Abstract
Background
Prior studies of suicide risk among prostate cancer patients are conflicting. We compared the risk of suicide in prostate cancer patients to cancer-free men including adjustment for clinical stage, socioeconomic position, somatic comorbidity, and previous depression.
Materials and methods
A cohort of 37,527 men diagnosed with prostate cancer in Denmark during 1998–2011 was identified in the Danish Prostate Cancer Registry (DaPCaR) and compared with 357,384 cancer-free men matched by age at the time of diagnosis. The primary outcome was death from suicide. Data were analyzed using cumulative incidence functions and multivariable Cox regression models.
Results
Among prostate cancer patients, 3813 had a previous depression, defined as filed antidepressant prescription within three years before diagnosis. In the study period, 108 prostate cancer patients were registered with suicide as the cause of death, hereof 26 with previous depression. There was no difference in the cumulative incidence of suicide between prostate cancer patients and cancer-free men. There was no effect modification of previous depression on the risk of suicide (p = .12). The hazard ratio (HR) for suicide varied with time since diagnosis. A sensitivity analysis showed that the risk of suicide was highest within the first year of diagnosis where prostate cancer patients had a 1.70-fold increased hazard compared with cancer-free men (95% CI, 1.11–2.59). Men with prostate cancer and previous depression had a three-fold increased hazard for suicide compared with prostate cancer patients without a history of depression (HR 2.84, 95% CI, 1.82–4.45).
Conclusion
The absolute risk of suicide is low following a prostate cancer diagnosis. Time since diagnosis and a history of depression was associated with the highest risk of suicide. Healthcare professionals should be aware of an increased risk of suicide among men with previous depression, especially in the immediate aftermath of the diagnosis.
Background
In the past two decades, the number of men diagnosed with prostate cancer in the Western World has exploded due to increased awareness and PSA testing. Today, more than 90% of patients will survive 5 years or more after diagnosis, making management of survivorship issues, such as psychological morbidity, important in this large patient population [Citation1]. We previously found that the first use of anti-depressants remains significantly increased for up to 18 years after a prostate cancer diagnosis compared with age-matched cancer-free men, thereby illustrating the long-lasting severity of the psychological burden [Citation2].
Cancer patients in general are at an increased risk of suicide compared with cancer-free populations [Citation3,Citation4]. The increased risk of suicide is suggested to be associated with factors such as hopelessness, impaired physical functioning, pain, and disease prognosis [Citation5]. In patients with prostate cancer, proposed risk factors for suicide may include older age (>75 years at diagnosis), recent diagnosis (<12 months since diagnosis), treatment with androgen deprivation therapy (ADT), and diagnosis of metastatic prostate cancer [Citation6–8].
A recent meta-analysis investigated which factors predicted suicide in the general population [Citation9]. The top five risk factors for death by suicide were prior psychiatric hospitalization, prior suicide attempt, prior suicide ideation, lower socioeconomic position, and stressful life events pointing to the complex interplay between risk factors. However, to our knowledge, no study has investigated the effect of previous psychiatric morbidity on the risk of suicide after a prostate cancer diagnosis.
Suicide risk in cancer patients vary substantially between cancer sites, and among prostate cancer patients, the results are inconsistent. A meta-analysis of observational studies comparing 1,281,393 prostate cancer patients with 842,294 matched prostate cancer-free men indicated a two-fold higher risk of suicide among men with prostate cancer (relative risk (RR) 2.01, 95% confidence interval (CI) 1.52–2.64) [Citation6]. Contrary to this result, a nationwide UK cohort study of almost 5 million cancer patients including 594,521 men with prostate cancer observed that prostate cancer patients were at a lower risk of suicide compared with the background population (standardized mortality ratio 0.90, 95% CI, 0.82–0.99) [Citation10]. Differences in the results of these studies may arise, from differences in the clinical setting and the level of surveillance between populations [Citation6,Citation10], the selection of comparisons, and controlling for confounding [Citation6].
We present a population-based cohort study on the risk of suicide among men with prostate cancer to address limitations in earlier studies. We investigate the association between a prostate cancer diagnosis and the risk of suicide and further whether this association is modified by the presence of previous depression. The aim is to test the hypothesis of a significant impact of previous depression on the risk of suicide in prostate cancer patients compared with cancer-free men with previous depression after adjustment for confounding by clinical and socioeconomic factors.
Material and methods
Study design and setting
This longitudinal registry-based study included prostate cancer patients diagnosed from 1998 to 2011 identified in the Danish Prostate Cancer Registry (DaPCaR). This registry holds information on all histological examinations of prostate tissue in Denmark between 1995 and 2011 [Citation11]. A cohort of cancer-free men matched by age at the date of diagnosis (index date) was generated from the Danish background population with a 1:20 ratio to the men with prostate cancer. First, we studied how exposure to a prostate cancer diagnosis affected suicide risk, and whether this effect differed or was modified by a previous diagnosis of depression. Secondly, we estimated the magnitude by which previous depression affected suicide risk among men diagnosed with prostate cancer and cancer-free men. All study participants were followed from the date of diagnosis/index date until suicide, death from other causes, change of exposure status (from no prostate cancer to prostate cancer), emigration, loss to follow-up, or 31 December 2016, whichever came first.
Participants
We included men from 1998 to consider the use of antidepressants within three years before diagnosis in all study participants; this information was obtained from the Danish Prescription Registry established in 1995 [Citation12]. Through the Danish Civil Registration System, we obtained information on the cohort of cancer-free men and the vital status for all included men [Citation13]. Eligibility criteria in both cohorts included no previous cancer and no previous major psychiatric disorder apart from depression (ICD-10 F00-F31). Previous cancer and psychiatric morbidity other than depression were assumed to increase the risk of suicide, which could bias the results.
Variables and data sources
The primary outcome was suicide defined as the registration of the underlying cause of death as ICD-10 codes X60-84 and Y87.0 in the Danish Causes of Death Registry [Citation14]. Previous depression was defined as either a hospital contact for depression (ICD-10 codes F32-33) or a filed antidepressant prescription (ATC code N06A) within three years before the date of diagnosis/index date. Information on cohabitation status the year of diagnosis and socioeconomic position as measured by the income quintile the year before diagnosis were obtained from registers on personal income administered by Statistics Denmark [Citation15], and comorbidity were obtained from the national patient register [Citation16]. Comorbidity was assessed as Charlson comorbidity indexes based on the sum of 15 weighted somatic conditions up to ten years before the date of diagnosis/index date [Citation17]. Data on the presence of metastases at diagnosis and the D’Amico risk group based on prostate-specific antigen (PSA) level, Gleason score, and clinical T-stage were obtained from DaPCaR [Citation18].
Statistical methods
Cumulative incidences of suicide were calculated for prostate cancer patients and cancer-free men with death from other causes as a competing risk.
For the main analysis of the hazard of suicide in prostate cancer patients compared with cancer-free men, we did an age-adjusted (including age as a continuous variable) Cox regression model with time since the index date as the underlying time scale (Model 1). Information on previous use of antidepressants were included in an additive model (Model 2). We included an interaction term in the model to investigate whether the association between prostate cancer diagnosis and suicide risk was modified by a previous depression (Model 3).
Due to the questionable proportionality of the hazards, we modeled the Cox regression coefficients in time intervals with time since diagnosis/index date, and we performed a sensitivity analysis calculating the hazard of suicide within the first year after diagnosis, using the same models as in our main analyses. Since suicide is a rare event, this estimate gives us the opportunity to evaluate the proportions of the problem.
The incidence of suicide was illustrated in prostate cancer patients with and without previous depression using cumulative incidence functions with death from other causes as a competing risk. We further illustrated the cumulative incidence of suicide according to the presence of metastases (categorized as M0, M+, or Mx) and the D’Amico risk group at diagnosis (categorized as low, intermediate, or high risk). Missing data on PSA at diagnosis was handled by including a category for an unknown D’Amico risk group.
In the sub-analysis of suicide risk among men with prostate cancer, we first analyzed the suicide risk in an age-adjusted model, including age as a continuous variable (Model A). Secondly, we included information on the presence of metastases at diagnosis in Model B. Lastly, we included the following possible confounders in Model C: calendar period (categorized into three groups: 1998–2002, 2003–2007, and 2008–2011), cohabitation status (living with a partner vs living alone), income quintile, and Charlson comorbidity index (grouped into 0, 1 and 2+). All analyses were performed in R version 3.4.2.
Ethics
The Danish National Health Data Authority (file number FSEID-00002771) approved the study protocol, and reporting was guided by the Strengthening of the Reporting of Observational Studies in Epidemiology (STROBE) recommendations and the Guidelines for reporting of statistics for clinical research in urology [Citation19,Citation20].
Results
After the exclusion of 4177 men with previous cancers and 883 with major psychiatric disorders, we established a cohort of 37,527 men diagnosed with prostate cancer. After the exclusion of 26,420 with previous cancers and 11,118 with major psychiatric disorders, we yielded a cohort of 357,384 cancer-free men for the main analysis (see flow chart in Appendix ). Suicide rates, median age, and comorbidity index did not vary between the men with prostate cancer and cancer-free men (). Among prostate cancer patients, more men with than without previous depression lived alone and had a substantially worse comorbidity burden at the time of diagnosis. Clinical characteristics did not differ between prostate cancer patients with previous depression and those without previous depression.
Table 1. Characteristics of 37,527 men diagnosed with prostate cancer between 1998 and 2011, and 357,384 cancer-free men from the background population.
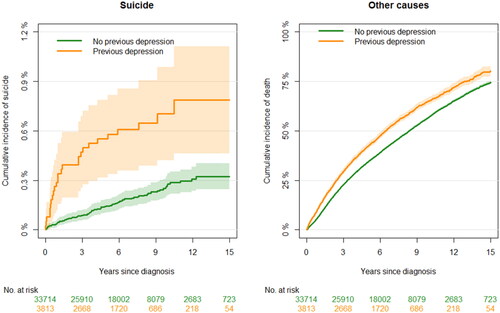
During the study period, 1239 cancer-free men and 108 prostate cancer patients were registered with suicide as the cause of death (). Among prostate cancer patients with a previous depression, 26 were registered with suicide as the cause of death, corresponding to almost a quarter of the total events in this group of patients. Cumulative incidences of suicide did not differ between prostate cancer patients and cancer-free men (), and in the main analysis, there was no statistically significant difference in the hazard of suicide between men with prostate cancer and cancer-free men (). This association did not differ significantly according to the presence of a previous depression (p = .12); the hazard ratio (HR) for suicide in prostate cancer patients with previous depression was 1.39 (95% CI, 0.91–2.10) compared with cancer-free men with previous depression (, Model 3), declining after diagnosis/index date (Appendix ).
Figure 1. Cumulative incidence of suicide (ICD-10: X60-84, Y87.0) and death from other causes as a competing event. Figures include 37,527 men with prostate cancer and 317,246 cancer-free men from the background population (comparison group). Exposure to prostate cancer was assessed as a time-varying covariate, i.e., a man could shift groups from unexposed to exposed. Please note the differing y-axes.
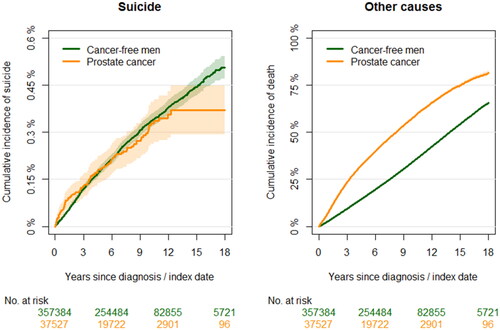
Table 2. Hazard ratios (HRs) for suicide with 95% confidence intervals (CIs).
Within the first year after diagnosis, 26 prostate cancer patients were registered with suicide as the cause of death of which 11 had a previous depression. In contrast to the results above for the entire period, sensitivity analysis confined to the first year after diagnosis showed that the hazard of suicide in men with prostate cancer was increased by 1.72 compared with cancer-free men (95% CI, 1.11–2.59) (). Further, previous depression was a significant risk factor for suicide in the first year after diagnosis (, Model 2). However, when introduced in the model as an interaction term, a previous depression did not significantly modify the relative effect of a prostate cancer diagnosis on the risk of suicide (p = .24) (, Model 3) although the HR was high among prostate cancer patients with a previous depression (HR, 2.38. 95% CI, 1.21–4.67). The suicide rate among prostate cancer patients with a previous depression was 308 per 100,000 person-years and 46 per 100,000 person-years among prostate cancer patients without a previous depression.
Table 3. Hazard ratios (HRs) with 95% confidence intervals (CIs) for suicide within the first year after diagnosis.
Among men with prostate cancer, the cumulative incidence of suicide was higher in the group of men with previous depression with a rapid rise in the first year after diagnosis (). No differences were found between cumulative incidences of suicide stratified on the presence of metastases and the D’Amico risk profile ( and ). Sub-analysis showed that living alone and having comorbidity at the time of diagnosis were significant risk factors for suicide (Appendix ). Among prostate cancer patients, the HR for suicide in those with previous depression declined with time since diagnosis compared with those without previous depression ().
Discussion
As expected, the number of suicides was low among prostate cancer patients. However, a significant proportion of the suicides was registered among patients with a previous depression or within the first year after diagnosis. Prostate cancer patients had a 1.70-fold increased risk of suicide during the first year after diagnosis compared with cancer-free men, and patients with previous depression were especially vulnerable. We found, however, no long-term overall increased risk of suicide in prostate cancer patients compared with cancer-free men. Within the group of prostate cancer patients, neither the D’Amico risk group nor the presence of metastases were significantly associated with the risk of suicide.
Interpretation
Our findings could indicate that healthcare professionals, in general, need to be aware of suicidal thoughts and depressive symptoms among prostate cancer patients who have a history of depression in the immediate aftermath of the diagnosis. Several other studies have also found the highest suicide risk in cancer patients immediately after diagnosis [Citation5,Citation6,Citation10]. Previous depression and suicide are intuitively associated, but few studies of cancer patients have included this significant risk factor in investigations of suicide risk. To our knowledge, only a Canadian study has included information on pre-diagnostic psychiatric care use in a population-based investigation of suicide risk in cancer patients [Citation21]. Cancer-free comparisons from the general population were matched on the level of psychiatric care use in a 5-year pre-diagnostic period [Citation21]. The findings suggested that the risk of suicide was higher in cancer patients than comparisons during the first 50 months after diagnosis (HR, 1.60; 95% CI, 1.42–1.81) [Citation21]. However, in a subgroup analysis with stratification on cancer type, the suicide risk did not differ significantly between prostate cancer patients and cancer-free comparisons (HR 1.07, 95% CI, 0.90–1.27) [Citation21]. Overall, the findings of the Canadian study seem to align with our results; however, we did not match on previous depression but instead examined if the effect of a prostate cancer diagnosis varied according to having had a previous depression. In other words, we considered previous depression as an effect modifier and not as a true confounder, which could help identify a vulnerable population of prostate cancer patients at increased risk of suicide and therefore enable us to estimate the extent of the effect in both prostate cancer patients and the cancer-free comparisons.
A meta-analysis of eight observational studies found a substantially increased risk of suicide (RR 2.01, 95% CI, 1.52–2.64) in prostate cancer patients compare to cancer-free comparisons [Citation6]. None of the included studies included information on pre-diagnostic depression or other psychiatric morbidities as potential risk factors and the meta-analysis found significant heterogeneity in terms of variation in the control for confounders and variation in the clinical settings between studies included [Citation6], which could explain the differing of the results from those of this present study.
The mechanism underlying the association between previous depression and suicide in prostate cancer patients is uncertain. Prostate cancer treatment may affect the association with a previous depression and thereby the risk of suicide; however, we did not have information on treatment in this study. Nevertheless, we would hypothesize that treatment with ADT would increase the suicide risk as men receiving this treatment have an increased risk of depression compared with men who were unexposed or less exposed to ADT as shown in a meta-analysis by Nead et al. (RR 1.41, 95% CI, 1.18–1.70) [Citation22]. In a Danish cohort, we have previously shown that prostate cancer patients receiving ADT in combination with radical prostatectomy had a higher risk of depression compared with patients treated with radical prostatectomy alone [Citation23], and the association was further confirmed by Guo et al. [Citation6]. The hypothesis is strengthened by our finding of a 1.49-fold increased risk of suicide (although not statistically significant) among men with metastatic disease, who are the patients most likely to commence on ADT – and the ones with the poorest prognosis. A few studies have compared suicide risk in men with and without ADT [Citation24–26]. These found deviating and uncertain evidence of an association between ADT and the risk of suicide; however, the studies were limited by a few events [Citation24], small study samples [Citation25], and cross-sectional design [Citation26]. Adverse effects from primary curative treatment might also contribute to the association: incontinence and erectile dysfunction are associated with an increased risk of depression [Citation27,Citation28], and lower urinary tract symptoms, in general, have been suggested to increase the odds of suicidal ideation [Citation29]. In our sub-analyses, living alone and comorbidity were identified as risk factors for suicide, and although we did not find any association with income this could indicate that men with a low socioeconomic position may be especially vulnerable for suicide after a prostate cancer diagnosis. Many other possible factors including psychological distress, hopelessness, and social isolation could explain some of the underlying association; however, the entire conceptual framework is most likely complex, and future research should focus on including multiple risk factors simultaneously to help identify the most sensitive and specific predictors of suicide [Citation30].
Strengths and limitations
This study is the first to investigate the effect of previous depression on the association between prostate cancer and the risk of dying by suicide. Furthermore, this study represents one of a few nationwide population-based studies of the suicide risk in prostate cancer patients compared with cancer-free men. A significant strength of the study is the use of nationwide registry-based data with minimal risk of selection- and attrition bias in a longitudinal study design; this ensures high generalizability of the results. The prostate cancer cohort was identified in DaPCaR, which is based on pathology reports ensuring the validity of the prostate cancer diagnoses. Furthermore, the ability to link data from DaPCaR to the Prescription Registry allowed for consideration of not only the most severe cases of previous depression that require hospital admission but the much broader spectrum of moderate to severe pharmaceutically treated depression. To avoid contamination bias in terms of other critical illnesses affecting the suicide risk, we excluded men with other major psychiatric disorders (ICD-10 codes F00-F31) and cancers before the index date. We addressed confounding by including comorbidity, income, cohabitation status, the risk profile of the disease, and the presence of metastases at diagnosis in statistical analyses. The use of antidepressant prescriptions as a proxy for depression may underestimate depression rates, potentially introducing information bias. Nonetheless, rates of depression treated non-pharmaceutically are assumed similar in cancer-free men and men who receive a prostate cancer diagnosis; consequently, misclassification would be non-differential and thereby not pose an interpretation problem.
Conclusion
The management of psychological morbidity is an important aspect of care in the large and growing population of long-term prostate cancer survivors. However, the absolute risk of suicide following a prostate cancer diagnosis was low. Time since diagnosis and a history of depression was associated with the highest risk of suicide. Despite the low absolute risk for suicide among prostate cancer patients, healthcare professionals should be aware of an increased risk among patients with a previous depression, especially in the immediate aftermath of the diagnosis due to a relatively high baseline risk among these men.
Supplemental Material
Download PDF (18.3 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data Availability statement
Access to data can be obtained by request to the corresponding author and the Danish data protection authorities.
Additional information
Funding
References
- Rawla P. Epidemiology of prostate cancer. World J Oncol. 2019;10(2):63–89.
- Friberg AS, Brasso K, Larsen SB, et al. Risk of depression after diagnostic prostate cancer workup – a nationwide, registry-based study. Psychooncology. 2021;30(11):1939–1947.
- Amiri S, Behnezhad S. Cancer diagnosis and suicide mortality: a systematic review and meta-analysis. Arch Suicide Res. 2020;24(Suppl 2):S94–S112.
- Brunckhorst O, Hashemi S, Martin A, et al. Depression, anxiety, and suicidality in patients with prostate cancer: a systematic review and meta-analysis of observational studies. Prostate Cancer Prostatic Dis. 2021;24(2):281–289.
- Robson A, Scrutton F, Wilkinson L, et al. The risk of suicide in cancer patients: a review of the literature. Psychooncology. 2010;19(12):1250–1258.
- Guo Z, Gan S, Li Y, et al. Incidence and risk factors of suicide after a prostate cancer diagnosis: a meta-analysis of observational studies. Prostate Cancer Prostatic Dis. 2018;21(4):499–508.
- Carlsson S, Sandin F, Fall K, et al. Risk of suicide in men with low-risk prostate cancer. Eur J Cancer. 2013;49(7):1588–1599.
- Bill-Axelson A, Garmo H, Lambe M, et al. Suicide risk in men with prostate-specific antigen-detected early prostate cancer: a nationwide population-based cohort study from PCBaSe Sweden. Eur Urol. 2010;57(3):390–395.
- Franklin JC, Ribeiro JD, Fox KR, et al. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol Bull. 2017;143(2):187–232.
- Henson KE, Brock R, Charnock J, et al. Risk of suicide after cancer diagnosis in England. JAMA Psychiatry. 2019;76(1):51–60.
- Helgstrand JT, Klemann N, Røder MA, et al. Danish Prostate Cancer Registry – methodology and early results from a novel national database. Clin Epidemiol. 2016;8:351–360.
- Pottegård A, Schmidt SAJ, Wallach-Kildemoes H, et al. Data resource profile: the Danish National Prescription Registry. Int J Epidemiol. 2017;46(3):798–798f.
- Schmidt M, Pedersen L, Toft H. The Danish civil registration system as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549.
- Helweg-Larsen K. The Danish register of causes of death. Scand J Public Health. 2011;39(7 Suppl):26–29.
- Baadsgaard M, Quitzau J. Danish registers on personal income and transfer payments. Scand J Public Health. 2011;39(7 Suppl):103–105.
- Lynge E, Sandegaard JL, Rebolj M. The Danish national patient register. Scand J Public Health. 2011;39(7 Suppl):30–33.
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383.
- D’amico A V W, Richard M, Bruce S, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280(11):969–974.
- von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457.
- Assel M, Sjoberg D, Elders A, et al. Guidelines for reporting of statistics for clinical research in urology. BJU Int. 2019;123(3):401–410.
- Klaassen Z, Wallis CJD, Chandrasekar T, et al. Cancer diagnosis and risk of suicide after accounting for prediagnosis psychiatric care: a matched-cohort study of patients with incident solid-organ malignancies. Cancer. 2019;125(16):2886–2895.
- Nead KT, Sinha S, Yang DD, et al. Association of androgen deprivation therapy and depression in the treatment of prostate cancer: a systematic review and meta-analysis. Urol Oncol. 2017;35(11):664.e1–664.e9.
- Friberg AS, Dalton SO, Larsen SB, et al. Risk of depression after radical prostatectomy - a nationwide registry-based study. Eur Urol Oncol. 2021;4(4):601–608.
- Patasius A, Kincius M, Kazlauskas E, et al. The role of androgen–deprivation therapy on suicide among patients with advanced prostate cancer: a nationwide population–based cohort study. Psychooncology. 2019;28(10):2098–2100.
- Juurlink DN, Herrmann N, Szalai JP, et al. Medical illness and the risk of suicide in the elderly. Arch Intern Med. 2004;164(11):1179–1184.
- Recklitis CJ, Zhou ES, Zwemer EK, et al. Suicidal ideation in prostate cancer survivors: understanding the role of physical and psychological health outcomes. Cancer. 2014;120(21):3393–3400.
- Martin S, Vincent A, Taylor AW, et al. Lower urinary tract symptoms, depression, anxiety and systemic inflammatory factors in men: a population-based cohort study. PLOS One. 2015;10(10):e0137903.
- Suija K, Kerkelä M, Rajala U, et al. The association between erectile dysfunction, depressive symptoms and testosterone levels among middle-aged men. Scand J Public Health. 2014;42(7):677–682.
- Breyer BN, Kenfield SA, Blaschko SD, et al. The association of lower urinary tract symptoms, depression and suicidal ideation: data from the 2005–2006 and 2007–2008 national health and nutrition examination survey. J Urol. 2014;191(5):1333–1339.
- Nock MK, Ramirez F, Rankin O. Advancing our understanding of the who, when, and why of suicide risk. JAMA Psychiatry. 2019;76(1):11–12.
Appendix
Figure A1. Flowchart of the cohorts included in the study. In the main analyses, all men with prostate cancer between 1998 and 2011 and a comparison cohort of cancer-free and prostate cancer diagnostic workup-free men age-matched at a ratio of up to 1:20 on the date of diagnosis (index date) were included, while the sub-analysis included the prostate cancer patients alone.
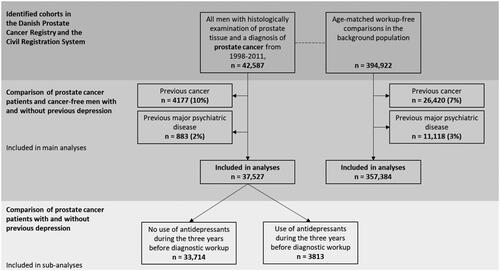
Figure A2. The time-dependent hazard ratio (HR) with 95% confidence intervals (dotted lines) for suicide in prostate cancer patients with prior depression compared with cancer-free men with prior depression.
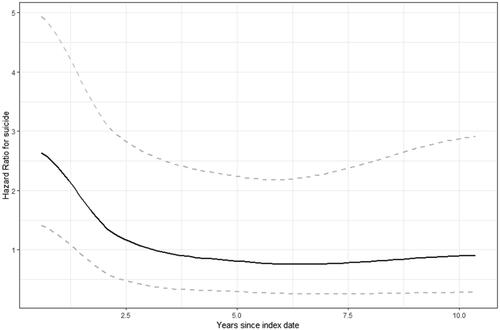
Figure A3. Cumulative incidence of suicide (ICD-10: X60-84, Y87.0) and death from other causes as a competing risk among 37,527 men with prostate cancer stratified on the presence of metastases at the time of diagnosis. Please note that y-axes differ.
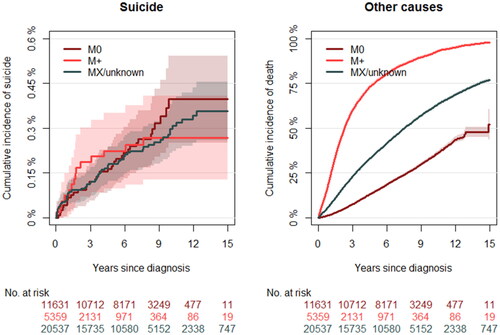
Figure A4. Cumulative incidence of suicide (ICD-10: X60-84, Y87.0) and death from other causes as a competing event among 34,519 men with prostate cancer stratified on D’Amico risk group at diagnosis (missing information on 3008 individuals). Please note that y-axes differ.
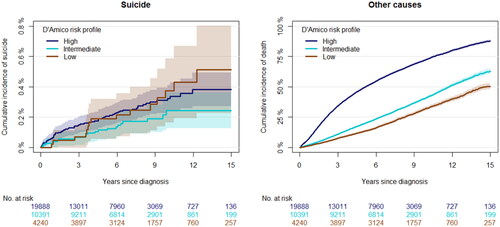
Figure A5. Hazard ratio (HR) with 95% confidence intervals (dotted line) for suicide in prostate cancer patients with previous depression compared with prostate cancer patients without depression.
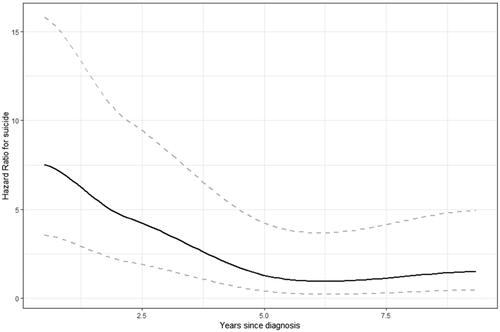
Table A1. Hazard ratios (HR) for suicide with 95% confidence intervals (CI) among 37,527 prostate cancer patients diagnosed in Denmark between 1998 and 2011.