Abstract
Objectives
The study aimed to find whether Örebro Musculoskeletal Pain Screening Questionnaire (ÖMPSQ) predicts the severity of fibromyalgia symptoms after one year in patients with fibromyalgia. The second aim of the study was to observe how symptoms evolved during a one-year follow-up.
Design
Prospective cohort and observational study. Five questionnaires were sent to patients. The same questionnaires (excluding ÖMPSQ) were sent after one year. The patients were allocated into two cohorts using the results of ÖMPSQ. Other variables were analyzed and observed separately.
Setting
Primary healthcare center in the city of Nokia, Pirkanmaa, Finland
Subjects
Patients with fibromyalgia were included in the study after a physician’s examination and confirmation of diagnosis with the assistance of the American College of Rheumatology (ACR) 2010 criteria.
Main outcome measures
Fibromyalgia impact questionnaire (FIQ) scores
Results
The FIQ scores increased slightly in both ÖMPSQ-cohorts with no statistically significant differences. The patients mostly reported that the symptoms were unchanged or got worse when asked separately from other questionnaires. There was a statistically significant decrease in PHQ-9 score in depressed patients who received antidepressants and/or psychological therapy. In addition, FIQ scores also decreased in depressed patients. Patients who received alterations to the treatment plan reported positive changes in the symptoms more often.
Conclusion
With these results, we cannot conclude that ÖMPSQ predicts the patient’s severity of symptoms. On the contrary, we can conclude that antidepressants and/or psychological therapy might reduce fibromyalgia symptoms for depressed patients with fibromyalgia. Patients with fibromyalgia might benefit from clinical evaluation and modifications to the treatment plan if necessary.
KEY POINTS
The long-term prognosis is not well known, and there are limited tools to predict the development of symptoms.
ÖMPSQ does not seem to be useful for predicting the development of fibromyalgia in patients who already have been diagnosed with fibromyalgia.
Management of depression for patients with fibromyalgia might be effective in reducing fibromyalgia symptoms.
Patients with fibromyalgia in Finnish healthcare center – one-year follow-up.
1. Introduction
Fibromyalgia is a functional syndrome characterized by centralized pain which is widespread, and often there are other symptoms including fatigue, memory problems as well as mood and sleep issues [Citation1]. The prevalence of fibromyalgia varies from 2 to 8% of the population [Citation1]. There is overlap with other functional syndromes [Citation2]. Commonly used criteria to assess patients with fibromyalgia are American College of Rheumatology (ACR) criteria for fibromyalgia which have been validated and are updated regularly [Citation3]. The definitive diagnosis is based on a clinical examination. Cognitive-affective factors like pain catastrophizing and fear-avoidance correlate with functional status and quality of life in patients with fibromyalgia [Citation4,Citation5].
One tool to assess fibromyalgia symptoms is the Fibromyalgia impact questionnaire (FIQ) which is a multidimensional questionnaire. It evaluates the quality of life and the ability to function physically in daily activities. It is useful for assessing the progress and status of a patient and especially for quantifying the changes during the course of the disease [Citation6,Citation7].
Questionnaires have been developed to estimate the probability of musculoskeletal pain becoming chronic. One of these is Örebro Musculoskeletal Pain Screening Questionnaire (ÖMPSQ) [Citation8]. For example, it has been used to identify patients at risk of developing chronic back pain [Citation9]. It also takes into account the psychosocial aspects of pain [Citation9]. Furthermore, research suggests that the questionnaire is valid in primary healthcare and different cultural environments [Citation10]. Finally, ÖMPSQ has been used and proven to be effective at estimating mild/moderate traffic injuries becoming chronic [Citation11]. There is a 25-item long version and a 10-item short version of the questionnaire. Psychological factors measured with ÖMPSQ have some predictive value in perceived physical health after three years of treatment for non-acute pain [Citation12].
It is important to identify the correct patients and provide effective health care. A Dutch study found that patients with severe symptoms of fibromyalgia benefitted the greatest from multimodal rehabilitation [Citation13]. Another study found that strong pain-related self-efficacy and treatment adherence predicted less disability and pain [Citation14]. However, there is a lack of research on predicting the course of the disease with ÖMPSQ. This study aimed to find whether ÖMPSQ predicts the severity of symptoms after one year in patients with fibromyalgia. This may give us valuable information on what intervention methods to use with patients. Because cognitive-affective factors like pain catastrophizing and fear-avoidance correlate with functional status and quality of life in patients with fibromyalgia we hypothesized that ÖPMSQ would be useful for predicting symptom severity in one-year follow-up. The second aim of the study was to describe how symptoms evolved during a one-year follow-up in different groups of patients.
2. Material and methods
This is a prospective cohort and observational study. At the time when the material was gathered (2016), the city of Nokia had 33,210 inhabitants and 19 physicians were working at the primary healthcare center of Nokia. The patients were identified from an electronic patient record.
The inclusion criteria included an ICD-10 diagnosis for fibromyalgia (M79.7). In addition, any patient with ICD-10 codes M79.0 (Rheumatism, unspecified), M25.5 (Pain in joint), R52.2 (Other chronic pain) or R52.9 (Pain, unspecified) was included, if the patient had ‘fibromyalgia’ or ‘fibrositis’ written in the patient record. Additional inclusion criteria were the following: ability to read, write and speak Finnish and the age of 18 years.
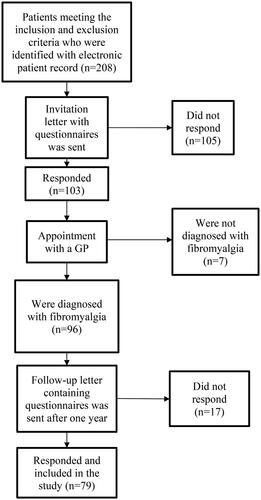
The exclusion criteria were the following: severe cognitive disability (e.g. Alzheimer’s disease), any psychotic disorder and unstable physical condition (e.g. metastatic cancer). Lactating and pregnant patients were also excluded. After the inclusion and exclusion criteria were met, 208 patients were identified. Patient recruitment is shown in .
A letter with five questionnaires was sent to the identified patients. The letter included FIQ, ÖMPSQ, ACR 2010, EuroQol (EQ-5D-3L), and Patient Health Questionnaire (PHQ-9) in Finnish language [Citation8,Citation15–17]. The results of EuroQol-questionnaire were not included in the study and ÖMPSQ was the 25-item version. There were 103 (50%) responders. Patients with clinically significant symptoms of depression based on a PHQ-9 score of ten or more and a clinical examination were classified as depressed.
The patients that responded (n = 103), had an appointment with a physician. At the appointment, the physician filled out an additional ACR 2010 questionnaire with the patient to assist the physician in the diagnosis. Furthermore, a clinical examination was performed, and the diagnosis was primarily based on it. After the appointment, a total of 96 (93%) patients were included. All patients who had clinically significant symptoms of depression received treatment for depression according to guidelines which included psychotherapy or medication or both.
The patients meeting the ACR 2010 criteria (n = 96) received another letter containing the same questionnaires except for ÖMPSQ after one year. In addition, the patients received a question that aimed to find out the patient’s perception of the development of fibromyalgia. The patients were asked whether the symptoms got worse, stayed the same or got better. Finally, they were asked whether there were any alterations made to the treatment plan during the appointment where the physician assessed the patient’s eligibility for the study. Altogether 79 (82%) patients returned the letter and were included in the study.
The patients that returned the follow-up letter were divided into two groups using the ÖMPSQ score with a cut-off score of 80. By using this cut-off score, ÖMPSQ had a sensitivity of 88% and specificity of 63% for predicting the functional ability of a patient, according to Linton SJ, Boersma K [Citation9]., and was therefore proposed by us. The outcome variable analyzed was the FIQ score. The patient’s FIQ score in the follow-up letter was compared to the FIQ score in the initial letter. In addition, the change in FIQ score was categorized into patients with and without depression. The changes in the perception of symptoms were observed in groups separated by sex, time of diagnosis, the presence of depression symptoms and whether a physician had made any alterations to the treatment plan.
The data were analyzed with SPSS version 28. Paired sample t-test was used for analyzing the relation between the main variables. Univariate logistic regression was used to analyze the relationship between the alteration of the treatment plan, depression and the perception of improvement of symptoms. All variables were normally distributed. Crosstabulations were analyzed with chi-square test. Confidence intervals (95% CI) and p-values were calculated for all results. A p-value under 0.05 was considered statistically significant.
3. Results
The responding group (n = 103) to the invitation letter did not have statistically significant differences compared to the group not responding (n = 105) when taking demographic features and patient history into consideration (detailed analysis is presented in ). All patients had not filled out every form properly. For this reason, the number of total patients in the analyses is lower than 79, which is the number of participants. The symptoms in both ÖMPSQ groups got worse after one year, which was the duration of the study. The FIQ score in the group with ÖMPSQ score of more than 80 points increased to a greater extent, but no statistically significant differences were observed (FIQ scores are presented in ). The patient’s perception of the symptoms of fibromyalgia got worse in 45% of the patients, stayed the same in 50% of the patients, and got better in 5% of the patients (detailed analysis is presented in ). The PHQ-9 scores decreased and the decrease by 1.0 points (95% CI −2.1 − 0.1) was not statistically significant in the overall population, but there was a statistically significant decrease by 3.2 points (95% CI −4.8 to −1.5) in depressed patients. The perception of symptoms changed statistically significantly in the two groups. It was found that the odds of improvement of the perception of symptoms increased by an odds ratio of 9.6 (95% CI 1.2 − 78.9) for patients whose treatment plan was modified (perception of symptoms got better = 1, stayed the same or got worse = 0). It was also found that the odds of the perception of symptoms getting worse or staying the same increased by an odds ratio of 2.7 (95% CI 1.1 − 6.7) for depressed patients defined by PHQ-9 score of ten or more (perception of symptoms got worse or stayed the same = 1, got better = 0).
Table 1. Comparison between the participants who returned the invitation letter and non-participants.
Table 2. FIQ scores for the main Cohorts and for depressed patients and patients without depression.
Table 3. The change in perception of fibromyalgia symptoms after one-year follow-up.
4. Discussion
We did not find a statistically significant difference in FIQ score between the two groups divided with ÖPMSQ score. However, the mean FIQ score rose more in the group with a high ÖMPSQ score. With these results, we cannot conclude that ÖMPSQ predicts the patient’s severity of symptoms after one year among patients who had already been diagnosed with fibromyalgia. After all, ÖMPSQ was originally developed to predict whether the pain becomes chronic and in fibromyalgia chronic pain is one of the main features of the syndrome. We found that making alterations to the treatment plan was useful. We can also conclude that depression treatment was effective because the PHQ-9 score decreased significantly in depressed patients, all of whom were treated for depression. On the other hand, the perception of symptoms got worse among depressed patients. This may be due to memory bias in depressed patients.
The main limitation of the study is the relatively low number of participants. In addition, the information was gathered only from one healthcare center. This may limit the generalizability of the results. Furthermore, the participation rate was not ideal (about 50%). However, the participants did not differ from the non-participants. In contrast, the follow-up questionnaires were returned at a greater rate (about 80%). FIQ does have some bias regarding wealthy women and more disabled people; therefore, a revised fibromyalgia impact questionnaire (FIQR) has been developed to address these issues [Citation6,Citation7]. However, at the time of our study, FIQR was not validated and available in Finnish. It is reasonable to assume that people in Finland are able to perform the daily activities included in FIQ regardless of socioeconomic status. However, our study did not include data on disability status, which may bias the results in either direction. Based on research many patients with fibromyalgia have also anxiety symptoms and these overlap with depression. We did not screen for anxiety disorders but in future studies, it would be beneficial because anxiety is common in this population of patients where psychiatric conditions are common. It is not possible to separate the effect from the treatment of depression and the improvement of fibromyalgia symptoms overall. Therefore, we do not know how much of the improvement in FIQ is explained by a reduction in the depression item and this is a subject for further studies. One strength of the study is that the diagnosis was confirmed by a physician after a thorough examination. In addition, the study also included male participants.
The estimated minimal clinically important difference (MCID) in FIQ score is 14% [Citation18]. In our study, the FIQ score changed by two to four percent which is not clinically significant. This may explain the low number of patients who reported positive changes in the symptoms of fibromyalgia. In a 15-year-long prospective study, the patient’s perception of the symptoms had improved slightly or significantly [Citation19]. The same kind of results can be found in another prospective study as well [Citation20]. Our results were different because patients mostly reported neutral or negative changes in symptoms.
In summary, we could not determine whether ÖMPSQ is effective at predicting the course of disease in patients with a previous fibromyalgia diagnosis. However, the identification and management of depressed fibromyalgia patients is probably beneficial to reduce fibromyalgia symptoms.
Ethics statement
The study plan has been approved by The Regional Ethics Committee of Tampere University Hospital. (R15041)
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from Nokia Healthcare Center but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of Nokia Healthcare Center.
Additional information
Funding
References
- Clauw DJ. Fibromyalgia: a clinical review. JAMA. 2014;311(15):1547–1555. doi: 10.1001/jama.2014.3266.
- Borchers AT, Gershwin ME. Fibromyalgia: a critical and comprehensive review. Clin Rev Allergy Immunol. 2015;49(2):100–151. doi: 10.1007/s12016-015-8509-4.
- Wolfe F, Clauw DJ, Fitzcharles MA, et al. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 2016;46(3):319–329. doi: 10.1016/j.semarthrit.2016.08.012.
- Martínez MP, Sánchez AI, Miró E, et al. The relationship between the fear-avoidance model of pain and personality traits in fibromyalgia patients. J Clin Psychol Med Settings. 2011;18(4):380–391. doi: 10.1007/s10880-011-9263-2.
- Van Wilgen CP, Van Ittersum MW, Kaptein AA, et al. Illness perceptions in patients with fibromyalgia and their relationship to quality of life and catastrophizing. Arthritis Rheum. 2008;58(11):3618–3626. doi: 10.1002/art.23959.
- Kaltsas G, Tsiveriotis K, et al. Fibromyalgia. In: feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, editors. Endotext. [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000 [cited 2022 Jul 1]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK279092/
- Bennett RM, Friend R, Jones KD, et al. The revised fibromyalgia impact questionnaire (FIQR): validation and psychometric properties. Arthritis Res Ther. 2009;11(4):R120. doi: 10.1186/ar2783.
- Questionnaires - Örebro University. [Internet]. [cited 2022 May 23]. Available from: https://www.oru.se/english/research/research-environments/hs/champ/questionnaires/.
- Linton SJ, Boersma K. Early identification of patients at risk of developing a persistent back problem: the predictive validity of the örebro musculoskeletal pain questionnaire. Clin J Pain. 2003;19(2):80–86. doi: 10.1097/00002508-200303000-00002.
- Maher CG, Grotle M. Evaluation of the predictive validity of the Orebro musculoskeletal pain screening questionnaire. Clin J Pain. 2009;25(8):666–670. doi: 10.1097/AJP.0b013e3181a08732.
- Gopinath B, Jagnoor J, Nicholas M, et al. Presence and predictors of persistent pain among persons who sustained an injury in a road traffic crash: pain outcomes related to road traffic crash injuries. Eur J Pain. 2015;19(8):1111–1118. doi: 10.1002/ejp.634.
- Westman A, Linton SJ, Öhrvik J, et al. Do psychosocial factors predict disability and health at a 3-year follow-up for patients with non-acute musculoskeletal pain? A validation of the örebro musculoskeletal pain screening questionnaire. Eur J Pain. 2008;12(5):641–649. doi: 10.1016/j.ejpain.2007.10.007.
- Van Abbema R, Van Wilgen CP, Van Der Schans CP, et al. Patients with more severe symptoms benefit the most from an intensive multimodal programme in patients with fibromyalgia. Disabil Rehabil. 2011;33(9):743–750. doi: 10.3109/09638288.2010.510177.
- Dobkin PL, Liu A, Abrahamowicz M, et al. Predictors of disability and pain six months after the end of treatment for fibromyalgia. Clin J Pain. 2010;26(1):23–29. doi: 10.1097/AJP.0b013e3181b40ee6.
- Burckhardt CS, Clark SR, Bennett RM. The fibromyalgia impact questionnaire: development and validation. J Rheumatol. 1991;18(5):728–733.
- Wolfe F, Clauw DJ, Fitzcharles MA, et al. The American college of rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken). 2010;62(5):600–610. doi: 10.1002/acr.20140.
- Arroll B, Goodyear-Smith F, Crengle S, et al. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med. 2010;8(4):348–353. doi: 10.1370/afm.1139.
- Bennett RM, Bushmakin AG, Cappelleri JC, et al. Minimal clinically important difference in the fibromyalgia impact questionnaire. J Rheumatol. 2009;36(6):1304–1311. doi: 10.3899/jrheum.081090.
- Kennedy M, Felson DT. A prospective long-term study of fibromyalgia syndrome. Arthritis Rheum. 1996;39(4):682–685. doi: 10.1002/art.1780390422.
- White KP, Nielson WR, Harth M, et al. Does the label “fibromyalgia” alter health status, function, and health service utilization? A prospective, within-group comparison in a community cohort of adults with chronic widespread pain. Arthritis Rheum. 2002;47(3):260–265. doi: 10.1002/art.10400.