Abstract
Objective
To investigate the association between a recorded procedure code for a medication review and adequate drug treatment management, and to explore factors associated with this code.
Design and setting
Cross-sectional study; two primary health care centres, in Region Västra Götaland, Sweden.
Subjects
A total of 302 consecutive patients (≥65 years old, 59% female; median number of drugs: six) requiring a non-urgent consultation with a physician in October–November 2017.
Main outcome measure
Adequate drug treatment management (treatment that did not require any further action), determined in consensus by two specialists in family medicine blinded to the medication review code.
Results
Adequate drug treatment management was, overall, less common in those with a recorded medication review over the last year: 63% versus 73% (p = 0.047). This negative association was evident among patients aged 65–74 years: 49% versus 74% (p = 0.003), but absent in those ≥75 years old: 67% versus 70% (p = 0.77). Recommendations from consensus included the search for additional information to be able to make a decision regarding initiation or withdrawal of a drug (n = 53), withdrawal of a drug (n = 41), or ordering a laboratory test (n = 25). Factors associated with a recorded procedure code included age above the remuneration limit of 75 years (odds ratio: 9.8; 95% confidence interval 5.0–19), type 2 diabetes (3.0 (1.5–6.2)), hypertension (2.4 (1.2–4.8)), and depression (2.5 (1.02–6.0)).
Conclusions
The presence of a recorded medication review was not positively associated with adequate drug treatment management but was associated with the age limit for remuneration, and some chronic diseases.
To improve drug treatment in older people in primary care, a remuneration system linked to recorded medication reviews has been introduced.
In this study, fewer patients with than without a recorded medication review (63% versus 73%) had adequate drug treatment management.
A recorded medication review was ten times more common in those ≥75 years, that is, the age limit for remuneration.
Recorded codes for medication reviews were also common in those with type 2 diabetes, hypertension, and depression.
Key points
Introduction
Research on medication-related problems has drawn attention to the quality of drug treatment in clinical practice. In an effort to improve the prescribing of drugs in older people, the concept of medication reviews has been introduced and established, and this intervention has been reported to have increased the quality of drug treatment [Citation1] and decrease the number of drug-related problems [Citation2]. During such a review, the physician is required to reconcile the medication and assess all drugs separately and in combination, to ascertain that the treatment is reasonable given the patient’s current health status, and carry out appropriate actions if needed.
To stimulate the performance of medication reviews in primary care, financial incentives have been introduced. For instance, in Region Västra Götaland, Sweden, primary health care centres (PHCCs) are remunerated for patients aged 75 years or older who have at least one record of a medication review, performed in the last 12-month period, in the electronic medical records [Citation3]. This is based on national guidelines declaring that medication reviews shall be performed at least annually in all patients 75 years or older who have at least five drugs in the medication list [Citation4]. The pay for performance model also includes, for instance, economic reimbursement for registering parameters concerning chronic diseases, for example, blood pressure in patients with type 2 diabetes or hypertension.
Using register data, procedure codes have not been clearly linked to quality of prescribing, as measured by national indicators of prescribing quality [Citation3]. However, as such indicators have limitations when it comes to their clinical relevance [Citation5], a deeper look into potential benefits of medication reviews is warranted. In addition, increased knowledge about medication reviews from the physician perspective is urged, reflecting the potential to improve drug treatment rather than the results of medication reviews. Indeed, the latter alternative does not take into account that patients’ perceptions have to be considered in clinical practice, and prevailing research primarily concerns medication reviews by pharmacists [Citation6]. We hypothesized that primary care patients with a recorded procedure code for a medication review over the last year would more often have adequate drug treatment management compared with those without this code, that is, treatment that does not require any further action before the next regular consultation. In addition to evaluating this hypothesis, from the perspective of the family physician, we aimed to explore factors associated with a recorded procedure code for a medication review.
Materials and methods
Design and setting
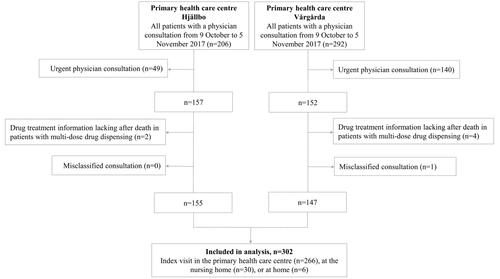
We performed a cross-sectional study using patient data from two PHCCs, Hjällbo and Vårgårda, belonging to the Swedish National Health Service in Region Västra Götaland. Hjällbo is located in a socially deprived suburb of Gothenburg and serves approximately 12,000 patients including one nursing home with 20 residents. It is staffed by 13 physicians (five specialists in family medicine, five residents in family medicine and three licensed physicians without specialist competence). Vårgårda is located in a rural area 65 km from Gothenburg, serving approximately 10,000 patients including two nursing homes with 100 residents. It is staffed by ten physicians (five specialists in family medicine, three residents in family medicine, one licensed physician without specialist competence, and one intern).
Participants
We included consecutive patients ≥65 years old requiring a non-urgent physician consultation at Hjällbo or Vårgårda, between 9 October and 5 November 2017. The consultation was either a visit to the health care centre, a consultation performed in the nursing home, or a home visit. If a patient had more than one consultation during the study period, the last one was defined as the index visit.
Data source and extraction
For each patient, an administrator prepared printouts from the electronic medical records from the last 2½ years (time limit corresponding to the introduction of a new electronic medical records system in 2015) preceding the index visit including laboratory tests, hospital discharge records, vaccinations, prescriptions and the medication list at the end of the index visit. Before the printout, filters that removed the procedure code for medication review from the index visit, if recorded, were applied. Presence of this code was recorded separately, thereby enabling blinding of the assessors for the recorded performance of a medication review during the visit where the drug treatment was extracted and assessed.
The printouts of the medical records were used to retrieve patient characteristics at the index visit regarding age, sex, residence (home or nursing home), and morbidities appearing in the Screening Tool of Older Persons’ Prescriptions (STOPP), the Screening Tool to Alert to Right Treatment (START) [Citation7] or in the set of indicators of prescribing quality for older people, provided by the Swedish National Board of Health and Welfare [Citation8]. We also extracted the most recent estimated glomerular filtration rate (eGFR) over the last year. The eGFR was usually calculated automatically in laboratory reports, using the Lund-Malmö formula [Citation9]. If eGFR was missing, we performed this calculation ourselves. In addition, we recorded whether the patient used multi-dose drug dispensing or not at the index visit, that is, machine-dispensed unit bags with drugs that should be ingested concomitantly, intended for patients who have difficulties in handling their medications.
Drug treatment at the end of the index visit was compiled, including both drugs used regularly and as needed. Drugs for topical use were included only if they have potential systemic effects. Drugs for temporary conditions, for instance infections, were only included if they appeared in any of the indicator sets. Combination drugs were counted as one drug.
Assessments
To determine if the patients’ medication was adequate, two physicians specialized in family medicine (N.P.L., S.A.S.) and clinical pharmacology (S.A.S.) performed a series of assessments, first independently and then jointly (). They first applied three sets of indicators of prescribing quality, STOPP/START version 2 [Citation7], the EU(7)-PIM list [Citation10] and the Swedish indicator set [Citation8], to alert for potentially inappropriate medications and potential prescribing omissions. These sets, described in detail in the supplemental material, provide lists of drugs that should in general be avoided in older people, and/or give recommendations of drug therapy, to avoid or to add, for specific conditions, and are all used in research [Citation11]. In the next step, the assessors determined whether an action at the end of the index visit, not performed during this visit, would have been reasonable regarding the medication. In doing so, they pictured themselves in a typical primary care setting and applied an overall medical perspective, taking into account the information available in the medical records, including morbidities and life expectancy. As mentioned, the assessors were blinded to whether the procedure code for medication review had been recorded during the index visit and they did not have access to medical records dated after this visit.
Figure 1. Flowchart of the study assessments. 1According to STOPP/START and the Swedish set of indicators of prescribing quality (supplemental material). 2At the end of the index visit. 3EU(7)-PIM list, STOPP/START, Swedish set of indicators of prescribing quality (supplemental material).
EU: European Union; PIM: potentially inappropriate medication; PPO: potential prescribing omission; START: Screening Tool to Alert to Right Treatment; STOPP: Screening Tool of Older Persons' Prescriptions.
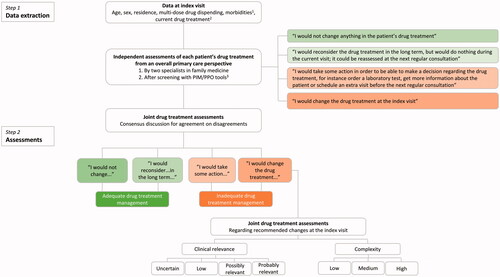
To reflect day-to-day clinical work in primary care, we used the following sentences to guide the categorization:
I would not change anything in the patient’s drug treatment;
I would reconsider the drug treatment in the long term, but would do nothing during the current visit; it could be reassessed at the next regular consultation;
I would take some action in order to be able to make a decision regarding the drug treatment, for instance order a laboratory test, get more information about the patient or schedule an extra visit before the next regular consultation; and
I would change the drug treatment at the index visit.
After all the patients’ medical records had been independently assessed, all cases, except where both assessors had made exactly the same decision, were reassessed jointly and any disagreements were resolved through consensus discussion. The actions decided in consensus were recorded. In the present study, cases where the drug treatment was jointly assessed to match above sentences (1) or (2) were collapsed into the category Adequate drug treatment management, while those matching sentences (3) or (4) were combined into an Inadequate drug treatment management category.
To shed further light on the category of ‘I would change the drug treatment’ (sentence (4)), the assessors jointly evaluated the clinical relevance and complexity of the changes in drug treatment suggested to have been performed at the index visit. For each suggested change in drug therapy, the clinical relevance of the change was categorized as uncertain, low, possibly relevant or probably relevant, reflecting the medical importance for the specific patient. The complexity was rated as low, medium or high, with ‘low’ reflecting that little physician effort was needed, and ‘high’, that a change would be more demanding, for instance requiring additional follow-up or more time for discussion with the patient.
Statistics
Data were analysed using SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY, USA). We based our sample size on findings in a pilot study [Citation12]. Based on the assumption that the proportion of patients with inadequate drug treatment management would be 15 percentage units lower in those with a recorded procedure code over the last year including the index visit, assumed to be 50%, 300 patients had to be included in the present study to yield a power of ≥80% to avoid a statistical type-II error. Therefore, we consecutively included patients from the start date until we reached about 150 patients from each PHCC. In the analyses, we compared patients with and without ≥1 recorded medication review over the last year. For categorical data, the chi-square test and Fisher’s exact test were used, and for discrete data, the Mann–Whitney test was used. As the pay for performance of medication reviews implied that PHCCs are only remunerated for reviews performed in patients ≥75 years of age, we analysed the age groups 65–74 and ≥75 years separately.
The inter-rater agreement regarding the overall medical assessment was evaluated with kappa statistics. Logistic regression was performed to obtain crude and adjusted odds ratios with 95% confidence intervals for the association between patient characteristics and ≥1 recorded medication review over the last year. In accordance with Swedish regulations and the local remuneration policy, age and number of drugs were dichotomized in these models (<75 versus ≥75 years of age; fewer than five versus five or more regular drugs in the medication list). Other patient characteristics included in the models were sex (female versus male), nursing home residence (yes versus no), and multi-dose drug dispensing (yes versus no). We also included morbidities where the prevalence differed significantly between the comparison groups in the univariate analyses. To further explore the association between patient conditions and recorded medication reviews, these morbidities were included both in a separate model and in a model where all patient characteristics were considered. The independent variables used in the logistic regression models were checked for correlations, that is, multicollinearity, using tolerance levels.
Results
In all, 302 patients were included in the study (); 178 (59%) were female and the median age was 74 years (interquartile range (IQR) 69–81, range 65–99) (). A total of 1986 drugs were included in the medication lists of 292 patients; ten (3%) patients were not receiving any drug treatment. Overall, the median number of drugs was six (IQR 3–9, range 0–20). The most common medical conditions were hypertension (n = 203, 67%), osteoarthritis (n = 91, 30%), type 2 diabetes (n = 85, 28%) and insomnia (n = 78, 26%). The eGFR was <60 and <30 mL/min in 102 (34%) and 9 (3%) patients, respectively. In 111 patients (37%), a code for a medication review was recorded at the index visit and 160 (53%) patients had one or more such codes recorded over the last year.
Table 1. Patient characteristics by presence or absence of a record of a medication review performed over the last year, overall and by age category.
The drug treatment was less often adequately managed in those with a recorded medication review (). Similar results were found in the subpopulation of patients younger than 75 years, but not in those 75 years or older. The assessors made consistent assessments in 167 (55%) patients regarding whether the drug treatment was adequately managed or not (kappa 0.33).
Table 2. Drug treatment management at the index visit, assessed in consensus by two physicians specialized in family medicine as being adequate or inadequate, by presence or absence of a record of a medication review over the last year, and by age category.
For patients with inadequate drug treatment management (n = 98), the assessors suggested a total of 182 actions at the index visit, most often to search for additional information in the medical records to be able to make a decision regarding the initiation or withdrawal of a specific drug (n = 53). Other frequently suggested actions concerned withdrawing a specific drug (n = 41) or ordering a laboratory test (n = 25). Common suggestions are described in . Proton pump inhibitors (PPIs), cyclooxygenase (COX) inhibitors, and furosemide figured most frequently, with actions suggested in 20% (18/90), 52% (17/33) and 23% (13/57) of patients, respectively.
Table 3. Common actions suggested at the index visit, by type of suboptimal treatment, in patients with inadequate drug treatment management (182 actions in 98 out of all 302 patients).
The clinical relevance of the 53 changes in drug treatment (in 43 patients), suggested to be performed directly during the index consultation, was uncertain in six patients, low in two patients, while in 23 and 22 patients, respectively, such a change was deemed to have been possibly and probably relevant. The complexity of the actions that were probably clinically relevant was judged to have been low in twelve, medium in six and high in four cases. The low-complexity actions, occurring more than once, concerned the combination of clopidogrel and omeprazole, with a suggested change to pantoprazole to avoid a potential interaction (in three patients), and a new prescription of codeine where initiating this treatment could have been avoided (in two patients). Actions of medium complexity most often concerned COX inhibitors, with a suggestion to change or withdraw the treatment (five cases). High-complexity issues concerned long-term painkillers including tramadol (in two patients) and diclofenac (one patient), and combined use of codeine and paroxetine (one patient).
Multivariate logistic regression showed that the most important factor associated with a record of a medication review was age ≥75 years (). Type 2 diabetes, hypertension, and depression were also associated with a recorded medication review. The tolerance level was >0.6 for all variables included in the models, indicating that multicollinearity was not a problem.
Table 4. Association between patient characteristics and presence of one or more recorded medication reviews over the last year.
Discussion
Main findings
In this study, we show that about two-thirds of patients with a recorded medication review, and about three in four patients without such a review, had adequate drug treatment management. The drug treatment was less often adequately managed in those with a recorded medication review. This was particularly true for patients below 75 years of age. A common reason for inadequate drug treatment management, contributing to three in 10 cases, was the lack of information in the electronic medical records, needed to make a decision concerning initiation or withdrawal of a specific drug. A record of a medication review was 10 times more common in those 75 years or older, that is, the defined limit for remuneration. It also occurred more often among patients with type 2 diabetes, hypertension, and depression.
Strengths and limitations
To the best of our knowledge, this is the first study that evaluates the association between a recorded medication review and adequate drug treatment management. Including patient data from two PHCCs with different profiles and staffed by more than 20 physicians at different career stages, the results may be generalizable, reflecting daily practice in primary care. However, prescribing practices and guidelines for medication reviews may differ within and between countries, and this may have implications for the external validity.
Another strength of this study is the drug treatment assessments that were independently performed by specialist physicians with relevant medical expertise and followed by a consensus discussion. This procedure ensures that the findings are relevant from a primary care perspective. In fact, indicators of prescribing quality, which are frequently used in this field of research, have limitations concerning their ability to reflect quality of drug treatment [Citation13], a considerable proportion not being clinically relevant at the individual level [Citation5]. Additionally, beyond limiting the assessments to what might be right or wrong based on the presence or absence of certain medications, the assessors suggested reasonable actions, taking into account the specific individual and the primary care context. For instance, a planned physician consultation for renewing a driving license may not constitute an appropriate setting for a discussion about a potentially problematic PPI treatment. Another strength of the study is that the assessors were blinded to the presence of a procedure code at the index visit. This design reduces the risk of bias in the drug treatment assessments. However, it may be regarded as a limitation that they were not blinded for recorded medication reviews over the entire year preceding the index visit. Further, the application of extensive screening tools prior to the assessments ascertained that these were performed systematically. Nevertheless, subjectivity in the assessments regarding whether the drug treatment was adequately managed or not cannot be excluded, as illustrated by the fair inter-rater agreement. The diversity in the individual assessments may not be surprising; the art of prescribing, from a family physician perspective, is complex and seldom a matter of black and white. The consensus procedure, however, is likely to increase the reliability of the results.
An important limitation is that information relevant to treatment decisions may have been known to the prescribing physician, but not fully documented in the medical records. For instance, aspects regarding the medical history and observations made during the consultation, as well as conveyed individual preferences, may be missing. Also, judging life expectancy and other ‘soft variables’ on information in medical records may be misleading. In addition, codes for medication reviews performed in the PHCC in those below the age-related remuneration limit may not have been recorded. Further, medication lists were compiled from the medical records, and in a non-negligible proportion this source has been found to be not perfectly consistent with the patients’ actual medication use [Citation14]. However, our approach reflects what is available to a family physician in day-to-day work and is arguably more realistic than using drug registers (alone or linked to other registers), which is common in studies on prescribing practices [Citation15]. Finally, although confounders were considered in the analyses, residual confounding cannot be excluded.
Findings in relation to other studies
In our study, records of at least one medication review in the previous year were present in four out of five patients aged 75 years or older. This is a considerably higher proportion compared with a study reporting increasing proportions over the first 5 years when this indicator was used for remuneration, up to 44% in 2013 [Citation3]. Conversely, only in one out of three patients below 75 years of age was such a procedure code recorded over the last year. A prominent factor associated with a code being recorded was the age limit linked with remuneration and Swedish regulations. One may thus speculate that financial compensation can have the power to influence physicians’ coding practices and direct primary health care efforts. Indeed, family physicians have been reported to perceive that Swedish regulations force them to perform medication reviews when they are actually not required to do so from a medical point of view [Citation16]. Moreover, a British study found that physicians performed medication reviews ‘in the quickest way possible to say that it was done’ [Citation17].
Our finding of a negative association between a procedure code for a medication review and adequate drug treatment management, evident in the entire cohort and particularly in those below 75 years of age, may be explained by confounding by indication and the lack of financial incentives to register medication reviews in the lower age span. For instance, specifically designated appointments for follow-up of diabetes and hypertension may have contributed to the findings; drugs are a major treatment modality for these conditions, which were both more common among those who had medication reviews recorded. Interestingly, recorded medication reviews were also associated with a depression diagnosis, perhaps reflecting the complexities related to psychiatric disease and prescribing of psychotropic medication in primary care [Citation18].
Our failure to show a positive association between a recorded medication review over the last year and adequate drug treatment management is in accordance with results of a systematic review reporting limited evidence for financial incentives to improve prescribing practices [Citation19]. In addition, a longitudinal register-based study reports comparable results regarding indicators of prescribing quality between PHCCs with high and PHCCs with low payment for recorded medication reviews [Citation3]. Moreover, educational interventions on medication reviews in primary care have not been shown to reduce acute hospital admissions or inappropriate prescriptions [Citation20]. In summary, previous evidence, combined with our blinded medical assessments at the individual level, supports that pay for performance based on the recording of codes does not have the intended effect to improve the quality of drug treatment. In a similar vein, repeated systematic reviews have failed to demonstrate beneficial effects of medication reviews on patient-relevant outcomes reflecting the net benefit-risk balance of drug treatment, that is, overall mortality and hospitalizations [Citation2,Citation21–26].
We found that several drug treatment changes that were medically relevant and of reasonably low complexity could have been performed directly during the index visit. The fact that these had not been carried out previously, or at the index visit, may reflect a lack of time to assess issues other than the main consultation reason. As discussed previously, patient-related aspects known to the family physician, but not fully documented and therefore not available to the assessors, may also explain at least some of the findings. Health care professionals in primary care work under considerable time pressure and have to prioritize their efforts in daily practice. Indeed, lack of time has recently been ranked high by health care professionals in primary care regarding the risk of medication errors [Citation27]. Further, actions that can be achieved with reasonable efforts in relation to the patient benefit have been reported to get a higher priority [Citation12]. Conversely, the withdrawal of specific drugs may conflict with patients’ demands and constitute a therapeutic dilemma for family physicians [Citation28]. The drugs most frequently found problematic at the patient level after a medical assessment have also been found to be problematic in previous research [Citation5,Citation12].
Meaning of the study
Medication reviews have been widely implemented in primary care over the last decades, and the procedure code for them has been introduced as a quality indicator to measure physician performance. Our study shows that a recorded code in primary care, reflecting that a medication review has been performed, was negatively associated with adequate drug treatment management, suggesting that this indicator does not reflect the quality of care provided. Indeed, the most prominent factor associated with a procedure code being recorded was the age limit for remuneration. These findings suggest that the administrative recording of procedure codes adds little to improve health care. Nevertheless, it cannot be excluded that the coding has other benefits, such as an increased focus on drug treatment issues and as an incentive for annual family physician–patient encounters. Indeed, although most older patients were adequately managed regarding their drug treatment, there is still room for improvement. Further research exploring the potential benefits of medication reviews, and perhaps also the perceptions of coding such efforts, from the perspectives of the family physician and the patients could be valuable.
Ethical approval
The study was approved by the Regional Ethical Review Board in Gothenburg, Sweden (DRN: 1046-15). Informed consent was waived by the Board.
Supplemental Material
Download MS Word (56.9 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Skjøt-Arkil H, Lundby C, Kjeldsen LJ, et al. Multifaceted pharmacist-led interventions in the hospital setting: a systematic review. Basic Clin Pharmacol Toxicol. 2018;123(4):363–379.
- Huiskes VJ, Burger DM, van den Ende CH, et al. Effectiveness of medication review: a systematic review and meta-analysis of randomized controlled trials. BMC Fam Pract. 2017;18(1):5.
- Ödesjö H, Anell A, Boman A, et al. Pay for performance associated with increased volume of medication reviews but not with less inappropriate use of medications among the elderly - an observational study. Scand J Prim Health Care. 2017;35(3):271–278.
- Swedish National Board of Health and Welfare. Handling and prescribing of drugs in health care [HSLF-FS 2017:37. Socialstyrelsens föreskrifter och allmänna råd om ordination och hantering av läkemedel i hälso- och sjukvården]. 2017.
- Lönnbro J, Wallerstedt SM. Clinical relevance of the STOPP/START criteria in hip fracture patients. Eur J Clin Pharmacol. 2017;73(4):499–505.
- Khalil H, Bell B, Chambers H, et al. Professional, structural and organisational interventions in primary care for reducing medication errors. Cochrane Database Syst Rev. 2017;10(10):CD003942.
- O'Mahony D, O'Sullivan D, Byrne S, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213–218.
- Fastbom J, Johnell K. National indicators for quality of drug therapy in older persons: the Swedish experience from the first 10 years. Drugs Aging. 2015;32(3):189–199.
- Nyman U, Grubb A, Larsson A, et al. The revised Lund-Malmö GFR estimating equation outperforms MDRD and CKD-EPI across GFR, age and BMI intervals in a large Swedish population. Clin Chem Lab Med. 2014;52(6):815–824.
- Renom-Guiteras A, Meyer G, Thürmann PA. The EU(7)-PIM list: a list of potentially inappropriate medications for older people consented by experts from seven European countries. Eur J Clin Pharmacol. 2015;71(7):861–875.
- Pazan F, Kather J, Wehling M. A systematic review and novel classification of listing tools to improve medication in older people. Eur J Clin Pharmacol. 2019;75(5):619–625.
- Parodi López N, Wallerstedt SM. Quality of prescribing in older people from a broad family physician perspective: a descriptive pilot study. BMJ Open. 2019;9(6):e027290.
- Wallerstedt SM, Belfrage B, Fastbom J. Association between drug-specific indicators of prescribing quality and quality of drug treatment: a validation study . Pharmacoepidemiol Drug Saf. 2015;24(9):906–914.
- Säfholm S, Bondesson Å, Modig S. Medication errors in primary health care records; a cross-sectional study in Southern Sweden. BMC Fam Pract. 2019;20(1):110.
- Wallerstedt SM, Wettermark B, Hoffmann M. The first decade with the Swedish prescribed drug register - a systematic review of the output in the scientific literature. Basic Clin Pharmacol Toxicol. 2016;119(5):464–469.
- Schmidt-Mende K, Hasselstrom J, Wettermark B, et al. General practitioners' and nurses' views on medication reviews and potentially inappropriate medicines in elderly patients - a qualitative study of reports by educating pharmacists. Scand J Prim Health Care. 2018;36(3):329–341.
- Duncan P, Cabral C, McCahon D, et al. Efficiency versus thoroughness in medication review: a qualitative interview study in UK primary care. Br J Gen Pract. 2019;69(680):e190–e198.
- Hedenrud TM, Svensson SA, Wallerstedt SM. "Psychiatry is not a science like others" - a focus group study on psychotropic prescribing in primary care. BMC Fam Pract. 2013;14:115.
- Rashidian A, Omidvari AH, Vali Y, et al. Pharmaceutical policies: effects of financial incentives for prescribers. Cochrane Database Syst Rev. 2015;(8):CD006731.
- Schmidt-Mende K, Andersen M, Wettermark B, et al. Educational intervention on medication reviews aiming to reduce acute healthcare consumption in elderly patients with potentially inappropriate medicines-a pragmatic open-label cluster-randomized controlled trial in primary care. Pharmacoepidemiol Drug Saf. 2017;26(11):1347–1356.
- Lehnbom EC, Stewart MJ, Manias E, et al. Impact of medication reconciliation and review on clinical outcomes. Ann Pharmacother. 2014;48(10):1298–1312.
- Alldred DP, Kennedy MC, Hughes C, et al. Interventions to optimise prescribing for older people in care homes. Cochrane Database Syst Rev. 2016;2:CD009095.
- Abbott RA, Moore DA, Rogers M, et al. Effectiveness of pharmacist home visits for individuals at risk of medication-related problems: a systematic review and meta-analysis of randomised controlled trials. BMC Health Serv Res. 2020;20(1):39.
- Rankin A, Cadogan CA, Patterson SM, et al. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev. 2018;9(9):CD008165.
- Tecklenborg S, Byrne C, Cahir C, et al. Correction to: interventions to reduce adverse drug event-related outcomes in older adults: a systematic review and meta-analysis. Drugs Aging. 2020;37(2):147–147.
- Holland R, Desborough J, Goodyer L, et al. Does pharmacist‐led medication review help to reduce hospital admissions and deaths in older people? a systematic review and meta‐analysis. Br J Clin Pharmacol. 2008;65(3):303–316.
- Fernholm R, Wachtler C, Malm-Willadsen K, et al. Validation and initial results of surveys exploring perspectives on risks and solutions for diagnostic and medication errors in primary care in Sweden. Scand J Prim Health Care. 2020;38(4):381–390.
- Carrier H, Zaytseva A, Bocquier A, et al. GPs' management of polypharmacy and therapeutic dilemma in patients with multimorbidity: a cross-sectional survey of GPs in France. Br J Gen Pract. 2019;69(681):e270–e278.