Abstract
Objective: This study aimed to analyze the Austrian health care system using the ecology of care model. Our secondary aim was to compare data from Austria with those available from other countries.
Design: 3508 interviews employing a 30-item questionnaire related to the utilization of the health care system including demographic factors were conducted. Participants were chosen by a Random Digital Dialing procedure. Further, a literature review of studies of other countries use of the ecology of care model was conducted.
Main outcome measures: Austria has one of the highest utilization of health care services in any of the assessed categories. The comparison with the literature review shows that Austria has the highest utilization of specialists working in the outpatient sector as well as the highest hospitalization rates. Taiwan and Korea have comparable utilization patterns. Canada, Sweden, and Norway are countries with lower utilization patterns, and the U.S. and Japan are intermediate.
Conclusion: In Austria and similarly organized countries, high utilization of all health care services can be observed, in particular, the utilization of specialists and hospitalizations. The over-utilization of all levels of health care in Austria may be due to the lack of a clear demarcation line between the primary and secondary levels of care, and the presence of universal health coverage, which also allows for unrestricted and undirected access to all levels of care. Previous studies have shown that comparable countries lack the health benefits of a strong primary care system with its coordination function.
In Austria and similarly organized countries, there appears to be high utilization of health care in general, as well as with particular utilization of specialists and hospitalizations.
The high utilization of all levels of care in Austria may be the result of competition, lack of a clear demarcation line between the primary and secondary level of care, and the presence of universal health coverage.
Pathways between primary and secondary care should be strengthened as previous studies have shown that comparable countries lack the health benefits of strong primary care and its function for health care coordination.
Key points
Background
The ecological model of care, first published in the 1960s, offers calculations on the utilization of different health care services and points strongly to the need for reorienting the organization of the health care system, medical training, and research [Citation1,Citation2]. In several countries, the findings of this early publication, as well as the revised version in 2001 [Citation3] and the Declaration of Alma Ata of the World Health Organization in 1978 [Citation4], were part of the impetus for a reorientation of health care system focus away from secondary and tertiary care towards primary care. The primary level of the health care sector is the component in which the vast majority of patients should receive treatment, particularly those with complex bio-psycho-social health needs [Citation1,Citation5–9]. An increasing body of evidence demonstrates that countries with strong primary care systems perform better concerning mortality of cardio- and cerebrovascular diseases, hypertension, chronic asthma, bronchitis, and emphysema. Also, those countries investing more heavily in primary care have less avoidable hospitalizations due to diabetes, asthma, and COPD. They further show a higher level of equality about the self-rated health care status among persons with different socio-economic circumstances and have a slower rate of increase in overall health care spending [Citation7,Citation9–11]. Despite these findings and a growing body of literature, many countries have not embraced the aims of the Alma Ata declaration, and continue to prioritize secondary and tertiary care services [Citation7,Citation12,Citation13].
Austria is representative of the Bismarck-system as a national social health insurance system with universal health coverage and has emphasized secondary and tertiary health care sectors in recent decades. The Austrian healthcare system is divided into the ambulatory health care sector, where GPs, specialists with own practices, and hospital outpatient departments are included alongside the hospital sector. Open access to all levels of care, including self-referral by patients, is an intrinsic principle of the Austrian health care system [Citation14]. Within the ambulatory public sector, access is – with some minor limitations – free to all physicians with minimal or no out of pocket co-payment. It is only a recommended option for patients to visit a GP first, and then be referred to a specialist [Citation12–15]. Additionally, a disproportionately high ratio of specialists compared to General Practitioners (GPs) work in the ambulatory sector [Citation15]. GPs most often work in solo practices, are self-employed, and payment is based primarily on fee-for-service. Beginning in 2017, GPs have had the additional option to practice in larger Primary Care Centers or Networks.
The primary aim of the present study is to investigate the ecology of care model within the Austrian health care system and to evaluate variations in the ecology of care across socio-demographic groups in Austria.
The secondary aim is to compare the Austrian health care system data with that from other countries that have previously been studied on their integration of the ecology of medical care model, including Sweden, Norway, Japan, the U.S., Taiwan, and Korea. Possible key factors for different outcomes across these countries are discussed.
Methods
The study is part of the research project ‘Ecology of Medical Care – Utilization of Health Care in Austria (ECOHCARE)’ that is registered with the ClinicalTrials.gov identifier NCT01261845.
The methods used for this study were twofold. First, the utilization of the Austrian health care system was assessed through the ecology of care model, which has been published as a short report previously [Citation16]. Further, variations between different socio-demographic groups within the model were assessed. For these steps, a quantitative approach was used, which is described in detail below.
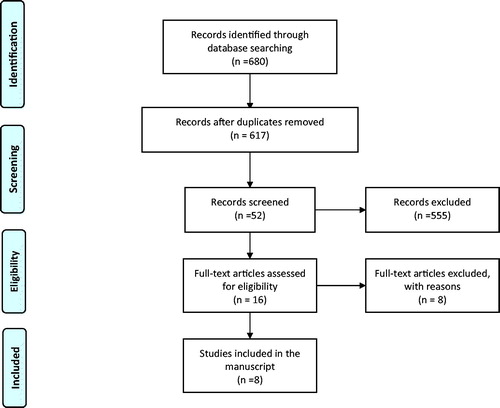
Second, publications that describe the ecology of care model in other countries were queried through a literature review. The review was performed between 1 November 2018 and 22 February 2019, of all literature available in the database PubMed published between 1961 and 2018. Inclusion criteria for the literature search were the use of the ecology of medical care model and its utilization within different sectors of the related health care systems of a country by adults of all age groups. Only the most recent data were taken into account if several publications of a given country were found. Search terms used were ‘ecology of medical care’ AND the single years between ‘1961’ and ‘2018’. After the identification of relevant publications, country data was compared to the Austrian data about the overall ecology of care model outcomes.
Quantitative approach
Sample
The overall results of the ECOHCARE study were published previously in the form of a figure, as a short report; however, the methods were not yet described at the time of that publication [Citation16]. The sample was laid out so that it formed a true-to-scale representation of the population (Mikrozensus) [Citation17]. The samples for the CATI-survey (Computer Assisted Telephone Interview) were drawn according to the standard procedure of Random Digital Dialing (RDD) on a combined sample of mobile and landline phone numbers [Citation18]. The distribution across the Austrian mobile phone carriers was made according to their market share. For the choice of the target person within one household, a random key – the so-called ‘last birthday method’ – was used, as is necessary for a representative survey. The last birthday method aims to reduce the possible selection bias of respondents by asking the person of a household called to respond, whom had a birthday most recently [Citation19]. If the chosen person was not present at the time of the call, the phone call was repeated up to four times. The survey was conducted in four waves, starting in October 2010 and ending September 2011, to avoid seasonal bias.
Questionnaire
The questionnaire consisted of 30 questions related to the utilization of the health care system and demographic factors. It was translated into the languages of the four largest non-German-speaking migrant populations in Austria (Bosnian/Croatian/Serbian and Turkish) using state of the art forward and backward translation. If a person was not able to speak German, a new appointment was made with an interviewer skilled in the appropriate language.
Measures
Utilization of health care services
To measure the utilization of health care services, participants were asked whether they used different health care services during the prior four weeks. We classified the health care services to include:
Primary care services: visits to a general practitioner (GP): ‘Were you treated by a GP within the last four weeks?’
Secondary care services: Visits to specialists (all physicians except GPs, which are not recognized as specialists in Austria) working in their own offices: ‘Were you treated by a specialist working in his or her office in the ambulatory sector within the last four weeks?’
Secondary care services: Outpatient hospital care: ‘Were you treated by a specialist in a hospital outpatient department within the last four weeks?’
Secondary care services: Hospital care: ‘Were you treated as an inpatient in a hospital within the last four weeks (except a university hospital)?’
Tertiary care: (classified as services in a university hospital): ‘Were you treated in a university hospital/academic medical center within the last four weeks?’
Demographic variables
Sex of participants, dichotomized to ‘female’ or ‘male’ as well as age were assessed. Educational status was assessed for primary (up to the age of 15 years), secondary (apprenticeship or secondary school) and tertiary education (university or any further). Working status was assessed for those working full-time, part-time, or not working.
Location of residence was surveyed by postal code as well as by federal capital and county and included assessment of the number of inhabitants. These answer categories were dichotomized into urban (Vienna and federal capitals) and rural (towns and settlements with less than 5000 inhabitants).
Participants were classified as migrants based on their country of birth. This variable was dichotomized into Austrians and others.
Data analysis
All statistical analyses were done using the statistic software SPSS 24.0. First, data were weighted by profession, age, highest education level, place of residence, and sex to enhance the similarity of the data with the Austrian population. Second, the demographic characteristics of the participants were described.
For the calculation of the ecology of care model for Austria, we used a similar methodology as published previously [Citation20,Citation21]. To present the results per 1000 persons per service, we calculated the number of individuals who actually utilized each service. This was accomplished by multiplication by a factor of 1000 and subsequent division of the result with the number of the overall sample for this service. Additionally, the number of individuals utilizing more than one service within a four-week period, particularly the GP, was calculated. All results are presented with 95% confidence interval (CI).
For the additional material, to estimate the independent effects of the individual characteristics on the different services used, all data were entered into a logistic regression analysis simultaneously to derive adjusted odds ratios (ORs) for each service group. For the calculation of the 95% CI, robust estimation of variance was used.
Results
Results of the quantitative component of this study show that 3508 respondents aged 15 years and older participated. offers an overview of participant characteristics.
Table 1. Austrian participants’ characteristics.
shows the number who presented to a given health care service. This table also details the proportion per 1000 persons in Austria, stratified by sociodemographic characteristics, who had at least one appointment with a physician within four weeks among the differing health care settings. Advanced age, having not worked recently and bad or very bad self-rated health status is associated with higher health care utilization of all services, except for that of being hospitalized in a university hospital. Hospitalization in a university hospital was associated with living in an urban region and with reported bad or very bad health status. Compared to the GP service utilization pattern, specialist use does not appear to depend on the age variable. Hospitalizations were more frequent in those with primary educational level and persons born in Austria. Further details regarding the associations of the demographics with the utilization pattern are shown in the additional material (Ad 1).
Table 2. Number of people who encountered a health care service, per 1000 persons (95% CI), stratified by sociodemographic characteristics, who had at least one appointment with a physician within 4 weeks by the different health care settings in Austria.
The results of the literature review identified 617 publications (). After reviewing these titles and abstracts, publications from seven countries and the first publication of White et al. [Citation2,Citation3,Citation20–28], three metropolis [Citation29–31], and five regional areas were selected [Citation32–36]. Due to the inclusion criteria, eight publications were chosen. Details of these publications are listed in . depicts the utilization of different services in terms of the ecology of care model for Austria as well as the seven other countries listed in . The comparison shows that Austria has high utilization of health care services in each of the assessed categories. Austria demonstrates the highest utilization of specialists working in the outpatient sector, with consideration of both specialists with their own practices and specialists in hospital outpatient departments. Austria additionally showed the highest hospitalization rates, taking into account both hospitalizations in secondary care hospitals and in academic medical centers. Taiwan and Korea are countries with similar utilization patterns. Canada, Sweden, and Norway are countries with a lower utilization pattern, and the U.S. and Japan are intermediate.
Table 3. Details of the publications of the seven countries listed in accordance with their publication date.
Table 4. Comparison of the different ecology of medical care studies: result for 1000 persons within 4 weeks.
Discussion
This is the first time that the utilization of the health care system of a wealthy European Bismarck-System country without gatekeeping was assessed through the ecology of care model and compared with results from other countries. The principal findings are overall high utilization of health care in Austria, with especially high utilizations of specialists and hospitals. The results of show a clear trend towards higher utilization of all services in Austria compared to other similar countries. Utilization of specialists was quite high (284/1000) in Austria, with similar patterns of utilization of specialists as found in Korea (136/1000) and Taiwan (152/1000). However, Taiwan and Korea both have a high percentage of hospital outpatient services, with no additional specialists working in their own practices () as this is not a component of health care in those countries [Citation25,Citation26]. Taiwan has a National Health Insurance (NHI) system with easy access to clinics, low private co-payment and access to all public and private healthcare facilities is free without the need for a referral [Citation26].
Meanwhile, in Korea, the NHI has established universal health coverage, and there is no demarcated line between primary care and hospital care. In Austria, the situation is similar, with no clear distinction between primary and secondary care, minimal or no out of pocket costs, and lack of necessity for specialty referral. As a result, much as in Korea and Taiwan, there is competition for patients.
Moreover, in Austria, the number of specialists working in the ambulatory sector is higher than the number of GPs, and their utilization is high, particularly in areas with a dense specialist care structure such as big cities. This points to a supply-induced demand [Citation15]. This element is also reflected in our results, as living in an urban region is positively associated with visiting a specialist with an own practice and being hospitalized in a university hospital ().
The utilization pattern of the U.S. health care system lies a bit lower than that observed in the three countries described above. The US maintains a referral based gate-keeping system that often prioritizes access to primary care first, before specialty consultation. However, the U.S. does not promote universal health coverage, which decreases access to services in general [Citation24,Citation32].
In contrast to the high Austrian utilization pattern of specialist and hospital services, the service utilization in Sweden, Norway, and Canada is much lower. All three countries have a focus on primary care and a regulatory mechanism of gatekeeping between the primary and secondary level of the public health care system [Citation20,Citation22,Citation27].
This leads to the conclusion that free access to all levels of care, universal health coverage and lack of gatekeeping may substantially increase utilization to the point of overutilization. As universal health-coverage is one of the most important principles of health equity and equality, it should be maintained. However, to decrease overutilization, one should consider abolishing or at least adapting the free-access-to-all-levels principle.
Austria has the highest hospitalization rates in OECD countries. One explanation could be Roemer’s law, which states that more hospital beds lead to higher hospitalization rates. This relationship was found to be robust across geographic scales that were analyzed [Citation37,Citation38]. Indeed, Austria has one of the highest numbers of hospital beds in Europe [Citation39].
A compounding factor to the weakness of the primary care sector is that basic and postgraduate education and training in General Practice and Family Medicine lags far behind European and international standards. Only recently has an obligatory six-month training period in a GP teaching practice become a component of postgraduate vocational training in general practice. This is an improvement to the situation of the last decades where essentially all vocational training and education for all medical specialties had been hospital-based only. High utilization of the secondary care sector in Austria has been identified in other publications, with the utilization of the secondary health care sector more than two to three-fold in Austria compared to countries with gatekeeping systems [Citation12,Citation13,Citation15]. In contrast, studies from the U.S. and England have shown that reductions in hospitalizations are associated with high proportions of primary care physicians relative to specialists [Citation40,Citation41]. Each of these studies offers similar reasons as to why the utilization of academic medical centers in Japan is very high, namely the free availability and ease of access in densely populated regions as well as the tertiary care focused education and training of medical students and young doctors [Citation21,Citation28,Citation33,Citation34].
However, GP service utilization in Austria is among the highest when compared to the other seven countries. In the decades since the first publication of the ecological model of care, many countries have changed the emphasis of their health care sectors to promote primary care. This has transformed how these health care systems have viewed appropriate access to care, shifting specialty visits and lowering costs. In Austria and similar countries, where the ecology model of care has yet to be embraced, there appears to exist general overutilization of care and an increased rate of use of specialists and hospitals.
The present study has some limitations. The study bears the potential for a recall bias [Citation42] as participants were questioned as to their ability to remember their utilization of health care services over the preceding four weeks. However, this recall bias should be less than that found in studies with a recall period of one year. Moreover, the reason for each health care utilization episode was not assessed and, therefore, the appropriateness utilization could not be established. The study design is cross-sectional and therefore, of limited explanatory power. The survey this study relies on was distributed eight years ago. However, there has not been a substantive change to the health care system in Austria, and more particularly within the study setting of general practice. In particular, any regulation to access the different levels and services of care is still lacking and politically not even considered. Therefore, we believe the survey and responses to be both novel and relevant about the current situation.
One strength is that the Austrian study had a high response rate and the data were weighted, meaning that our sample is representative to the Austrian population. The comparison of the different results of other ecology of care studies has some limitations. One limitation is that the data was retrieved in different years with different data sampling methods and recruitment strategies. Also, the demographic composition of the various populations differs slightly. Further, differing definitions of the primary care sector were used. For instance, in the publication on Korea PC physician included GPs, general pediatricians, and general internists, whereas in Austria, only GPs were included. Despite this, Austria still demonstrated the highest utilization patterns. Ultimately, all studies of employed the ecology of care model and gave utilization of numbers per 1000 persons for a given timeframe of four weeks. The 1961 paper detailing the ecology of medical care is a landmark study for primary care and its position for the use of health care services and medical education [Citation2]. Using the same, well known and prominently published methodology facilitates and strengthens comparative studies and conclusions.
Conclusion
In Austria and similarly organized countries, high utilization of all levels of health care can be observed. In the case of Austria, this may be the result of competition, particularly when considering the high number of specialists working in the ambulatory sector, the very high number of hospital beds, the lack of a clear separation between the primary and secondary levels of care, and universal health coverage in the presence of unregulated access to all levels of care.
The authors conclude that establishing a clear and focused referral pathway from primary to secondary care could lead more appropriate utilization patterns in Austria, as seen in similar countries in this study. One important goal of health care is to help patients to access the appropriate point of service at the right time. At present, the lack of clarity in access and referral is a prominent contributor to the higher utilization of health care services in Austria. Engagement in the ecological model of care at all levels, particularly concerning primary care, including pre- and postgraduate as well as vocational education and health policy planning, would promote more appropriate and efficient access to care.
Ethical approval
All procedures were in accordance with the ethical standards of the responsible committee and with the Helsinki Declaration of 1975, as revised in 1983. The study procedures were approved by the ethics committee of the Medical University of Vienna (n° 988/2010).
Study trial number
The study is part of the research project ‘Ecology of Medical Care – Utilization of Health Care in Austria (ECOHCARE)’ that is registered with the ClinicalTrials.gov identifier NCT01261845.
Disclosure statement
The authors reported no conflict of interest.
Additional information
Funding
References
- White KL. The ecology of medical care: origins and implications for population-based healthcare research. Health Serv Res. 1997;32(1):11–21.
- White KL, Williams TF, Greenberg BG. The ecology of medical care. N Engl J Med. 1961;265:885–892.
- Green LA, Fryer GE, Jr., Yawn BP, et al. The ecology of medical care revisited. N Engl J Med. 2001;344(26):2021–2025.
- WHO. Declaration of Alma-Ata. WHO Chron. 1978;32(11):428–430.
- Fryer GE, Jr., Green LA, Dovey SM, et al. Variation in the ecology of medical care. Ann Fam Med. 2003;1(2):81–89.
- Hite RW. Health care in the age of ecology. Health Prog. 2003;84(6):33–36, 54.
- Kringos DS, Boerma W, van der Zee J, et al. Europe's strong primary care systems are linked to better population health but also to higher health spending. Health Aff (Millwood). 2013;32(4):686–694.
- Schafer WLA, Boerma WGW, Murante AM, et al. Assessing the potential for improvement of primary care in 34 countries: a cross-sectional survey. Bull World Health Organ. 2015;93(3):161–168.
- WHO. The World Health report: primary health care – now more than ever. Geneva: World Health Organization; 2008.
- Starfield B, Shi LY. Policy relevant determinants of health: an international perspective. Health Policy. 2002;60(3):201–218.
- Starfield B, Shi LY, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502.
- Hoffmann K, Stein KV, Maier M, et al. Access points to the different levels of health care and demographic predictors in a country without a gatekeeping system. Results of a cross-sectional study from Austria. Eur J Public Health. 2013;23(6):933–939.
- Stigler FL, Starfield B, Sprenger M, et al. Assessing primary care in Austria: room for improvement. Fam Pract. 2013;30(2):185–189.
- Hofmarcher MM, Quentin W. Austria: health system review. Health Syst Transit. 2013;15(7):1–292.
- Hoffmann K, Stein KV, Dorner TE. Differences in access points to the ambulatory health care system across Austrian federal states. Wien Med Wochenschr. 2014;164(7-8):152–159.
- Pichlhofer O, Maier M. Unregulated access to health-care services is associated with overutilization – lessons from Austria. Eur J Public Health. 2015;25(3):401–403.
- Urbas E, Költringer R. [Microcensus 1999 – Results on Health in Vienna]. Vienna: Municipality of Vienna, Department of Health Planning and Finances; 2002.
- Schnell R. Die Umstellung des LFS (labour force survey) auf RDD-CATI (random digit dialing – computer assisted telephone interviewing). Working Paper du Statec 14. Konstanz: Universität Konstanz; 2006.
- Oldendick RW, Bishop JF, Sorenson SB, et al. A comparison of the Kish and last birthday methods of respondent selection in telephone surveys. J Off Stat. 1988;4(4):307–3018.
- Ferro A, Kristiansson PM. Ecology of medical care in a publicly funded health care system: a registry study in Sweden. Scand J Prim Health Care. 2011;29(3):187–192.
- Fukui T, Rahman M, Ohde S, et al. Reassessing the ecology of medical care in Japan. J Community Health. 2017;42(5):935.
- Hansen AH, Halvorsen PA, Forde OH. The ecology of medical care in Norway: wide use of general practitioners may not necessarily keep patients out of hospitals. J Public Health Res. 2012;1(2):177–183.
- Johansen ME. Comparing medical ecology, utilization, and expenditures between 1996–1997 and 2011–2012. Ann Fam Med. 2017;15(4):313–321.
- Johansen ME, Kircher SM, Huerta TR. Reexamining the ecology of medical care. N Engl J Med. 2016;374(5):495–496.
- Kim YS, Choi YJ. The ecology of medical care in Korea. J Korean Med Sci. 2016;31(11):1684–1688.
- Shao CC, Chang CP, Chou LF, et al. The ecology of medical care in Taiwan. J Chin Med Assoc. 2011;74(9):408–412.
- Stewart M, Ryan B. Ecology of health care in Canada. Can Fam Physician. 2015;61(5):449–453.
- Takahashi O, Ohde S. The ecology of medical care in Japan Revisited. Value Health. 2014;17(7):A434.
- Leung GM, Wong IO, Chan WS, et al. The ecology of health care in Hong Kong. Soc Sci Med. 2005;61(3):577–590.
- Roncoletta A, Gusso GD, Bensenor IM, et al. A reappraisal in São Paulo, Brazil (2008) of “The Ecology of Medical Care”: the “One Per Thousand's Rule”. Fam Med. 2012;44(4):247–251.
- Shao S, Zhao F, Wang J, et al. The ecology of medical care in Beijing. PLOS One. 2013;8(12):e82446
- Duwe EA, Petterson S, Gibbons C, et al. Ecology of health care: the need to address low utilization in American Indians/Alaska Natives. Am Fam Physician. 2014;89(3):217–218.
- Kaneko M, Matsushima M, Irving G. The ecology of medical care on an isolated island in Okinawa, Japan: a retrospective open cohort study. BMC Health Serv Res. 2017;17(1):37.
- Namiki H, Kobayashi T. The ecology of medical care on the westernmost remote island, Yonaguni Island, Japan: a cross-sectional study. PLOS One. 2018;13(6):e0199871.
- Thacker SB, Greene SB, Salber EJ. Hospitalizations in a southern rural community: an application of the 'ecology model'. Int J Epidemiol. 1977;6(1):55–63.
- Vo TL, Duchesnes C, Vogeli O, et al. The ecology of health care in a Belgian area. Acta Clin Belg. 2015;70(4):280–286.
- Delamater PL, Messina JP, Grady SC, et al. Do more hospital beds lead to higher hospitalization rates? a spatial examination of Roemer's Law. PLOS One. 2013;8(2):e54900.
- Van Loenen T, Faber MJ, Westert GP, et al. Van den Berg MJ. The impact of primary care organization on avoidable hospital admissions for diabetes in 23 countries. Scand J Prim Health Care. 2016;34(1):5–12.
- OECD/EU. Health at a glance: Europe 2018: state of health in the EU cycle. Paris; 2018.
- Gulliford MC. Availability of primary care doctors and population health in England: is there an association? J Public Health Med. 2002;24(4):252–254.
- Kravet SJ, Shore AD, Miller R, et al. Health care utilization and the proportion of primary care physicians. Am J Med. 2008;121(2):142–148.
- Peersman W, Pasteels I, Cambier D, et al. Validity of self-reported utilization of physician services: a population study. Eur J Public Health. 2014;24(1):91–97.