Abstract
Purpose. To estimate retrospectively the rate of isolated nodal failures (INF) in NSCLC patients treated with the elective nodal irradiation (ENI) using 3D-conformal radiotherapy (3D-CRT). Materials/methods. One hundred and eighty-five patients with I-IIIB stage treated with 3D-CRT in consecutive clinical trials differing in an extent of the ENI were analyzed. According to the extent of the ENI, two groups were distinguished: extended (n=124) and limited (n=61) ENI. INF was defined as regional nodal failure occurring without local progression. Cumulative Incidence of INF (CIINF) was evaluated by univariate and multivariate analysis with regard to prognostic factors. Results. With a median follow up of 30 months, the two-year actuarial overall survival was 35%. The two-year CIINF rate was 12%. There were 16 (9%) INF, eight (6%) for extended and eight (13%) for limited ENI. In the univariate analysis bulky mediastinal disease (BMD), left side, higher N stage, and partial response to RT had a significant negative impact on the CIINF. BMD was the only independent predictor of the risk of incidence of the INF (p=0.001). Conclusions. INF is more likely to occur in case of more advanced nodal status.
The role of the elective nodal irradiation (ENI) in the treatment of non-small cell lung cancer (NSCLC) is a controversial issue. Number of isolated nodal failures (INF) is estimated to be as low as 6–15%, usually below 10% Citation[1–7]. On the other hand, the incidence of unforeseen nodal metastases in stage I NSCLC may be as high as 25% in surgical series Citation[8], Citation[9]. Data on the incidence of INF are mainly taken from studies on dose escalation or stereotactic radiotherapy with highly selected groups Citation[1–3], Citation[5], Citation[7], Citation[10]. In these studies patients were treated with omission of the ENI Citation[1–7], Citation[11] or patients treated with ENI represented small (13%) percentage Citation[10].
As postulated by Jeremic Citation[12], the prerequisite condition for reporting on incidence of INF after radiotherapy with omission of the ENI is an evaluation of incidental irradiation by omitted lymph node stations (LNS). Recent publication by Chapet et al. Citation[13] providing recommendations on the definition of the borders of mediastinal and hilar LNS in the CT produced an opportunity of detailed reporting on intended and non-intended doses received by particular LNS.
There are no data in the literature on the incidence of INF in the series of patients receiving the 3D-planned ENI. Our study was undertaken in view of the retrospective evaluation of INF in relation to the dose received by particular LNS and prognostic factors in consecutive patients treated with precisely defined extent of the 3-D planned ENI.
Patients and methods
Patients
Consecutive 207 NSCLC patients treated with definitive entirely 3D-planned conformal radiotherapy (3D-CRT) between 1998 and 2004 by one of the authors (LK) were considered. Twenty-two patients were excluded. Reasons of exclusion were following: no CT of the chest performed during follow-up (12), technical problems with recovering of initial treatment plans (6), major deviations in the treatment delivery (4). Final analysis is based on 185 patients. Characteristics of the group are summarized in .
Table I. Characteristics of group.
Patients were staged according to the American Joint Commission on Cancer (AJCC) 1997 Staging System. Initial staging consisted of a history and medical examinations, routine blood tests, chest x-ray, bronchoscopy, chest CT with upper abdomen, and pulmonary function tests. Bone scan and CT or MRI of the brain were done only in case of clinical suspicion of metastases. No patient had positron emission tomography (PET) done for an initial staging. Only 5% of patients underwent mediastinoscopy. Twenty-nine percent of patients had bulky mediastinal disease (BMD), which was defined as involvement of three or more LNS or enlargement of the single lymph node to 3 cm or more. According to the institutional policy, fit and less than 70 years old stage III patients received 2–3 cycles of platinum based chemotherapy before radiotherapy.
Radiotherapy planning and targets volumes definition
Patients were included in the consecutive clinical trials. According to the extent of the elective nodal irradiation (ENI), two groups were distinguished retrospectively: extended ENI–124 patients (all stages) and limited ENI–61 patients (all but one with III stage). The patients receiving extended ENI were treated according to the following schedules: 66–74 Gy delivered in 2 Gy per fraction over 6.5–7.5 weeks (n = 64), 57 Gy delivered in 1.2–1.8 Gy per fraction b.i.d in 4 weeks (n = 39), 60 Gy in 1.5 Gy per fraction 3 times a day over 2.5 weeks (n = 21); doses prescribed to the elective Planning Target Volume (PTVelect) varied between 39 Gy over 1.5–4 weeks and 54 Gy over 5.5 weeks, median: 50 Gy.
The patients treated with limited ENI received 56.7–58.8 Gy delivered in 2.7–2.8 Gy per fraction over 4 weeks using simultaneous integrated boost technique. Dose to the PTVelect was 39.9 Gy delivered in 1.9 Gy per fraction over 4 weeks.
The GTV (Gross Tumor Volume) was defined for each group as tumor volume visualized in CT and endobronchial extension as described in bronchoscopy. All lymph nodes with the diameter ≥ 1 cm in short axis in CT were included in GTV. For patients receiving chemotherapy, the initially involved LNS were always included in the GTV regardless of the type of the treatment response obtained. Some reductions of the GTV volume were possible within pulmonary parenchyma in case of response to chemotherapy of the primary tumor.
There were two types of CTV (Clinical Target Volume): CTVelect and CTVboost. CTVboost was defined as GTV with 0.5 cm margin within pulmonary parenchyma, and whole nodal station was delineated for CTV of lymph nodes considered as pathologic. An elective CTV (CTVelect) differed for two analysed groups. The nomenclature of hilar and mediastinal LNS as proposed by Mountain and Dressler Citation[14] was mandatory during a treatment planning and is in use in this study [ and ]. CTVelect in the group with extended ENI comprised ipsilateral hilum, 2R, 2L, 3A, 3P, 4R, 4L, groups 5, 6, 7, and group 8 for tumours located in the lower lobes. For group with limited ENI the LNS with the highest probability of microscopic invasion only were included in the CTVelect; namely ipsilateral hilum, 4R, 4L, group 7, and group 5 for left side. Differences in the definition of the CTVelect for extended and limited ENI are shown in the .
Figure 1. Schema of Mountain and Dressler mediastinal and hilar lymph node stations classification system, after Mountain and Dressler Citation[14].
![Figure 1. Schema of Mountain and Dressler mediastinal and hilar lymph node stations classification system, after Mountain and Dressler Citation[14].](/cms/asset/c388c2d5-995a-4646-b6be-5b16adb18eca/ionc_a_244067_f0001_b.gif)
Figure 2. Differences in delineation of the CTVelect for extended (brown and green color on axial and coronal sections, respectively) and limited ENI (violet and red color on axial and coronal sections, respectively).
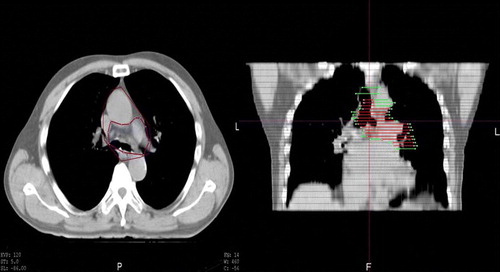
Table II. Classification of hilar and mediastinal Lymph Nodes Stations according to Mountain and Dressler classification Citation[14].
PTV boost and PTVelect were created by adding margins of 1 cm to the respective CTVs. Margins for PTVs were adapted, if necessary, for respiratory motion as visualized under fluoroscopy. Dose was specified to the ICRU point. Treatment was entirely 3D-planned, dose homogeneity criteria within respective PTVs had to be within 95–107% of the prescribed dose. Mean dose for lung had to be kept at or below 20 Gy (exceptionally 22 Gy). Treatment was delivered on linear accelerators with 4–15 MV photons.
Follow-up
As patients were enrolled in consecutive clinical trials, they were followed on regular basis, with visits 1 month following treatment, next every 3 months during first 2 years, and every 6 months thereafter. Chest x-rays were performed at every visit, CT of the chest every 6 months or more frequently at the suspicion of progression. Acute and late pulmonary toxicity were scored according to SWOG Citation[15] and RTOG/EORTC scale Citation[16], respectively.
Evaluation of doses received by lymph node stations (LNS) – sites of INF
For patients with INF the particular LNS were delineated by one author (LK). The special attention was paid, if there were no geographical misses of the nodal disease in the sites of INF. The LNS were delineated according to the recommendations of the Atlas from the University of Michigan Citation[13]. The separate cumulative dose volume histograms (DVH) were created from initial dose prescriptions. For LNS where the INF occurred the minimum and maximum doses were considered.
Radiation dose is considered in this study as the physical dose. Otherwise, there was no biological dose equivalent done for accelerated treatment, and/or low doses per fraction of the incidental irradiation.
Endpoints and statistical analysis
Isolated nodal failure (INF) was defined as a nodal failure outside initially involved lymph nodes without previous or synchronous local progression regardless distant metastases status.
Local progression was scored as enlargement of initial (primary or nodal) abnormalities on CT (any abnormalities on chest x-ray were verified by CT). Lack of the progression of the residual disease during at least 6 months following treatment was accepted as a sign of local control. Kaplan-Meier method was used for an estimation of overall survival and Cumulative Incidence of INF (CIINF). For CIINF deaths, local progressions and last observations without occurrence of INF were censored observations. Univariate analysis was used for an evaluation of relation of patient, tumour, and treatment characteristics to the CIINF. Factors related to the CIINF with significance tested by log-rank at p ≤ 0.2 were evaluated in the multivariate analysis (Cox proportional hazards model).
The times for survival and CIINF were calculated from the start of radiotherapy.
Results
Overall survival, local progression, distant metastases, lung doses and pulmonary toxicity
Median follow-up for living patients was 30 months (range: 15–86). The mean PTVelect for limited and extended ENI were 583 cc and 591 cc, respectively. This lack of significant reduction of the volume treated with more limited elective area was related to more advanced stages of patients treated with limited ENI (39% vs. 23% of BMD for limited vs. extended ENI, p < 0.05). The two-year actuarial survival rate was 35%. No one of four treatment schedules used in the presented study gave different results in terms of overall survival. Local progression and distant metastases occurred respectively in 104 (56%) and 79 (43%) patients as any component of failure. The mean lung doses were 17 Gy and 19 Gy for patients treated with limited and extended ENI, respectively. Acute and late pulmonary toxicities were mild and there was no difference for both analyzed groups. There was one death attributed to acute lung toxicity in the extended ENI group. Besides this, there were 20% and 15% of cases of grade 1–2 acute pulmonary toxicity for extended and limited ENI, respectively. For late pulmonary toxicity, 6% of patients in each of both analyzed extents of the ENI experienced the highest observed grade 3 toxicity.
Isolated nodal failures
There were no geographical misses of the nodal disease, according to the criteria of inclusion of the lymph nodes in the GTV. Isolated nodal failure (INF) defined as above was found in 16 (9%) patients. The two-, and three-year CIINF rates were 12% and 14%, respectively. summarizes characteristics of cases with INF. Diagnostics of INF were done between 3 and 63 months (median: 7.5 months). Nine of 16 INF were located exclusively outside CTVelect. Minimum doses in the LNS not included in the CTVelect, where INF occurred ranged from 0 to 42 Gy (median: 3 Gy); only in 1 case the minimum dose was ≥ 40 Gy. Minimum doses for 7 INF that occurred in the LNS included in the CTVelect, ranged from 29 to 58 Gy (median: 50 Gy).
Table III. Characteristics of cases with the Isolated Nodal Failures (INF).
INF occurred in the regions receiving doses < 40 Gy in 11 (69%) of 16 cases, whilst in the regions receiving doses ≥ 40 Gy in 5 (31%) of 16 cases, p = 0.04.
There were 8 (6%) INF for 124 patients with extended ENI and 8 (13%) for 61 patients with limited ENI. For 96 stage III patients undergoing extended ENI there were seven INF (7%), whilst in 60 III stage patients with limited ENI there were seven INF (12%), p = 0.3.
In 8 (50%) of 16 patients with INF distant metastases occurred before, simultaneously or up to 3 months after diagnosis of INF.
Results of univariate analysis for relation of prognostic factors to the CIINF are summarized in . There was a statistically significant relation of bulky mediastinal disease (BMD) (), side (left or right), N stage, and response to radiotherapy with incidence of INF. In the multivariate analysis, the risk of INF was related only to the presence of BMD, RR–5.88, 95% CI–1.92–20.00, p = 0.002. When the variable of BMD was not included in the Cox model, the N stage was the only independent predictor of INF, RR–2.57, 95% CI–1.30–5.08, p = 0.004. The two-year CIINF rate for patients with N3 disease was 47%. Since the BMD is expected to be associated with the high risk of distant metastases, we have checked whether there were any disease-free survivals among those patients. Among 53 patients with BMD there were 7 (13%) patients alive free of disease at last observation.
Figure 3. Cumulative incidence of Isolated Nodal Failures in relation to the presence of the bulky Mediastinal Disease (BMD) [bold line - presence of BMD, dashed line - absence of BMD].
![Figure 3. Cumulative incidence of Isolated Nodal Failures in relation to the presence of the bulky Mediastinal Disease (BMD) [bold line - presence of BMD, dashed line - absence of BMD].](/cms/asset/64b2ef99-7d05-4bb1-a195-14ca040fa920/ionc_a_244067_f0003_b.gif)
Table IV. Results of univariate analysis for Cumulative Incidence of the INF (CIINF).
Discussion
The rate of 9% of INF shown in this study was similar to the results from the series with the similar follow-up where the ENI was omitted or was given to small percentage of patients Citation[1–7], Citation[11], Citation[17], Citation[18]. The similar rate of INF in our study as in the series with omission of the ENI is in agreement with the findings of Emami et al. Citation[19]. In the analysis of four prospective RTOG studies, the rate of the relapses in the mediastinum, contralateral hilum and supraclavicular regions did not differ significantly in patients with respectively, adequate and inadequate inclusion of these regions in the irradiation field. One may conclude that the similar rate of INF in our study as in the series without ENI supports the routine omission of the ENI. The characteristics of our group, however, differ from the series reporting on the incidence of INF. The latter are mainly based on the dose escalation studies and include less advanced stages Citation[1–7], Citation[17], Citation[18]. The high percentage (84%) of patients had stage III disease. It would be expected that in such a group the risk of INF is higher; moreover it was shown in the study, that the higher nodal stage is related to the higher risk of the INF. Initially higher stage led to the worsening of local and distant results and related to this the probable underestimation of regional failures. Patients with weight loss, well known adverse prognostic factor, had less isolated nodal failures than others. They had also earlier disease dissemination and shorter survival (data not shown), so the competitive risks’ phenomenon did not allow for disclosing INF. No difference in the rate of INF between series with and without ENI may be related to the underestimation in all studies of the real incidence of such events. Patients with early disease dissemination have not often examinations performed for an evaluation of the mediastinum. Under reserve that this factor would have influenced results, the hypothesis that the ENI yielded the low rate of INF is also conceivable. This hypothesis may be supported by the fact that the INF occurred more frequently in the regions receiving doses < 40 Gy than in the LNS receiving higher doses.
To the best of our knowledge the presented study is the first published statistical analysis of relation of prognostic factors with the risk of INF in patients with NSCLC treated with 3D-CRT. Multivariate analysis showed that the presence of bulky mediastinal disease was the only independent predictor of the risk of INF. This variable was taken into account, because in earlier analysis of own data this was the strongest negative prognostic factor Citation[20]. Our finding is supported by the results of Rosenzweig et al. Citation[6], where 10 of 11 patients with INF were N+ including five N3 disease. It is unknown if more extended ENI for more advanced nodal disease would result in improvement of survival, because higher nodal stage is a known adverse prognostic factor. In the presented study 13% of patients with bulky mediastinal disease remained disease free after radiotherapy. Thus, moderate benefit in disease control might be expected from extended ENI in those patients. However, an extended ENI might be associated with an increased toxicity. Nevertheless, we were able to show that when respecting lung dose constraints, the use of the ENI regardless of the extent did not increase usually observed pulmonary toxicity.
Most of INF (10 of 16) occurred in supraclavicular (7) and contralateral hilar regions (3), which were not included in the elective area in both extents of the ENI. Rosenzweig et al. Citation[6] in the series of 171 patients (including 86% of III stage cases) treated with omission of the ENI had 8 of 11 INF in the supraclavicular regions and superior mediastinum. This may be related to the fact that patients with N2 disease are more likely to develop supraclavicular metastases, what was shown by a pattern of failure after surgery of NSCLC Citation[21]. We have shown that the N stage is highly related to the risk of INF. Taking into account such a pattern of INF, we can't exclude the impact of the incidental irradiation on the low rate of regional failures in parts of the mediastinum located close to the involved area. The lower amount of incidental irradiation in the superior mediastinum, supraclavicular regions and contralateral hila than in the vicinity of the bulk of the disease is very likely.
Our study is not reliable for drawing conclusions about a relation of the histology or differentiation degree to the risk of INF, because of the high percentage of patients with no data about exact grade and the type of NSCLC. Other investigators related the histology Citation[9], Citation[22] and differentiation degree Citation[23] to the risk of unforeseen regional metastases.
The higher risk of INF associated with left side of the disease seen in this study was not confirmed by the multivariate analysis, because this was also related to the initially more advanced nodal stage of left-sided tumors. However, we should be aware that left lung has more developed contralateral lymphatic drainage. Nohl-Osler Citation[24] showed that right-sided tumors with mediastinal disease had 5–7% of contralateral metastases, whilst for N2 left-sided tumors, the contralateral involvement reached 22% and 40% for upper and lower lobes, respectively. This should probably impact on larger elective treatment volume for left-sided N2 disease, if PET scanning is not available”.
Lack of the progression of the residual disease following treatment was accepted as a sign of local control for this study as for others evaluating the response of lung cancer to radiotherapy Citation[1]. Patients with complete disappearance of all radiological signs of the disease had significantly lower incidence of INF than patients with partial response to radiotherapy. It cannot be excluded that the INFs seen in this study were a result of a seeding from uncured primary and an improvement of local control as postulated by partisans of the ENI Citation[25] would lead to decreased number of regional failures. On the other hand, an opposite hypothesis is also conceivable that radiosensitive tumors with complete response to treatment had also better response to low radiation doses on elective area and this led to the improvement of regional control for such cases.
The lack of PET and systematic mediastinoscopy for initial staging in this study should be considered as important limitation of our findings. CT of the chest is now considered as a tool not enough efficient for diagnostics of mediastinum in comparison to PET combined with CT Citation[26]. In our series, the median time to occurrence of INF was 7.5 months. For 50% of patients with INF, the distant metastases were found before, simultaneously or up to 3 months following diagnosis of the INF. There were probably patients for whom PET would have shown distant and/or regional metastases before radiotherapy. Thus it is possible that with PET staging the INF rate would be lower in our study.
We should acknowledge that our study because of its retrospective nature cannot answer a question on the value of the ENI for NSCLC. There are however some findings of our study that we postulate to investigate in the prospective trials. Patients with advanced nodal disease should be subject to the prospective study evaluating impact of the ENI on survival. Extent of the ENI should also be investigated for such cases. As precise definition of the extent of the ENI for prospective studies is needed, such studies as ours evaluating doses for particular LNS in sites of nodal failures would be of value.
Conflicts of interest
There were no financial and/or personal relationships with other people and organizations that could inappropriately influence (bias) this work.
References
- Belderbos JSA, Heemsbergen WD, De Jaeger K, Baas P, Lebesque JV. Final results of a phase I/II dose escalation trial in non-small-cell lung cancer using three-dimensional conformal radiotherapy. Int J Radiat Oncol Biol Phys 2006; 66: 126–34
- Bradley J, Graham MV, Winter K, Purdy JA, Komaki R, Roa WH, et al. Toxicity and outcome results of RTOG 9311: A phase I-II dose-escalation study using three-dimensional conformal radiotherapy in patients with inoperable non-small-cell lung carcinoma. Int J Radiat Oncol Biol Phys 2005; 61: 318–28
- Chen M, Hayman JA, Ten Haken RK, Tatro D, Fernando S, Kong FM. Long-term results of high-dose conformal radiotherapy for patients with medically inoperable T1-3N0 non-small-cell lung cancer: Is low incidence of regional failure due to incidental nodal irradiation?. Int J Radiat Oncol Biol Phys 2006; 64: 120–6
- Cheung PCF, Mackillop WJ, Dixon P, Brundage MD, Youssef YM, Zhou S. Involved-field radiotherapy alone for early-stage non-small cell lung cancer. Int J Radiat Oncol Biol Phys 2000; 48: 703–10
- McGarry RC, Papiez L, Williams M, Whitford T, Timmerman RD. Stereotactic body radiation therapy of early-stage non-small cell lung carcinoma: Phase I study. Int J Radiat Oncol Biol Phys 2005; 63: 1010–5
- Rosenzweig KE, Sim SE, Mychalczak B, Braban LE, Schindelheim R, Leibel SA. Elective nodal irradiation in the treatment of non-small cell lung cancer with three-dimensional conformal radiation therapy. Int J Radiat Oncol Biol Phys 2001; 50: 681–5
- Zimmermann FB, Geinitz H, Schill S, Thamm R, Nieder C, Schratzenstaller U, et al. Stereotactic hypofractionated radiotherapy for stage I (T1-2 N0 M0) non-small-cell lung cancer. Acta Oncol 2006; 45: 796–801
- Ginsberg RJ, Rubinstein L, for the Lung Cancer Study Group. A randomised study of lobectomy versus limited resection for patients with T1N0 non-small-cell lung cancer. Ann Thorac Surg 1995;60:615–22.
- Kotoulas CS, Foroulis CN, Kostikas K, Konstantinou M, Kalkandi P, Dimadi M, et al. Involvement of lymphatic metastatic spread in non-small cell lung cancer accordingly to the primary cancer location. Lung Cancer 2004; 44: 183–91
- Rosenzweig KE, Fox JL, Yorke E, Amols H, Jackson A, Rusch V, et al. Results of a phase I dose-escalation study using three-dimensional conformal radiotherapy in the treatment of inoperable non-small cell lung carcinoma. Cancer 2005; 103: 2118–27
- Senan S, Burgers S, Samson MJ, van Klavreren RJ, Oei SS, van Sornsen de Koste J, et al. Can elective nodal irradiation be omitted in stage III non-small-cell lung cancer? Analysis of recurrences in a phase II study of induction chemotherapy and involved-field radiotherapy. Int J Radiat Oncol Biol Phys 2002; 54: 999–1006
- Jeremic B. Incidental irradiation of nodal regions at risk during limited-field radiotherapy (RT) in dose-escalation studies in non-small cell lung cancer (NSCLC): Enough to convert no-elective into elective nodal irradiation (ENI)?. Radiother Oncol 2003; 71: 123–5
- Chapet O, Kong F-M, Quint LE, Chang AC, Ten Haken RK, Eisbruch A, et al. CT-based definition of thoracic lymph node stations: an atlas from the University of Michigan. Int J Radiat Oncol Biol Phys 2005; 63: 170–8
- Mountain CF, Dresler CM. Regional lymph node classification for lung cancer staging. Chest 1997; 111: 1718–23
- Thomas CR, Giroux DJ, Stelzer KJ, Craig JB, Laufman LR, Taylor SA, et al. Concurrent cisplatin, prolonged oral etoposide, and vincristine plus chest and brain irradiation for limited small cell lung cancer: A phase II study of the Southwest Oncology Group (SWOG-9229). Int J Radiat Oncol Biol Phys 1998; 40: 1039–47
- Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organisation for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 1995; 31: 1341–6
- Sibley GS, Jamieson TA, Marks LB, Anscher MS, Prosnitz LR. Radiotherapy alone for medically inoperable stage I non-small-cell lung cancer: The Duke experience. Int J Radiat Oncol Biol 1998; 40: 149–54
- Slotman BJ, Antonisse IE, Njo KH. Limited field irradiation in early stage (T1-2N0) non-small cell lung cancer. Radiother Oncol 1996; 41: 41–4
- Emami B, Mirkovic N, Scott C, Craig JB, Laufman LR, Taylor SA, et al. The impact of regional nodal radiotherapy (dose/volume) on regional progression and survival in unresectable non-small cell lung cancer: An analysis of RTOG data. Lung Cancer 2003; 41: 207–14
- Kepka L, Fijuth J, Zawadzka A, Blatkiewicz D, Zajda K, Wierzchowski M. Accelerated Radiotherapy (aRT) for locally advanced NSCLC: Significance of bulky disease?. Radiother Oncol 2002; 64: S254
- Kelsey CR, Light KL, Marks LB. Patterns of failure after resection of non-small-cell Lung Cancer: Implications for postoperative radiation therapy volume. Int J Radiat Oncol Biol Phys 2006; 65: 1097–105
- Giraud P, De Rycke Y, Lavole A, Milleron B, Cosset J-M, Rosenzweig KE. Probability of mediastinal involvement in non-small-cell lung cancer: A statistical definition of the clinical target volume for 3-dimensional conformal radiotherapy?. Int J Radiat Oncol Biol Phys 2006; 64: 127–35
- Sawyer TE, Bonner JA, Gould PM, Garces YI, Foote RL, Lange CM, et al. Predictors of subclinical nodal involvement in clinical stages I and II non-small cell lung cancer. Implications in the inoperable and three dimensional dose-escalation settings. Int J Radiat Oncol Biol Phys 1999; 43: 965–70
- Nohl-Oser HC. An investigation of the anatomy of the lymphatic drainage of the lungs as shown by the lymphatic spread of bronchial carcinoma. Ann R Coll Surg Engl 1972; 51: 157–76
- Williams TE, Thomas CR, Turrisi AT. Counterpoint: Better radiation treatment of NSCLC using new techniques without elective nodal irradiation. Semin Radiat Oncol 2000; 10: 315–23
- Vansteenkiste JF, Stroobants SG, De Leyn PR, Dupont PJ, Bogaert J, Maes A, et al. Lymph-node staging in non-small cell lung cancer with FDG-PET scan: A prospective study on 690 lymph node stations from 68 patients. J Clin Oncol 1998; 16: 2142–9