser N, Reynolds K, et al. Mortality prediction with a single general self-rated health question. A meta-analysis. J Gen Intern Med. 2006;21:267–275.
- World Health Organization (WHO) Global Status Report on noncommunicable diseases 2014. WHO Press; 2014. [Internet]. [cited 2017 Sep 30]. Available from: http://www.who.int/nmh/publications/ncd-status-report-2014/en/
- Kwaśniewska M, Kaleta D, Dziankowska-Zaborszczyk E, et al. Lifestyle index and self-rated health status. Int J Occup Med Environ Health. 2007;20:349–356.
- Harrington J, Perry I, Lutomski J, et al. Living longer and feeling better: healthy lifestyle, self-rated health, obesity and depression in Ireland. Eur J Public Health. 2010;20:91–95.
- Yamada C, Moriyama K, Takahashi E. Self-rated health as a comprehensive indicator of lifestyle-related health status. Environ Health Prev Med. 2012;17:457–462.
- Mood C. Life-style and self-rated global health in Sweden: a prospective analysis spanning three decades. Prev Med. 2013;57:802–806.
- Allen N, Badon S, Greenlund K, et al. The association between cardiovascular health and health-related quality of life and health status measures among U.S. adults: a cross-sectional study of the National Health and Nutrition Examination Surveys, 2001–2010. Health Qual Life Outcomes. 2015;13:152.
- Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260.
- Rumsfeld JS, Alexander KP, Goff DC Jr, et al. Cardiovascular health: the importance of measuring patient-reported health status: a scientific statement from the American Heart Association. Circulation. 2013;127:2233–2249.
- Lloyd-Jones D, Hong Y, Labarthe D, on behalf of the American Heart Association Strategic Planning Task Force and Statistics Committee, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613.
- Ford ES, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125:987–995.
- Dong C, Rundek T, Wright CB, et al. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and hispanics: the northern Manhattan study. Circulation. 2012;125:2975–2984.
- Folsom AR, Yatsuya H, Nettleton JA, et al. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–1696.
- Veromaa V, Kautiainen H, Saxen U, et al. Ideal cardiovascular health and psychosocial risk factors among Finnish female municipal workers. Scand J Public Health. 2017;45:50–56.
- Hernandez R, Kershaw K, Siddique J, et al. Optimism and cardiovascular health: multi-ethnic study of atherosclerosis (MESA). Health Behav Policy Rev. 2015;2:62–73.
- Willis B, DeFina L, Bachmann J, et al. Association of ideal cardiovascular health and long-term healthcare costs. Am J Prev Med. 2015;49:678–685.
- The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28:551–558.
- Lundberg O, Manderbacka K. Assessing reliability of a measure of self-rated health. Scand J Soc Med. 1996;24:218.
- Robine J-M, Jagger C, Romieu I. Selection of a Coherent Set of Health Indicators for the European Union. Phase II: Final report. Euro-REVES 2002. [Internet]. [cited 2017 Sep 30]. Available from: https://ec.europa.eu/health/ph_projects/2000/monitoring/fp_monitoring_2000_frep_03_en.pdf (p.81-95)
- Selvin E, Crainiceanu CM, Brancati FL, et al. Short-term variability in measures of glycemia and implications for the classification of diabetes. Arch Intern Med. 2007;167:1545–1551.
- The International Expert Committee. International Expert Committee Report on the Role of the A1C Assay in the Diagnosis of Diabetes. Diabetes Care. 2009;32:1327–1334.
- Bush K, Kivlahan DR, McDonell MB, et al. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158:1789–1795.
- Ilmarinen J. The Work Ability Index (WAI). Occup Med. 2007;57:160.
- Gould R, Ilmarinen J, Järvisalo J, et al. Dimensions of Work Ability. Results of the Health 2000 Survey. Helsinki (Finland): Finnish Centre of Pensions; 2008. p. 25–34.
- El Fassi M, Bocquet V, Majery N, et al. Work ability assessment in a worker population: comparison and determinants of Work Ability Index and Work Ability score. BMC Public Health. 2013;13:305.
- Personnel report 2014 of the city of Pori [Internet]. [cited 2017 Sep 30]. Available from: https://www.pori.fi/material/attachments/hallintokunnat/henkilostopalvelut/bpM8lTCC0/Henkilostoraportti_2014.pdf (p. 6-7, 9).
- Tsai J, Ford E, Li C, et al. Multiple healthy behaviors and optimal self-rated health: findings from the 2007 Behavioral Risk Factor Surveillance System Survey. Prev Med. 2010;51:268–274.
- Rosenkranz RR, Duncan MJ, Rosenkranz SK, et al. Active lifestyles related to excellent self-rated health and quality of life: cross sectional findings from 194,545 participants in The 45 and Up Study. BMC Public Health. 2013;13:1071.
- Gooding HC, Shay CM, Ning H, et al. Optimal lifestyle components in young adulthood are associated with maintaining the ideal cardiovascular health profile into middle age. J Am Heart Assoc. 2015;4:e002048.
- Momsen AM, Stapelfeldt CM, Nielsen CV, et al. Screening instruments for predicting return to work in long-term sickness absence. Occup Med (Lond). 2016;67:101–108.
- Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. 2009;69:307–316.
- Benyamini Y, Idler EL, Leventhal H, et al. Positive affect and function as influences on self-assessments of health: expanding our view beyond illness and disability. J Gerontol B Psychol Sci Soc Sci. 2000;55:107–116.
- McEwen B. Allostasis and allostatic load: Implications for neuropsychopharmacology. Neuropsychopharmacology. 2000;22:108–124.