Introduction
Adult T-cell leukemia/lymphoma (ATLL) is a highly aggressive peripheral T-cell lymphoid neoplasm associated with the human T-cell lymphotropic virus type-1 (HTLV-1) infection. Cutaneous manifestations of ATLL are diverse with clinical and histopathologic features mimicking various skin conditions [Citation1]. As a result, one-third of patients with cutaneous manifestations of ATLL are initially misdiagnosed, which has led to its classification as an emerging public health problem in northeastern urban communities with large Caribbean migrant populations such as ours [Citation2].
The most common clinical manifestations of ATLL include nodulotumoral-type lesions, plaques, and patches and clinicians are most habituated to identifying such lesions [Citation3]. However, familiarization with the published literature identifies multiple case reports of atypical cutaneous manifestations of ATLL that inevitably perplexed providers on initial presentation [Citation4–6]. Often, these patients were empirically treated for the disease being clinically mimicked and ultimately required histopathologic analysis for accurate diagnosis after initial attempts at treatment were unsuccessful. We present a case of ATLL with atypical cutaneous manifestations that due to appropriate, early dermatologic diagnosis reconnected the patient with his oncology team to begin salvage chemotherapy and address the inevitable, morbid clinical deterioration that soon precipitated due to advancement of this aggressive disease.
Case report
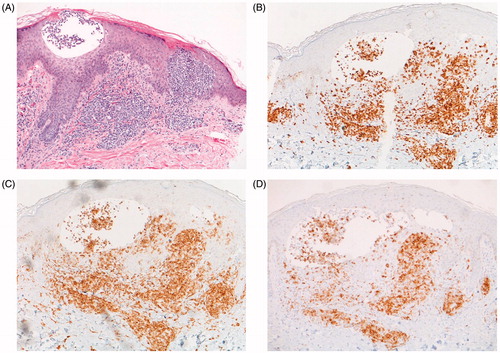
A 61-year-old man of Caribbean descent with a 14-month history of ATLL diagnosed after workup for fatigue and weight loss, now 5 months status post stem cell transplant, presented with a pruritic rash on his face, trunk and proximal extremities for the past 15 days. Examination was notable for pink oedematous pseudovesiculated plaques closely resembling Sweet Syndrome (), although the patient was afebrile and otherwise asymptomatic. Of note, the patient also had an erythematous eruption on the neck and trunk 2 months prior that resolved with corticosteroids. Due to lack of engraftment, the patient’s immunosuppression including all corticosteroids was discontinued 1 week before the onset of the current rash. The possibility of relapsed malignancy-associated Sweet Syndrome, following steroid-induced clinical resolution of the previous rash, was considered [Citation3,Citation7]. Despite this clinical picture, a punch biopsy revealed HTLV-1+ epidermotropic ATLL and immunophenotyping remained consistent with the diagnosis: CD3+, CD4+, CD25+, CD8- (). The biopsy also displays intra-epidermal microvesicles containing atypical lymphoid cells (), which explains the clinical appearance of Sweet Syndrome. Improvement of the rash occurred following salvage chemotherapy with ifosfamide, carboplatin and etoposide.
Discussion
While the cutaneous manifestations of ATLL are manifold, there are no previously reported cases of ATLL resembling Sweet Syndrome to our knowledge [Citation3]. Patients who develop ATLL-associated skin manifestations after systemic diagnosis most commonly have nodulotumoral-type lesions followed by plaques and patches; however, unlike our patient, classical plaque-type cutaneous ATLL is described as disseminated infiltrating erythema clinically comparable to Mycosis Fungoides [Citation1]. The literature does detail three rare case reports of vesiculobullous eruptions more similar to our patient, however, distribution and morphology of lesions mimicked alternate clinical disorders including dyshidrotic eczema and bullous Mycosis Fungoides [Citation4–6].
Ultimately, management of cutaneous manifestations of ATLL is based on the treatment of the underlying systemic disease, which is a primary reason early identification and diagnosis are essential, especially since the presence of skin lesions is an independent prognostic factor [Citation8]. We present this case to broaden the collection of features that warrant diagnostic consideration of ATLL, which will allow for earlier diagnosis and improved prognosis.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Miyashiro D, Sanches JA. Cutaneous manifestations of adult T-cell leukemia/lymphoma. Semin Diagn Pathol. 2019.
- Marchetti MA, Pulitzer MP, Myskowski PL, et al. Cutaneous manifestations of human T-cell lymphotrophic virus type-1-associated adult T-cell leukemia/lymphoma: a single-center, retrospective study. J Am Acad Dermatol. 2015;72:293–301.
- Cohen PR, Talpaz M, Kurzrock R, et al. Malignancy-associated Sweet’s syndrome: review of the world literature. J Clin Oncol. 1988;6:1887–1897.
- Mouzakis J. Vesiculobullous variant of adult T-cell leukemia/lymphoma in a Caribbean Émigré. J Drugs Dermatol. 2011;10:1469–1471.
- Chan HL, Su IJ, Kuo TT, et al. Cutaneous manifestations of adult T cell leukemia/lymphoma. J Am Acad Dermatol. 1985;13:213–216.
- Bittencourt AL, Mota K, Oliveira RF, et al. A dyshidrosis-like variant of adult T-cell leukemia/lymphoma with clinicopathological aspects of mycosis fungoides. A case report. Am J Dermatopathol. 2009;31:834–837.
- Cohen PR. Sweet’s syndrome–a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis. 2007;2:34.
- Sawada Y, Hino R, Hama K, et al. Type of skin eruption is an independent prognostic indicator for adult T-cell leukemia/lymphoma. Blood. 2011;117:3961–3967.