Abstract
Background and purpose
The aim of this cross-sectional study was to investigate long-term health-related quality of life (HRQoL) in men with prostate cancer treated 2002–2008 with external beam radiotherapy (EBRT) combined with high dose-rate brachytherapy (HDRBT), Cohort A, and to compare these data with age-adjusted normative data. In addition, differences in HRQoL following adjustments of the brachytherapy technique in 2001 were investigated by comparing Cohort A with men treated at the same clinic from 1998-2000, Cohort B.
Methods and material
Cohort A: 1495 men treated with EBRT 2 Gy to 50 Gy and 2 fractions of 10 Gy HDRBT at a single centre, 2002–2008, still alive at five years. As part of routine follow-up, the patients responded to the EORTC QLQ-C30 and PR-25 questionnaires. Cohort B: HRQoL data was retrieved from an earlier study from the original article.
Results
In Cohort A, 1046 (70%) men completed the questionnaires at five years, median age 66 years. In general, HRQoL mean scores were high and similar to Swedish age-matched normative data. Concerning disease-specific HRQoL, low levels of bowel and urinary problems were reported, in contrast to a substantial effect on sexual functioning. ‘No’ or ‘A little’ problems with faecal incontinence and urinary incontinence were reported by 98% and 93% of patients, respectively. The corresponding figure for sexual functioning was 39%. A difference in the frequency of nocturia in favour of Cohort A was the only statistically significant difference between Cohort A and B found in general and disease-specific HRQOL (p = 0.03), despite modifications in the brachytherapy procedure introduced in 2001.
Conclusion
Long-term general HRQoL was rated high and comparable to an aged-matched reference population five years after treatment with combined radiotherapy. Disease-specific HRQoL was still affected, foremost in the sexual domain.
Background
Today, the main treatment options in routine use for prostate cancer (PC) are open or robotic radical prostatectomy (RP), external beam radiotherapy (EBRT), brachytherapy (BT) or combinations of these treatments [Citation1–4]. These modalities have a high rate of cure, but also potential to cause life-long disabilities concerning urinary, bowel and sexual functioning. Hence, it is important also to consider toxicity and health-related quality of life (HRQoL) when counselling the individual PC patient in the choice of treatment [Citation5]. In a recent review, long-term HRQoL between different curative treatment options for PC were summarised, showing high general HRQoL irrespective of treatment [Citation6]. In general, men had more sexual problems and incontinence after RP than after EBRT or active surveillance. On the other hand, men treated with EBRT had more bowel symptoms, but also suffered from deterioration of sexual function. In comparison with RP and EBRT, mono low-dose rate BT (LDRBT) seemed to retain better sexual functioning, but more irritative urinary problems. Furthermore, a randomised study found that LDRBT combined with EBRT and ADT resulted in more urinary problems than dose-escalated EBRT and ADT [Citation7]. Data on long-term HRQoL in men treated with combined high-dose rate brachytherapy (HDRBT) is, however, scarce. The studies are often small and mix men treated with HDRBT and LDRBT. Thus, there is a need for further studies elucidating the long-term effects on HRQoL after combined HDRBT.
HDRBT combined with EBRT was introduced at Karolinska University Hospital 1998 and has, since then, been an established curative treatment option for localised PC. The principles of treatment, five- and 10-year outcome and toxicity data for a subset of men have been reported previously [Citation8,Citation9]. The 10-year follow-up showed excellent local control, estimated to >98%, and a prostate cancer-specific mortality of 5%. With the intention to reduce urinary toxicity, a modern HDR-brachytherapy equipment was introduced in 2001, allowing for a better dose-distribution and control of the dose to the urethra. The effect on toxicity of the change in procedure was evaluated by use of the RTOG symptom scale for men treated before and two years after the introduction of new technique. The recordings showed a reduction in RTOG grade 3 or higher urinary toxicity to 10–15% in the late cohort, compared to 25–40% in the early cohort [Citation10]. In 2005, five-year HRQoL in men treated 1998–2000 was investigated using the EORTC QLQ-C30 and the disease-specific questionnaire EORTC QLQ-PR25 [Citation11]. The study showed similar general HRQoL as an aged matched male reference population. However, moderate urinary and significant sexual problems were still present after five years.
The first aim of the present study was to explore general and disease specific effects on HRQoL in a large cohort of men treated with HDRBT and EBRT in comparison with aged matched Swedish reference data, to gain further information on the long-term effects on HRQoL of this treatment modality. The second aim was to investigate if changes in the treatment procedure introduced in 2001, which reduced genitourinary toxicity assed by the treating physician, also translated into improved long-term HRQoL at five years in the cohort of men treated with the new technique.
Method and materials
Cohort A
During 1998 to 2010, 2387 men diagnosed with localised and locally advanced prostate cancer were treated at the Karolinska University Hospital with EBRT combined with two fractions of HDRBT. Men treated between January 2002 until December 2008 were included in the present cross-sectional study, n = 1639. In this group, 108 (7%) men died and 36 (2%) had a recurrence of PC before five years, leaving 1495 men for follow-up in the present study. The study was approved by ethical authorities in the Stockholm Region (04/1025/3, 2006/620-31/1) and the STROBE cross-sectional reporting guideline was used [Citation12].
Clinical staging
All included men had histologically confirmed adenocarcinoma of the prostate, classified according to the Gleason grading system [Citation13]. Further, staging was performed according to the TNM classification 5th-7th edition [Citation14]. In patients with Gleason ≥ 4 + 3, PSA ≥ 20 µg/L and from 2007 cT3a tumour, a bone scan and surgical lymph node dissection were performed. Only men with ≤ T3a N0, M0 disease were offered HDBRT.
Treatment
All men in Cohort A were treated with a combination of HDRBT 10 Gy in 2 fractions, combined with EBRT 2 Gy in 25 fractions, using a conventional 3-dimensional technique. In addition, 98% received neoadjuvant and concomitant total androgen blockade for six to nine months. Principles of the combined HDBRT + EBRT treatment technique have been described in detail previously [Citation9]. The EBRT planning target volume PTV comprised the prostate gland and the vesicles, covered by the 95% iso-dose curve. The only constraint to organs at risk was a limit not to exceed 50 Gy in the posterior rectal wall. The HDRBT PTV comprised the prostate gland and the base of the seminal vesicles with a 3 mm margin, except in the cranial and caudal direction. The V100% to CTV was minimum 90% of the prescribed dose, and the V200% was set to <10% of PTV dose. The dose constraints to the urethra and rectum were Dmax <11 Gy and Dmax <6 Gy, respectively.
Follow-up
The patients were followed up three months after radiotherapy, and thereafter, twice a year for the next two years and then annually up to ten years. The follow-up included blood samples, and evaluation of side-effects. From March 2005, the EORTC QLQ-C30 and QLQ-PR25 questionnaires were included in the routine follow-up. Patients signalling worse outcomes at any time were examined based on the medical needs required by the symptoms or disabilities reported.
Data collection
The questionnaires collected for clinical follow-up at five years, ± 1 year were used in this study. If the patient had completed more than one form during this time span, the one closest to five years was used. The questionnaires were sent with the summon. The patients were asked to respond before their visit to the clinic. The questionnaires was handed to a nurse at the clinic before the clinical examination. No reminders were sent. Basic patient and tumour characteristics, data on biochemical failure and death were collected from patients’ medical records from 2005 until October 2019 and stored, together with the HRQoL forms, using the Medlog system software (Information Analysis System, NV 89402, USA).
Cohort B
Cohort B consisted of men treated with combined HDRBT from 1998 to 2000 at the Karolinska University Hospital. Brachytherapy was performed with the initial procedure used from 1998 to 2001, but in other aspects the treatment was identical to Cohort A. Men, still alive five years after treatment, were offered to take part in a study to evaluate long-term HRQoL [Citation11]. A total of 196 men were still alive and of those, 182 (93%) responded to the questionnaires. From this group, in total 24 men were excluded because of development of secondary cancer diagnoses (n = 4) and recurrence of disease (n = 20). Hence, 158 men remained to be analysed. Data from the original publication (mean scores, confidence intervals and frequencies) were used in the present study to evaluate differences in HRQoL in men treated before (Cohort B) and after (Cohort A) the modifications of treatment technique in 2001.
Reference population
Reference data for the EORTC QLQ-c30 was retrieved from a publication including a random sample of 3000 individuals from the Swedish population, aged 18–79 years [Citation15]. In the present study, age-matched reference data from the male population was used.
Health related quality of life (HRQoL) instruments
The EORTC Quality of Life Questionnaire C30 (EORTC QLQ-C30) is a core questionnaire designed to measure HRQoL in cancer patients regardless of type of malignancy [Citation16]. It consists of 30 items, forming five functional scales (physical, role, emotional, social, and cognitive), three symptom scales (fatigue, pain, nausea and vomiting), a global health status/QoL scale, and six single items (dyspnoea, loss of appetite, insomnia, constipation, diarrhoea, and financial impact of disease).
To address PC-specific issues, the disease-specific module EORTC QLQ-PR25 was used. It consists of 25 items, that cluster into five multi-item scales; sexual activity and function, urinary, bowel and, hormonal treatment related symptoms, and one single item concerning incontinence aid. This questionnaire was developed during the study period and validated in 2008 in a psychometric field study [Citation17]. The study confirmed the suggested multi-item scale structure. However, the reliability for the bowel and hormonal treatment related scales was low, probably related to low score variation. The investigators considered the scales relevant despite this, but advocated that both the scale score means and the frequency of intensity per item to be reported.
Statistical methods
Questionnaire data were analysed according to the EORTC scoring manual [Citation18], but missing data were not imputed. Raw scores were transformed into a linear scale ranging from 0 to 100. Higher scores indicate better functioning for the functional subscales and the global quality of life scale, and more symptoms for the symptom scales. Mean scores and 95% confidence intervals were calculated on the summed scores. Expected mean scores for each of the EORTC QLQ-C30 subscales was calculated by indirect standardisation using the age-distribution in the study cohort, and with age-specific mean reference scores from the Swedish population [Citation15]. Differences between Cohort A and B concerning the frequency of disease specific sub-items in QLQ-PR 25 was assessed by Chi-square tests.
Results
In Cohort A, 1046 (70%) completed the EORTC QLQ-C30 and QLQ-PR25 questionnaires. The mean time between BT and HRQoL follow-up was 5.3 years (range 4.0–5.9 years). Patient characteristics in Cohort A and B are shown in . In Cohort A, 13% had Gleason score ≥8 and 36% had T3 status. In Cohort B 13% had WHO grade 3 cancer and 28% had documented T3 status. The median PSA at diagnosis was 10.2 µg/l (range 1-110) and 13.8 µg/l (2–116) in Cohort A and B, respectively.
Table 1. Patient characteristics for Cohort A and Cohort B.
Health related quality of life results, cohort A
The HRQoL results from the EORTC QLQ-C30 for Cohort A are presented in . Overall, the mean scores were high for the functioning scales and low for symptom scales and single items. In comparison with the age-matched Swedish reference population there were small statistically significant differences between the two cohorts concerning physical- and role-functioning in favour of the HDBRT-EBRT treated patients, and for global health status and social-function in favour of the reference population (). Concerning symptom scales and single items, the HDRBT-EBRT treated patients reported lower levels of pain, dyspnoea and financial difficulties than the reference group. However, Cohort A reported more problems concerning constipation, diarrhoea and insomnia.
Figure 1. a and b, EORTC QLQ-C30, Functional, symptom scales and single items, mean score. A comparison between Cohort A and an age-matched Swedish reference population (ref. population). Global health (GH), Physical functioning (PF), Role functioning (RF), Emotional functioning (EF), Cognitive functioning (CF), Social functioning (SF), Fatigue (FA), Nausea/vomiting (NV), Pain (PA), Dyspnoea (DY), Sleeping disturbances (SL), Loss of appetite (AP), Constipation (CO), Diarrhoea (DI), Financial difficulties (FI).
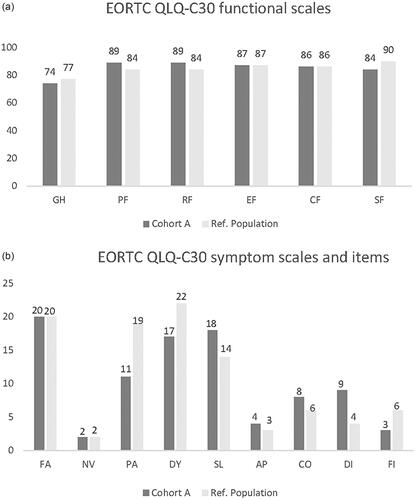
Table 2. EORTC QLQ-C30 and QLQ-PR25 HRQoL results cohort A and B.
The results from the disease-specific questionnaire EORTC QLQ-PR25 for cohort A are shown in and . For the urinary-, bowel- and hormone-related scales, the mean scores indicated low levels of problems. However, patients reported a higher level of urinary than bowel problems. Sexual function and activity appeared to be more seriously affected. In the group of men reporting sexual function (men sexually active during the past month), 10% and 29% reported ‘No’ or ‘A little’ erectile problems, respectively, whereas 34% reported ‘Very much’ problems.
Table 3. EORTC QLQ-PR25 selected items at five years, comparing Cohort A and B.
Comparison of HRQoL in men treated 1998–2000 and 2002–2008
The comparison between Cohort A and Cohort B showed similar results regarding EORTC QLQ-C30 and QLQ-PR25 five years after radiotherapy, with basically no statistically significant differences between the two cohorts ( and ). The only statistically significant difference was found for the frequency of nocturia, in favour of Cohort A. In total, 22% of the men in Cohort A reported severe nocturia (“Quite a bit” and “Very much”) compared to 31% in Cohort B (p = 0.03). “No” or “A little” problems were reported by the majority of men, 99% and 97-98% respectively, concerning rectal bleeding and faecal incontinence. About a third of the patients in Cohort A and B reported a modest to high sexual interest. In the group of men reporting sexual activity, similar proportions reported “No” or “A little” erectile problems in both cohorts.
Discussion
During 1998 to 2010, 2387 men with localised and locally advanced prostate cancer were treated with curative intended combined EBRT and HDRBT at our institution. Ten-year outcomes showed an excellent local control and OS in all risk groups [Citation9]. The present study aimed to analyse long-term HRQoL five years after treatment and is, to our knowledge, the largest cross-sectional single institution study in this field. In general, patients reported high levels of HRQoL, measured by the EORTC QLQ-C30 questionnaire, comparable to an age-and gender-matched Swedish reference population. The disease-specific HRQoL results showed low levels of bowel and urinary problems, but substantial problems in the sexual domain. The comparison of HRQoL in Cohort B treated during the first two years after the introduction of HDRBT (1998–2000) with Cohort A treated 2002–2008 showed similar HRQoL in both general and disease-specific domains, except for the frequency of nocturia, in favour of the latter group. The difference was, however, small and of dubious clinical significance. The major changes in the treatment procedure introduced during 2001, which limited the RTOG grade ≥3 urinary side effects by 50%, did not appear to translate into a corresponding difference in urinary or general HRQoL between the treatment groups.
Only a few studies report long-term HRQoL (≥ five years) after HDRBT, including one or two brachy sessions combined with EBRT. The number of patients in these studies range from N = 55 to N = 215 and are heterogeneous including patients from all risk groups, with or without the addition of ADT [Citation11,Citation19–24]. One of these studies reported only general [Citation21] and two only disease-specific HRQoL [Citation23,Citation24]. The studies used various HRQoL questionnaires, which makes comparisons and interpretation of results even more difficult. However, the studies reported high HRQoL in the general domains, comparable to age-matched reference populations or matched controls, which support the findings in the present study. Moreover, most of the studies, including the present study, observed an improvement in role and physical functioning [Citation11,Citation19,Citation21], which may be due to adaptation or ‘response shift’, a phenomenon well known in HRQoL research described by Sprangers and Schwartz [Citation25]. They suggested that a major change in health status leads to a change in the way an individual values different quality of life issues. A lower level in social functioning was noted amongst patients compared to the reference population in our study, consistent with the findings in Cohort B. In contrast, two of the studies utilising the EORTC questionnaires did not find any difference between patients and the reference population in social functioning, despite reporting bowel and urinary problems at similar levels as in our study [Citation19,Citation20]. Concerning disease-specific HRQoL, men treated with HDRBT and EBRT typically show a specific pattern with low levels of bowel problems, a slightly higher proportion of urinary bother and more substantial problems in the sexual domain concerning both activity and erectile function, similar to our findings in the present study [Citation5,Citation11,Citation20,Citation22–24].
In comparison with randomised studies investigating modern dose-escalated and hypo-fractionated EBRT regimes, our consecutively treated patient cohort had similar long-term results concerning general HRQoL [Citation26–28]. However, in the Ascende-RT study, comparing LDRBT combined with EBRT and dose-escalated EBRT, the LDRBT group reported a significant deterioration of physical function after five years [Citation7]. Furthermore, these studies reported low levels of bowel problems in general at five to six years, especially concerning serious problems with faecal leakage and rectal bleeding, similar as in our study. Modest levels of urinary problems were still present at five years, above all urgency and nocturia in the present study. In general, the above-mentioned studies reported, compared to their baseline levels, low levels of residual urinary problems after five years. However, in the Ascende-RT study the cumulative incidence of Grade 3 toxicity in the combination arm was three times higher than the incidence in the dose-escalated EBRT-arm, indicating that the higher biological dose to the prostate with the BT combination might be of importance for the development of these treatment related side-effects [Citation7]. Shahid et al, found a relationship between urinary function and dose to the urethra (Dmax10%) [Citation24]. Thus, ours and previous studies indicate that the level of urinary problems are relatively rare five years after dose-escalated RT, but with a modest level of urgency still remaining in the HDRBT group.
In our study, a large proportion of men reported loss of sexual function and interest compared to problems in other domains. Similar results have been shown in a number of studies covering different treatment regimens of PC, including surgery [Citation5,Citation11,Citation20,Citation22–24,Citation26–29]. Longitudinal data show lower HRQoL in this domain at baseline compared to other areas of interest, which might partially explain this finding, as age and pre-treatment function are recognised predictors of sexual function [Citation29,Citation30]. Another aspect of concern is the use of neoadjuvant and adjuvant hormonal treatment that is known to impair sexual function and could thereby contribute to the low functional levels in the sexual domain [Citation31–33].
In the comparison of men treated before and after the introduction of a modern dose-planning system and high-resolution ultrasound technique, only a small improvement in nocturia was found despite the reduction of early toxicity found in our preliminary evaluation described above. In the study by Wahlgren et al [Citation34], longitudinal data from the early cohort showed a marked deterioration in the urinary scale after treatment that gradually improved during the first years. A similar pattern was also found in the hypofractionation studies discussed above [Citation26–28]. This suggests that the improved technique foremost reduced the acute toxicity and, that the residual symptoms still present are likely to be a sign of late radiation induced urinary problems.
The interpretation of HRQoL scores and differences in scores within and between different populations could be of concern. In a large patient cohort, such as ours, even small differences in scores could prove to be statistically significant, but might be of little clinical relevance. Osoba et al investigated the clinical relevance of changes in HRQoL-scores [Citation35]. They defined the term SSD, subjectively significant difference, based entirely on the patients self-appreciated perception of what size of the change is a meaningful change and found that a change in 10 points in the EORTC QLQ-C30 questionnaire mean score would be clinically relevant. Applying the same definition as Osoba, we did not observe any clinically significant differences either between Cohort A and B or the age-matched reference population concerning general HRQoL.
The main strength in our study is the large consecutive patient population, treated in a single institution and which have been followed-up uniformly during 10 years including HRQoL questionnaires at five years. The EORTC QLQ C30 and EORTC QLQ-PR25 questionnaires were used, which both are validated and one is disease specific. A Swedish reference population was available for comparison of the results for general HRQoL. The response rate was acceptable, 70% at five years. The main limitations are the cross-sectional design, the lack of baseline HRQoL data, especially concerning EORTC QLQ-PR25, and the risk of passive coercion bias as our questionnaires were administered through the treating institution.
Conclusion
Overall, long-term general HRQoL in men with localised prostate cancer was rated high and comparable to an aged-matched reference population, five years after treatment with combined HDRBT and EBRT. Disease-specific HRQoL was still affected at five years, foremost in the sexual domain. The changes in treatment procedure introduced in 2001 reduced genitourinary toxicity as assessed by the physicians with 50% but did not translate into improved long-term self-reported HRQoL.
Supplemental Material
Download MS Word (38 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author, [MHE], upon reasonable request.
References
- Hoskin PJ, Rojas AM, Bownes PJ, et al. Randomised trial of external beam radiotherapy alone or combined with high-dose-rate brachytherapy boost for localised prostate cancer. Radiother Oncol. 2012;103(2):217–222.
- Zelefsky MJ, Yamada Y, Fuks Z, et al. Long-term results of conformal radiotherapy for prostate cancer: Impact of dose escalation on biochemical tumor control and distant metastases-free survival outcome. Int j Radiat Oncol Biol Phys. 2008;15(71):1028–1033.
- Dearnaley DP, Jovic G, Syndikus I, et al. Escalated-dose versus control-dose conformal radiotherapy for prostate cancer: Long-term results from the MRC RT01 randomised controlled trial. Lancet Oncol. 2014;15(4):464–473.
- Mahmood U, Levy LB, Nguyen PL, et al. Current clinical presentation and treatment of localized prostate cancer in the United States. J Urol. 2014;192(6):1650–1656.
- Ávila M, Patel L, López S, et al. Patient-reported outcomes after treatment for clinically localized prostate cancer: a systematic review and Meta-analysis. Cancer Treat Rev. 2018;66:23–44.
- Taylor JM, Chen VE, Miller RC, et al. The impact of prostate cancer treatment on quality of life: a narrative review with a focus on randomized data. Res Rep Urol. 2020;12(12):533–546.
- Rodda S, Tyldesley S, Morris WJ, et al. ASCENDE-RT: an analysis of Treatment-Related morbidity for a randomized trial comparing a Low-Dose-Rate brachytherapy boost with a Dose-Escalated external beam boost for high- and Intermediate-Risk prostate cancer. Int J Radiat Oncol Biol Phys. 2017;98(2):286–295.
- Kälkner KM, Wahlgren T, Ryberg M, et al. Clinical outcome in patients with prostate cancer treated with external beam radiotherapy and high dose-rate iridium 192 brachytherapy boost: a 6-year follow-up. Acta Oncol. 2007;46(7):909–917.
- Hjälm-Eriksson M, Nilsson S, Brandberg Y, et al. High rate of local control and cure at 10 years after treatment of prostate cancer with external beam radiotherapy and high-dose-rate brachytherapy: a single Centre experience. Acta Oncol. 2021;60(10):1301–1307.
- Cohn-Cedermark G, Hjälm-Eriksson M, Castellanos, et al. The frequency of side effects among patients with localized prostate cancer treated with combined external radiotherapy and HDR 192-Iridium brachytherapy boost decreases with number of treated patients; An effect of the learning curve. Poster session, European Society for Therapeutic Radiology and Oncology ESTRO 27, Annual conference, 2008 Sept 14-18, Gothenburg, Sweden.
- Wahlgren T, Nilsson S, Lennernas B, et al. Promising long-term health-related quality of life after high-dose-rate brachytherapy boost for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2007;69(3):662–670.
- von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Epidemiology. 2007;18(6):800–804.
- Delahunt B, Egevad L, Samaratunga H, et al. Review. Gleason and fuhrman no longer make the grade. Histopathology. 2016;68(4):475–481.
- Sobin LH, Wittekind CH, editors. International union against cancer. TNM classification of malignant tumours. 5th ed. New York (NY), John Wiley & Sons, 1997.
- Michelson H, Bolund C, Nilsson B, et al. Health-related quality of life measured by the EORTC QLQ-C30—reference values from a large sample of swedish population. Acta Oncol. 2000;39(4):477–484.
- Aaronson NK, Ahmedzai S, Bergman B, et al. The european organisation for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–376.
- Van Andel G, Bottomley A, Fossa SD, et al. An international field study of the EORTC QLQ-PR25: a questionnaire for assessing the health-related quality of life of patients with prostate cancer. Eur J Can. 2008;44(16):2418–2424.
- Fayers PM, Aaronson NK, Bjordal K, et al. The EORTC QLQ-C30 Scoring Manual 3rd Edition. Brussel (BE) European Organisation for Research and Treatment of Cancer, 2001.
- Galalae RM, Loch T, Riemer B, et al. Health-related quality of life measurement in long-term survivors and outcome following radical radiotherapy for localized prostate cancer. Strahlenther Onkol. 2004;180(9):582–589.
- Joly F, Brune D, Couette JE, et al. Health-related quality of life and sequelae in patients treated with brachytherapy and external beam irradiation for localized prostate cancer. Ann Oncol. 1998;9(7):751–757.
- Huang-Tiel HJ, Otto I, Golka K, et al. Health-related quality of life and rates of toxicity after high-dose-rate brachytherapy in combination with external beam radiation therapy for high-risk prostate cancer. Investig Clin Urol. 2020;61(3):250–259.
- Hoskin PJ, Rojas JA, Ostler MJ, et al. Quality of life after radical radiotherapy for prostate cancer: Longitudinal study from a randomised trial of external beam radiotherapy alone or in combination with high dose rate brachytherapy. Clin Oncol (R Coll Radiol). 2013;25(5):321–327.
- Morgan TM, Press RH, Cutrell PK, et al. Brachytherapy for localized prostate cancer in the modern era: a comparison of patient-reported quality of life outcomes among different techniques. J Contemp Brachytherapy. 2018;10(6):495–502.
- Shahid N, Loblaw A, Chung HT, et al. Long-term toxicity and health-related quality of life after single-fraction high dose rate brachytherapy boost and hypofractionated external beam radiotherapy for intermediate-risk prostate cancer. J Clin. Oncol. 2017;29(7):412–420.
- Sprangers MAG, Schwartz CE. Integrating response shift into health-related quality of life research: a theoretical model. Soc Sci Med. 1999;48(11):1507–1515.
- Fransson P, Nilsson P, Gunnlaugsson A, et al. Ultra-hypofractionated versus conventionally fractionated radiotherapy for prostate cancer (HYPO-RT-PC): patient-reported quality-of-life outcomes of a randomised, controlled, non-inferiority, phase 3 trial. Lancet Oncol. 2021;22(2):235–245.
- Staffurth JN, Haviland JS, Wilkins A, CHHiP Trial Management Group, et al. Impact of hypofractionated radiotherapy on patient reported outcomes in prostate cancer: Results up to 5 year in the CHHiP trial (CRUK/06/016). J. Eur Urol Oncol. 2021;4(6):980–992.
- Wortel RC, Oomen-de Hoop E, Heemsbergen WD, et al. Moderate hypofractionation in intermediate- and High-Risk, localized prostate cancer: Health-Related quality of life from the randomized, phase 3 HYPRO trial. Int J Radiat Oncol Biol Phys. 2019;103(4):823–833.
- Huang GJ, Sadetsky N, Penson DF. Health related quality of life for men treated for localized prostate cancer with long-term follow up. J Urol. 2010;183(6):2206–2212.
- Alemozaffar M, Regan MM, Cooperberg MR, et al. Prediction of erectile function following treatment for prostate cancer. JAMA. 2011;306(11):1205–1214.
- Roeloffzen EM, Lips IM, Van Gellekom MP, et al. Health-related quality of life up to six years after (125) I brachytherapy for early-stage prostate cancer. Int J Radiat Oncol Biol Phys. 2010;76(4):1054–1060.
- Hollenbeck BK, Wei JT, Sanda MG, et al. Neoadjuvant hormonal therapy impairs sexual outcome among younger men who undergo external beam radiotherapy for localized prostate cancer. J. Urology. 2004;63(5):946–950.
- Fransson P, Widmark A. Does one have a sexual life 15 years after external beam radiotherapy for prostate-cancer? Prospective patient-reported outcome of sexual function, a comparison with age-matched controls. Urol Oncol. 2011;29(2):137–144.
- Wahlgren T, Nilsson S, Ryberg M, et al. Combined curative radiotherapy including HDR brachytherapy and androgen deprivation in localized prostate cancer: a prospective assessment of acute and late treatment toxicity. Acta Oncol. 2005;44(6):633–643.
- Osoba D, Rodrigues G, Myles J, et al. Interpreting the significance of changes in Health-Related quality-of-Life scores. J Clin Oncol. 1998;16(1):139–144.
