Abstract
Background
Cancer, especially breast cancer, remains a public health problem because of its negative consequences, which require long-term programs to alleviate its devastating effects. This study aimed to examine unmet supportive care needs and health-related quality of life of females with breast cancer.
Methods
A cross-sectional study with a mixed-method design was employed. A simple, randomly selected sample of 352 females attending Al-Rantisi and Al-Amal hospitals was included in this study. A validated Arabic version of the Supportive Care Needs Survey (34 items) and The European Organization for Research and Treatment of Cancer Quality of Life (EORTC QLQ-C15-PAL) were used. Moreover, twenty-five semi-structured interviews were performed (13 females, eight husbands, and four healthcare workers). Quantitative data were analysed using descriptive and inferential analysis, whereas thematic analysis was used for qualitative data to highlight main themes.
Results
The highest unmet need reported by females with breast cancer was psychological needs (63%), followed by health-related systems and information (62%) and physical and daily life (61%). Pain and fatigue were the most reported symptoms (65.8% and 62.5%, respectively), followed by emotional distress, physical function, and physical symptoms; 55.8%, 54.3%, and 51.5%, respectively. These unmet needs and health-related quality of life-related dimensions were highlighted and elicited by qualitative data analysis. Unmet needs are high among married females, on conservative treatments, young females (< 40 years old), and females in the first year of diagnosis. The presence of chronic diseases did not increase needs. However, health-related quality of life was affected. Six themes are subtracted: availability of anticancer therapy, affordability of healthcare, family and social support, psychological support, health education, and self-image & intimate relationship.
Conclusion
Many needs are unmet. Caring for females with breast cancer should be comprehensive to fill gaps, including psychological care, health information and education, physical care and support, and medical care.
Introduction
Cancer is one of the significant causes of morbidity and mortality, with approximately 14.1 million new cases and 8.2 million fatalities worldwide [Citation1]. Breast cancer (BC) remains a significant public health issue in developed and developing countries, accounting for 25.1% of all cancers [Citation2,Citation3]. It has tremendous social and economic consequences and is the leading cause of morbidity and mortality [Citation4,Citation5]. BC is a disease that is well understood and treatable, especially in developed countries, and more women now survive the disease than die from it. For women in Palestine, the situation is far bleaker. The condition is the most common and widely spread type of cancer; its mortality reached 9.8% of all cancers. Palestinian women make up 32.3% of cancer cases reported in the Gaza Strip, with a prevalence of 149.1 cases per 100,000 population. Between 2017 and 2018, 8326 new BC cases were registered, accounting for 18% of all reported cancers [Citation6].
Identifying cancer patients’ needs and interventions to approach these needs are based on an assessment of unmet needs and health-related quality of life (HRQoL), which are conceptually two different morbidity outcomes. According to a study involving 117 patients with breast, prostate, and lung cancer, assessment of needs helps identify patients with critical HRQoL, necessitating clinicians’ attention [Citation7]. A large sample size of a mixed cancer population supports the evidence that unmet needs are an essential indicator of HRQoL in the early survivorship phase for a broad group of cancer patients [Citation8]. Unmet needs were significantly associated with all aspects of HRQoL and psychological distress [Citation8].
Cancer patients face various symptoms and issues in their daily lives, including physical, psychological, and socioeconomic side effects of treatment and disease complications. The international cancer treatment guidelines advise using a multidisciplinary team to evaluate and address patients’ needs for supportive care. Numerous symptoms and problems must be managed, including pain [Citation9], distress [Citation10], insufficient social support [Citation11], and treatment location [Citation12].
Identifying the patients’ care needs using a patient-centred approach and effectively meeting those needs is now recognised as a crucial component of cancer patients’ integrated healthcare management. Before, during, and after diagnosis, throughout treatment, and during the terminal phase, needs are assessed. Research has linked the early incorporation of supportive cancer care services to improved patient health outcomes in terms of overall survival, functional and cognitive status, performance status, and the proportion of patients with uncontrolled symptoms, as well as a higher quality of life [Citation13,Citation14]. Cancer patients’ unmet care needs tend to arise in the early stages of cancer survival, which negatively impacts patients’ quality of life. The frequency and seriousness of a problem determine whether to refer a patient to supportive care services [Citation13,Citation15].
Studies have shown that medical professionals frequently fail to address patients’ symptoms and problems [Citation16] adequately. Additionally, patients’ and clinicians’ perceptions of needs often diverge [Citation17]. Patients’ care needs come in many forms, including physical, practical/daily life activities, economic, environmental, cultural, knowledge, communication, emotional, psychosocial/psychosexual, functional/valuable/daily life activities, and spiritual/existential areas [Citation18]. In the Gaza strip, limited studies were found, and palliative care services are not well-framed [Citation19] and psychosocial care, home management should be given significant attention and adopting a multi-disciplinary team approach to shape the comprehensiveness of care [Citation20]. This study aimed to examine the unmet needs of females with breast cancer and its association with HRQoL.
Materials and methods
Study design
A convergent mixed method design was used, in which qualitative and quantitative data were collected simultaneously. The findings from both approaches were compared and related.
Study setting
Cancer services are concentrated at two leading hospitals; one in Gaza city and the second in the southern part of the Gaza strip. The study took place at Al Rantisi specialised hospital and Al-Amal hospital. The first one is located in Gaza city, while the second serves patients of southern governorates.
Study population, sample size and sampling
The study population was all females of all ages diagnosed with breast cancer at any stage and under/under no treatment from 2014-2020. They are approximately 1500 females diagnosed with breast cancer between 2014 to 2020. Moreover, females husbands and healthcare workers, who provide health services to those females, were also included.
An online sample size calculator (https://www.surveysystem.com/sscalc.htm) estimated the sample size was 306 with a 95% confidence interval. The sample size calculation was based on the assumption that 50% of females with breast cancer are satisfied or have no needs, and 50% are not satisfied and have unmet needs. A 10% non-response rate was added to 306 patients (306 + 31 = 337). In the end, the sample size was raised to 360.
For the quantitative study, simple random sampling was approached to select participants from a pre-prepared list. Purposive sampling from different age groups was followed to select participants for interviews. Thirteen females, who had BC for 12 months or more without looking at the disease stage, were recruited for interviews, in addition to 10 husbands. Four nurses and physicians were interviewed further to explore the unmet needs of females with breast cancer.
Inclusion criteria
Females (>18 years old)
Confirmed diagnosis of breast cancer regardless of stage, time since diagnosis, or status of treatment
Capable of understanding the questionnaire
Had visited a hospital for cancer treatment within the past 12 months
Exclusion criteria
Severe physical or psychological problems result from other medical issues.
Not willing to participate
Ethical consideration
Ethical clearance was obtained from the Palestinian Health Research Council (PHRC/HC/807/21), followed by permission from the General directorate of human resources development, the ministry of health (No: 634365). Written informed consent was obtained from each participating female in the quantitative study and interviewees of the qualitative study. Study objectives were presented before consent was administered. Anonymity and voluntary participation were ensured, and data were kept confidential in the corresponding author’s closet.
Instruments
The Arabic version of the European Organization for Research and Treatment of Cancer Quality of Life (EORTC QLQ-C15-PAL -15 items), developed by Alawneh et al. [Citation21], was used to measure QoL. The 15-item structured instrument measures two functional health dimensions (emotional functioning [2 items] and physical functioning [3 items]), symptoms dimensions (like sleeplessness and dyspnea, nausea/vomiting, loss of appetite, constipation [5 items]), fatigue (2 items), and pain (2 items), in addition to global quality of life (QoL). Questions are answered on four-point Likert scales (not at all, a little, quite a bit, very much). The global QoL is measured on 7 points Likert scale.
The Supportive Care Needs Survey (SCNS-34) was also used to examine unmet care needs. It contains 34 items in five domains: psychological needs (10 questions), health system and information needs (11 questions), physical and daily living needs (5 items), patient care and support needs (5 items) and sexuality needs (3 items). Items are responded to on a five-point Likert scale (not applicable = 0, satisfied = 1, low need = 3, moderate need = 4, high need = 5). The SCNS-34 was developed by Boyes, Girgis, and Lecathelinais [Citation22] and later was translated into many languages except Arabic. The instrument was translated into Arabic and tested for its reliability and validity. The overall alpha Cronbach of the SCNC-34 was 0.79 (ranging from 0.73 to 0.84) and was shown to be content valid as measured by the item content validity index (I-CVI > 0.90) and scale content validity index (S-CVI >0.88).
Semi-structured interview guides were prepared to collect necessary information from participants (females with breast cancer, their husbands and health care workers). The interview guide enclosed 13 questions for health workers, 16 for females with breast cancer and ten for husbands, with the possibility of probing in each question for all interviewees.
Data collection and analysis
After three hours of structured training, four qualified and trained student nurses collected the quantitative data from September to December 2021. The three hours of training for data collectors covered communication techniques, goals, objectives and research questions of the study, the questions themselves and potential misconceptions. Data were collected through a face-to-face interview. Participants were asked to come to the hospitals mentioned above during the morning duty shift. Data regarding socio-demographic and clinical variables were collected from the mouths of the patient and medical records, respectively. The authors of the first (AE) and second (MR) collected qualitative data. Interviews with females, their husbands and health workers took place in a separate room, and all interviews were audio-recorded.
The SPSS software version 22 was used in data analysis. Before analysis, data were checked for missing and extreme variables. Descriptive and inferential analyses were performed. Continuous variables (age, years of treatment…) were presented as mean and standard deviation, whereas categorical variables (stage of cancer, place of residency, marital status…) were presented as frequency and percentage. Analysis of the EORTC QLQ-C15-PAL -15 and the SCNS-34 was done separately, in which dimensions of the EORTC QLQ-C15-PAL −15 were presented as M ± SD and weighted mean. The mean value of the EORTC QLQ-C15-PAL -15 and the SCNS-34 dimensions was compared with socio-demographic variables. Paired t-test and ANOVA were used accordingly, and a p-value less than 0.05 was considered statistical significance.
Results on supportive care needs were presented as no needs (not applicable, satisfied) and some needs (low need, Moderate need, high need). Patients who reported either not being helpful or satisfied were considered to have no need. At the same time, patients who answered low, moderate or high need were believed to have some requirements. Therefore, patients who scored three and above are considered to have needs. Patients’ answers to the SCNS-34 were squeezed from 5 points to a 2-point Likert scale and were coded as 1 (some needs) or 0 (no needs).
Thematic analysis was approached in the study of qualitative data. Thematic coding includes creating themes from qualitative data. From the collection of unprocessed qualitative data to the discovery of codes and themes, several approaches were used, including immersion and familiarization, the creation of preliminary codes, the search for and review of themes, the definition and naming of themes, and the creation of the report [Citation23]. The theme analysis combined all transcripts into a single, comprehensive dataset. This analysis offers a broader perspective on the subject of interest. A professional transcriptionist transcribed all audio recordings of interviews verbatim into word documents, which were then read and reread numerous times, as well as the tapes themselves several times to confirm the transcription’s accuracy. The materials were kept with the first author to save confidentiality and will be discarded appropriately.
We carefully studied the transcripts line by line to understand them as a whole before creating the initial codes for the data. A second in-depth investigation of the principles was carried out to find potential themes using a word document. Then, all identified articles were compared to all of the data that had been extracted. To ensure no information was lost, we made the time-consuming decision to code for as many different themes as possible.
Then we again went through the texts, aggregating the codes that revealed numerous critical assertions into clusters within the exact text. To illustrate the relationship between codes and themes, a thematic map was made. These assisted us in seeing and thinking about the connections between concepts. Any themes that were too diverse or lacked sufficient evidence to support them were dropped at this step.
Results
Characteristics of participants
Three hundred fifty-two women agreed to participate in the quantitative study (response rate 97.7%). The mean age was 51.63 ± 12.97 years. Three-quarters of women were married, and most of them were homemakers. Most females were housewives (85.2%), and 4.6% were employees. Most females (67.2%) lived in families with incomes less than 1000 New Israeli Shekel (NIS). Nearly 10% of the females were illiterate. The majority had breast cancer duration of fewer than six years (79.5%), 50% underwent a total mastectomy, one-third had a family history of breast cancer, and 37.2% had chronic diseases (hypertension, diabetes mellitus, heart disease, …) ().
Table 1. Socio-demographic characteristics of respondents (from mouth of patients n = 352).
Table 2. Clinical characteristics of respondents (from medical files n = 352).
Twenty-five in-depth interviews were conducted among females (n = 13), husbands (n = 8) and healthcare workers (n = 4). Almost all interviewed females and their husbands were living under the poverty line with income less than 1000NIS. All females had breast cancer for at least one year and were diagnosed with stage two to three at the time of diagnosis. The themes elicited from the analysis were six; unavailability of anticancer therapy, affordability of healthcare, family and social support, psychological support, health education, and self-image & intimate relationship.
Health-related quality of life (HRQOL)
HRQOL was measured on a four-point Likert scale using the EORTC QLQ-C15, which has five domains: physical function, fatigue, pain, physical symptoms and emotional status. In addition, one question measured the overall health status/quality of life. Generally, the mean score of females’ responses to the general health status question/quality of life was 4.80 ± 1.29 and the mean score of the EORTC QLO-C15-PAL, including the general question of health, was 2.42 ± 0.58 ().
Table 3. Quality of life (pain, fatigue, physical symptoms, physical function and emotional subscale) of respondents (n = 352).
1. Physical function
The mean score was 2.17 ± 0.85. One-fourth (89/352) claimed they had no problem walking around the home, whereas two-thirds had somehow high trouble (222/352). Half of the women were required to stay in bed/chair during the day (169/352). In return, little dressing of help is needed, and eating or using the toilet (50/352, 14.2%).
2. Pain
The mean score of perceived pain was 2.63 ± 0.93. More than 50% of women had pain (191/352), significantly interfering with their daily activities (225/352, 63.9%).
3. Fatigue
The mean score was 2.50 ± 0.91. The majority of women reported feelings of weakness and tiredness. However, the feeling was high in 18.8% and 17.9%, respectively. Two-thirds reported weakness and fatigue (35.9% and 34.9%, respectively).
4. Physical symptoms
The overall mean score was 2.06 ± 0.69. Shortness of breathing and trouble sleeping were commonly reported problems by women. The symptoms were from mild to high (51.1% and 54.7%, respectively). More than half reported no nausea or constipation (54.4% and 62.9%, respectively).
5. Emotional status
The mean score was 2.23 ± 0.99. Half of participating women perceived having a feeling of depression ranged from low to high. However, feeling tense was much higher (72.6%).
Assessment of supportive care needs using the SCNS-34
Results are presented based on the quantitative and qualitative analyses
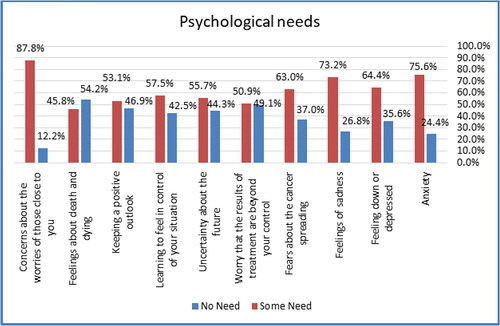
1. Psychological needs:
The mean score for this dimension was 1.63 ± 0.30 on a two-point Likert scale. Three-quarters of participating females reported having anxiety (266/352) and feelings of sadness (257/352). The majority had concerns and were worried about closers (309/352, 87.8%), whereas around two third had a problem with cancer spreading (221/352, 63%). The last concern was around feeling about death and dying (157/352, 57.9%) ().
Psychological support emerged as a central concern among most interviewed women. They claimed doctors and nurses in the Gazan governmental hospitals usually did not provide psychological support. Meanwhile, some women claimed that doctors and nurses in Al-Motale’s hospital in Al-Quds (Jerusalem) provided enough psychological support in a more humanitarian manner. However, the women argued that the Gazan doctors and nurses saw many cancer patients daily, so they could not support patients psychologically.
‘…. No one care with the psychological condition…’ (Female, teacher, 34y)
‘…. doctors and nurses did not behave with us as a human being….it seems that they lost their feelings, so who can support us psychologically….’ (Female, housewife, 43y)
Some women believed that psychological support and consultation should be done by a specialized psychologist, not only by doctors or nurses. On the other hand, most women reported that non-governmental organizations/community-based organizations were interested in providing them with such support. This support ranged from providing psychological consultation through a specialized psychologist to providing various recreational activities. There was a general consistency among all women that doctors and nurses should have the most significant role in providing such support as they are the ones who follow patients, step by step, during their disease journey.
‘… the women’s health center used to gather all women with breast cancer even with our families and took us on a journey…the centre provided free transportation and free breakfast and lunch meals.’ (Females, housewife, 36y)
‘… I practiced all the exercises we received from the women’s health center…their exercises were beneficial and alleviated my worries and my psychological status…’ (Females, housewife, 30y)
Females’ partners confirmed that the worst thing that happened to their wives was the deterioration in their psychological status once they had been informed about a cancer diagnosis. The decline has been exacerbated during the chemotherapy stage.
‘…My wife lost their interest to talk, eat, or drink due to cancer…’ (Husband, jobless, 45y)
The healthcare providers reported a multidisciplinary team in Al-Shifa and Naser hospitals, and these teams recently started providing psychological support. The providers acknowledged that such support could have been better systemised and needed to give more support due to time limits.
‘… the psychological support requires more and more activation…’ (physician, breast surgery, 46y)
Another form of psychological support was social and family support. Discussion of family support took up an extended part of the interviews. The vast majority of interviewed females acknowledged the critical role of their husbands and families. Participants provided many examples of how their husbands supported them, e.g., companioning their wives to hospitals on every visit, providing psychological support, and helping with homework. Many women acknowledged the role of their mothers, brothers and sisters in providing psychological and financial support. Some women reported that their friends provided them with enough support through frequent visits, regular telephone calls, or bringing gifts. One of the main helpful ideas was the support from cases with a similar disease, as reported by most interviewed women.
The participants prescribed how they got the benefits and the release of worries after meeting with a group of similar diseases. They listened to each other experiences through the journey of disease. They also used a WhatsApp group to exchange their experiences, advice, and coordinate fun activities. Some women talked about how spiritual support as Muslims positively affected them. Some women overcame the disease severity by increasing their prayers and reading/listening to the Holly Quran. Most women attributed their satisfaction with cancer to their acceptance of God’s decree, while some reported that believing in God’s law was the most effective way to cope with cancer.
‘…My husband asked me not to do makeup or use a wig; he told me that this is from God and everything will come back again…’ (Female, housewife, 36y)
‘…My husband told me that my appearance didn’t’ change and he loved me now more and more…without his support, I did not know how can I fight cancer’ (Female, housewife, 39y)
‘…I could discuss with my friends something that I could not discuss with even my family…’ (Female, housewife, 43y)
‘…I had good relationships with some women with breast cancer. I felt comfortable talking with someone with the same pain … No one can feel your pain rather than the person with similar pain.’ (Female, housewife, 43y)
‘I used to discuss my case with women with breast cancer; we talked on the treatment, side effects of chemotherapy, the intimate relation…This made me express my feeling freely.’ (Female, teacher, 48y)
‘The one who sees someone else’s pain makes it easy for him…’ (Female, housewife, 36y)
Females’ husbands believed faith in God’s decree was the most powerful coping mechanism to accept cancer.
‘…. Whoever sees someone else’s calamity, makes it easy for him. We believe in Allah…’ (Husband, jobless, 45y)
There was consistency among all husbands that they provided psychological support for their wives. The husband’s support included joining their wives at the hospital, joining their wives in picnics, or letting their families frequently visit their wives. One unexpected expression by some husbands was the massive worry of their wives about the possibility of their husbands marrying a second wife. The husbands did their best to cancel this idea from their wives’ minds as a sort of loyalty and psychological support.
‘…I wished that I was the person who has cancer, not my wife, I can tolerate the pain, but she can’t…’ (Husband, carpenter, 39y)
‘…When my wife had an appointment to a hospital, I woke up so early at Fajr to prepare the taxi and some arrangements and accompany her.’ (Husband, employee, 53y)
‘…I never let my wife hear that I am talking about my intension to marry again.’ (Husband, employee, 55y)
The providers believed that one of the most important priorities is focusing on the psychological aspect of care because of changes in females’ body image after chemotherapy and surgeries.
‘…Our community still doesn’t accept a young wife undergoes to mastectomy; the relations among partners are affected and the second marriage exists, so, the psychological support is necessary…’ (Husband, jobless, 36y)
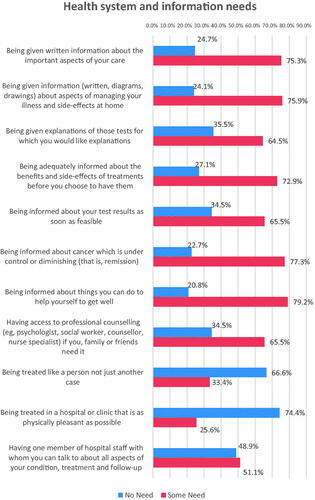
2. Health system and information needs:
The mean score was 1.62 ± 0.31. The most perceived need was information on how to help themselves to get well (278/352, 79.2%) and information about the progress and control of cancer (272/352, 77.3%). Not far away, information about an essential aspect of care and illness management and side-effect at home were also highlighted by three quarters (265/352, 75.3% and 267/352, 75.9%, respectively). More than two-thirds perceived that treatment in a physically pleasant hospital or clinic was unnecessary (262/352, 74.4%) ().
The lack of health education was highlighted as an unmet need among most females. They described the health education in the Gazan governmental hospitals as non-systematized and unplanned in the best circumstances. They claimed doctors and nurses only answered patients’ questions and provided few instructions during the first visit. They justified this as doctors and nurses were so busy due to the high number of cancer cases seen daily. However, most females confirmed that the source of health education was non-governmental organizations such as women’s health centers, internet sites and physicians at their private clinics. They reported that qualified health educators from non-governmental organizations regularly visited patients in governmental hospitals to provide instructions about diet, nutrition, regular self-examination, and follow-up. Non-governmental organizations used different approaches to health education, such as group sessions and the distribution of educational brochures.
‘…I remember that the doctor only told me to avoid the sugars…’ (Female, housewife, 48y)
‘I am a patient, and the doctor should provide us continuous instructions according to his experience…’ (Female, housewife, 43y)
‘A specialized dietician from the women’s health center visited us each Sunday and Thursday to give us written instructions of the food regimen and asked us to feel free to call when necessary’ (Female, housewife, 43y)
‘… I feel that doctors behaved with us as numbers and without feelings, they said that there were overwhelmed with the high number of cases, so they could not provide health education…’ (Female, housewife, 39y)
‘…Why there was no a committee from a doctor, nurse, dietician, psychologist to monthly gather 20-30 patients and educate them on the nature of cancer, prevention, healthy diet, stress release…’ (Female, housewife, 38y)
Despite the health education and instructions provided to patients after mastectomy and during chemotherapy, health workers declared that the current health education is neither complete nor systematic.
‘We don’t provide 100% health education; the providers can’t do everything….’ (physician, breast surgery, 46y)
The health workers agreed with patients that they have limitations in providing a complete and systematic health education due to the heavy workload and time constraints.
‘…Most doctors see a huge number of patients, they can’t stay with each patient and explain everything to him…’ (Head-nurse, 51y), (physician, oncologist, 46y)
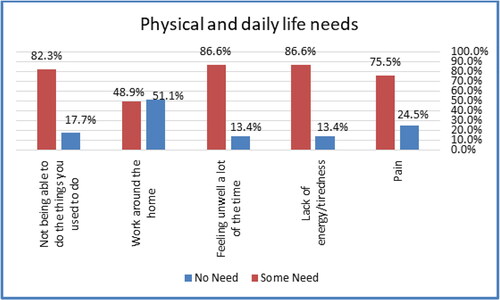
3. Physical and daily life needs
The mean score was 1.61 ± 0.30 on a two-point Likert scale. Most participating women felt unwell most of the time and lacked energy/tiredness or were unable to do things they used to do (303/352,86.6% and 288/352, 82.3%, respectively) ().
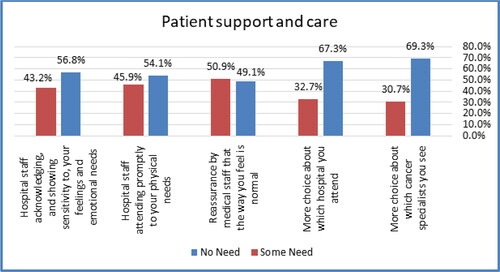
4. Patient support and care needs
The overall mean score was 1.41 ± 0.34, and the most item perceived as a need was that medical staff should reassure patients whether changes in physical and psychological status during the treatment course are as regular as expected unless alarming (179/352, 50.9%). However, other items were perceived as unnecessary, as given by at least half participating women ().
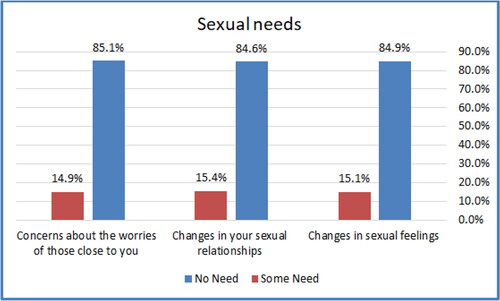
5. Sexual needs
The overall mean score was 1.15 ± 0.34. The majority (≥ 84%) of participating women perceived no need in the sexual aspect of their life. Only 15% perceived changes in sexual feelings and relationships ().
One of the worst experiences raised by all interviewed women as hair loss due to chemotherapy. Many described the loss of hair, eyelashes, and eyebrows as more challenging and painful than chemotherapy. They were very concerned with how hair loss might affect their appearance from the view of their husbands. However, most of them used a wig to cope with this annoying issue. They received the wigs freely from non-governmental organizations such as women’s health centers.
On the other hand, women who performed mastectomies expressed frustration due to how their husbands felt. However, they decided to do breast reconstruction whenever possible. Furthermore, two women claimed that breast reconstruction service was not available in governmental settings, and they were obligated to undergo reconstructive surgery in private facilities.
When the researchers tried to probe how intimate relationship has been affected due to breast cancer or mastectomy, the answers and reactions were not complete. It seems that the sensitivity of such a relation made it difficult to dig deeper. Contrary to our expectations, most women claimed their intimate relationship was normal and their husbands unaffected. The women mentioned that they tried their best to appear normal and curb any opportunity for their husbands to feel upset about their appearance.
‘…I couldn’t imagine that I will catch my hair by my hands…’ (Female, teacher, 34y)
‘…After completing my therapy, I will promptly do breast reconstruction.’ (Female, housewife, 36y)
‘… I became very nervous and depressed after losing my hair…’ (Female, housewife, 43y)
‘… After using the wig, I became less anxious and accepted my case…I don’t want my husband says that I am a sick wife…’ (Female, teacher, 48)
‘…the relation with my husband didn’t change, I didn’t let him feel any difference, I used to use a wig and make-up…’ (Female, housewife, 39y)
‘…My husband told me that I don’t see any change in your appearance; you are more beautiful than before….’ (Female, housewife, 31y)
The husbands expressed mixed feelings towards the intimate relationship. Some of them stated that the relations were not like before the cancer diagnosis, while others mentioned that they accepted the new circumstance. One of the surprising reactions was expressed by a partner who felt he no longer thought of the sexual relationship.
‘…. the relation was changed, how can I practice this relation and my wife has mastectomy!?….’ (Husband, employee, 53y)
‘…. The relationship exists but it is not like before….’ (Husband, carpenter, diploma; driver, BSc; jobless, high. Sec. school; jobless, 36y; EMS, 50y)
The health workers reported that the poor development in breast reconstruction surgery post-mastectomy was still a challenge, despite the satisfactory achievements in the diagnosis and surgical intervention of breast cancer. One oncoplastic surgeon reported that breast reconstruction is complex and requires extensive training and capacity development.
‘…we tried to provide comprehensive care to women with breast cancer, but the less developed breast reconstruction interventions should be considered…’ (physician, breast surgery, 46y)
‘Concerning breast surgeries, we do most of the basic surgeries which are safe and quality; however, we still do the required training for surgeons to provide a developed reconstructive surgery …’ (Physician, breast surgery, 42y)
Another concern women had highlighted as a complication resulting from chemotherapies and might influence sexual and social interaction was tooth loss. The necessary dental services were not available in government health facilities, and thus patients were not affording the cost of dental services in private clinics, which reached 1300 USD. They sought help from non-governmental organizations such as the women’s health center and the Palestinian society for caring for cancer patients.
‘… please see my teeth; I am afraid this shape won’t satisfy my husband. Moreover, I could not laugh or sit with my family, and even I did not attend my brother’s ceremony. My teeth require at least 5500 ILS, and I cannot cover little of them…’ (Female, housewife, 48y)
‘…I went to many societies, but they informed me that they do not support such dental services … they told me they provide only filling or root dental treatment for a minimal number of teeth. This mouth is not attractive’ (Female, teacher, 48y)
‘Indeed, yes, I suffered from tooth loss, and I cannot chew, laugh, speak with my husband and eat properly. I don’t know where dental services are provided for free’ (Female, housewife, 43y)
Other unmet needs explored from the interviews are the unavailability and affordability of anticancer therapy.
Other emerged themes
1. Unavailability of anticancer therapy
There was a consensus among all interviewed women with breast cancer that chemotherapy wasn’t regularly available. Such conditions forced doctors to change the therapy protocol and use other alternatives from available anticancer drugs. Some participants were not satisfied and expressed their worries about this option. The shortage of chemotherapy was one of the main challenges the MoH couldn’t solve during the last few years. According to the MoH monthly reports, a doctor mentioned that the zero stock of chemotherapy reached around 60%. Due to the political conflict and the difficult access to chemotherapy in the West Bank health facilities, the MoH was trying to contract with the private sector inside the Gaza Strip. Unfortunately, few women reported that even in the private sector, there was a delay in receiving the drugs, which reached two or three months. However, in addition to poor early detection, the shortage of chemotherapy could reflect the low average 5-year survival rate among Palestinian women with breast cancer, as a senior nurse revealed.
‘I have been referred to Al-Motale’a hospital, in Jerusalem, due to the lack of chemotherapy and biological therapy inside Gazan hospitals’ (Female, teacher, 34y)
‘… I stayed for two or three months waiting for a call from AL-Hayat center, in Gaza city, to receive my treatment, and when I called them, they said that when the treatment is available, they will call me back’ (Female, housewife, 39y)
‘Many patients lost their right of obtaining the chemotherapy….’ (oncologist, 46y)
‘the hormone therapy was not always available at the governmental hospitals, so I purchased it from my pocket…’ (Female, housewife, 35y)
The husbands agreed with their wives about the unavailability of complementary drugs within the governmental hospitals. The husbands procured multivitamins, minerals, and some analgesics from their pockets or received them with no charges from the women’s health centers or other community-based organizations.
‘… If the women’s health center cannot secure some prescribed medications. I have to purchase them from private pharmacy…’ (Husband, jobless, 48y)
The healthcare providers reported that about 40% of chemotherapy was unavailable. Hence, doctors tried to use other alternatives, like transferring patients to non-governmental hospitals in Jerusalem under government coverage. Biological therapy was often unavailable in Gaza, so patients were transferred for treatment abroad. Similarly, radiation therapy was unavailable in Gaza. The health provider also stressed that lack of chemotherapy, biological therapy, or radiotherapy from 4-6 months could affect the quality of life, recovery from cancer, or effectiveness of treatment protocol.
‘…The biological therapy is unavailable; even Al-Hayat hospital can’t secure the therapy to all patients…’ (Head-nurse, 51).
‘… We provided what was available of chemotherapy, but in case we don’t have, we transfer the patients…’ (oncologist, 46y)
‘… the radiotherapy is 100% unavailable, and transferring the patients is endless suffering, and most of the time the Israeli authorities reject the patients…’ (oncologist, 46y)
2. Affordability of care
Most interviewees claimed that poverty and life needs were much higher than their income. Despite the free of charge of care provided to cancer patients, the affordability of care was highlighted as an issue among the vast majority of the interviewed women. Many women claimed that they found hardship in securing the transportation fees (back and forth) while receiving the chemotherapy within the governmental hospital or during the treatment abroad outside Gaza. Other participants expressed their suffering in securing complementary therapies such as multivitamins, minerals, and food supplements.
It is essential to note the crucial role that non-governmental and community-based organizations play in securing most unmet needs and paying for some diagnostic tests. Most interviewees reported that cancer affected their economic situation as they could not work to ensure their living expenses. The deteriorating financial status highly exacerbates this in the Gaza Strip due to the siege imposed on Gaza for the last fifteen years, as one husband claimed.
‘After reeving the chemotherapy, I became exhausted and dizzy, so I took a taxi and paid around 30 NIS, and this was very costly’ (Female, housewife, 43y)
‘I can’t work at home now as I have weakness in my arm due to cancer…’ (Female, housewife, 47y)
‘My life has been affected as before cancer. I was able to work and bring what my family needed, but now I am unable to do so; I am physically weak’ (Female, housewife, 38y)
Most husbands suffered from financial hardship and expressed their inability to secure some basic needs for their wives and families. It is worth mentioning that husbands acknowledged the women’s health centre’s role in covering the costs of diagnostic tests and medications for all women who cannot pay.
‘… I paid 500 NIS to pass the long queue at the governmental hospital’ (Husband, jobless, 36y)
‘I can secure nothing for my wife’ (Husband, driver, 34y)
‘… the most supporter of my wife was the women’s health center…’ (Husband, carpenter, 39y)
Comparison of unmet needs with selected socio-demographic and clinical variables
summarizes the mean differences of selected socio-demographic and clinical variables with the SCNS-34 dimensions and as a whole. Generally, married women had more unmet needs than unmarried (t-test= 3.670, p < 0.001). The mean score of spousal women’s responses was higher in all the SCNS-34 dimensions except for physical and daily life needs, in which the mean was equal for both groups. However, significance was noticed in the health system and information.
Table 4. Association between supportive care needs and socio-demographic variables.
There was a significant relationship between unmet needs and breast surgical intervention (F = 4.161, p < 0.01). The significance was pro females who did not undergo breast surgery (partial or total mastectomy), as shown by the Bonferroni test. The importance was reported with psychological needs and the health system and information (F = 2.927, p < 0.05 and F = 10.045, p < 0.001, respectively)
A significant relationship was also noticed between the unmet needs of the SCNS-34 and the age of females (F = 9.599, p < 0.001). The mean score of the SCNS-34 dimensions was higher in the age group under 40 years. However, it was significant only with psychological, patient support and care and sexual needs (p < 0.01)
The mean score of unmet needs decreased with the increased duration of having breast cancer. Unmet needs were significant to newly discovered breast cancer females until three years from diagnosis (F = 3.987, p < 0.05). Specifically, the significance was noticed with the health system, information, and sexual needs (p < 0.05).
The presence of chronic diseases did not increase unmet needs. Overall, unmet need needs were significantly higher among females without chronic conditions (p < 0.05). The mean score of unmet needs of breast cancer females was higher in all the SCNS-34 dimensions except for psychological needs. However, significance was noticed with sexual and health system and information needs (p < 0.01).
Comparison of health-related quality of life with selected socio-demographic and clinical variables
As a whole, there was no significant relationship between unmarried and married women with quality of life (p > 0.05), similarly with the five dimensions of the EORTC-QOLQ-C15-Pal (p > 0.05).
The mean quality of life score, including all dimensions EORTC-QOLQ-C15-Pal except for fatigue, was higher for females who had not undergone breast surgery. However, no significant relationship was reported (p > 0.05).
HRQoL was seen to be better among the age group [Citation41–55]. The mean score was less in this group compared to other groups in all dimensions approximately (p < 0.05).
Overall, HRQoL worsened as the duration of breast cancer increased. However, it was not significant (p > 0.05). This was obvious in all the EORTC-QOLQ-C15-Pal dimensions except for the emotional part but also remained not substantial (p > 0.05)
Generally, HRQoL was affected by the presence of chronic diseases (p < 0.05); the mean score of HRQoL was higher in all the EORTC-QOLQ-C15-Pal dimensions. However, significance was observed with pain and physical function (p < 0.05) ().
Table 5. Association between HRQOL and socio-demographic variables.
Discussion
Accurate assessment of unmet supportive needs for females diagnosed with breast cancer is crucial for developing and initiating appropriate interventions to improve the QoL. If healthcare providers are aware of the specific unmet needs, they would effectively and efficiently communicate with their patients. Thus, patient satisfaction and QoL eventually improved. To the best of our knowledge, this is the first objective study to examine the supportive care needs (SCNs) and HRQOL of females with breast cancer in the Gaza strip/Palestine. This study provides actionable insights for policymakers and healthcare professionals regarding this topic.
The study shows that psychological and health-related information are the most prevalent unmet needs. The findings are consistent with comparative literature, which still show that psychological and information needs are the top priority and need, even in the long run, for females with breast cancer [Citation24]. A systematic review presented by Vivar and McQueen [Citation25] shows that breast cancer survivors continue to experience psychological needs first and then information needs. These needs are also proven by the qualitative study undertaken by Wells and his colleagues [Citation26]. Psychological needs are higher among survivor females less than two years. Literature suggests that addressing psychological needs would greatly influence supporting women in effective adjustment processes in the long run and improving their QoL [Citation27,Citation28]. It could be noticed that unmet needs for patients from western countries are highest in the psychological domain, whereas Asian patients’ needs are mostly related to health information. Lam and his colleagues explained the variation between countries as culture based, in which supportive care needs are products of perspectives of culture and integration of psychology [Citation29].
Interviewed women expressed concerns regarding psychological support as a central topic of discussion. Compared with the non-governmental hospital, Al-Motale’s hospital, in Al-Quds (Jerusalem), Gazan governmental hospitals generally do not provide psychological support. That can be interpreted by the high number of cancer patients observed daily in Gaza’s governmental hospitals. Therefore, healthcare providers cannot offer psychological support to their patients due to their workload. A significant concern in this regard is the shortage of specialised staff. Specialist psychologists can provide psychological consultations and various recreational activities with the involvement of doctors and nurses.
The need for health information is matched with previous studies [Citation30,Citation31]. Lack of knowledge regarding diet, treatment, side-effects, complications, physical activity, and re-assurance of treatment side-effects. Many patients receiving cancer treatment want information on how to get well, manage and control the disease, and manage side effects at home [Citation32]. There was a significant need for health education among most female patients in Gazan governmental hospitals. As a result of heavy workloads and time constraints, health workers need to provide complete and systematic health education to patients. Access to disease-related information can impact a patient’s self-confidence and self-efficacy in dealing with the disease and their motivation to understand how to combat it. As patients follow the progress of the disease, healthcare professionals should pay greater attention to providing adequate and effective health education support to them.
Interviewed women were supported with strength from family and colleagues to manage and overcome treatment steps and complications raised during treatment phases. Support and encouragement have taken many shapes, including, but not limited to, accompanying them to the hospital, helping with house activities, financial aid and regular home visits. These shapes of support and encouragement are also highlighted in the literature [Citation33,Citation34]. Previous literature indicates that patients highly value their family and friends support [Citation35]. Family involvement, especially the involvement of husbands and earlier patients with a similar disease with a specialised psychologist, can be beneficial in easing worries of a similar condition. Psychological care should be emphasised due to changes in female body image following chemotherapy and surgery. In line with previous studies, religious-based and spiritual support proved to be one of the most effective coping methods for cancer [Citation36,Citation37].
Most women emphasised physical function, pain, and fatigue as major concerns. These results are consistent with the literature assessing these symptoms [Citation38]. Pain and fatigue are associated with lower physical function. This is proven by our qualitative and quantitative studies and is in line with several studies. Patients with breast cancer reported lower physical, including physical performance Battery, longer chair stand times and lower handgrip strength [Citation39]. This is justifiable since females are exposed to various treatments, including chemotherapy and surgical interventions. Chemotherapy alone is known to have a specific devastating effect on the human body, including muscles and bones. Indeed, engagement in simple physical activities is found to have significant attribution in decreasing the intensity of pain and fatigue and improving sexual function [Citation40].
Sexual needs are the least reported, similar to Malaysia’s findings [Citation24]. Unlike our findings, sexual problems are common, with an estimated prevalence of up to 85% [Citation41,Citation42]. Our result could be justifiable since the topic ‘of sex’ is sensitive, and patients are reluctant to express their sexual feelings and needs. Moreover, further qualitative research, implemented by female interviewers, is recommended to explore the exact sexual needs. Treatment and management of symptoms are of greater importance to breast cancer patients than their sexual lives. However, as a result of the nature and specificity of the breast cancer treatments (e.g., chemotherapy, mastectomy, etc.), patients may also be concerned about the impact of the disease on their sexual lives, especially since they may lose hair and eyelashes, eyebrows, or perform a mastectomy, as well as how their husbands feel about these matters. As a result, they did behave differently and adjusted their lives accordingly. For instance, they wore a wig and changed their dressing style. This point is highlighted and deeply discussed [Citation33,Citation43].
Unmet needs were found to affect the HRQOL of females with breast cancer negatively. This finding confirms a Japanese [Citation44] and a Korean study [Citation45]. These results present the importance of determining the specific needs of females with breast cancer and initiating interventions to improve their QoL. Selecting the exact condition would reduce the chaos of service utilisation and healthcare system costs. Married women have more unmet needs in terms of their sexual needs and information needs than unmarried women.
Nevertheless, physical and daily life needs were equally met in both groups. There was a discrepancy between our findings and those of previous studies [Citation46]. These inconsistent results may result from limited samples, or unmarried women are more likely to have access to social resources and additional information channels due to time constraints and responsibilities. These findings require further rigorous investigation to verify. According to previous literature, support needs differ based on the patient’s age. The results of our study indicate that patients under the age of 40 require more care and support than older patients. Particularly for psychological, patient support and maintenance, and sexual needs.
According to this study, women who do not undergo breast surgery (partial or total mastectomy) have more significant psychological and informational needs than those who undergo surgery [Citation47]. Additionally, the unmet needs of newly diagnosed breast cancer women were higher until three years after diagnosis. The higher uncertainty of the disease patients encounter during the initial treatment may partly explain the higher anxiety about side effects. Moreover, Age-related differences can be explained largely by older patients’ emotional maturity, greater capacity to cope with breast cancer, and relative economic stability [Citation48]. The findings of this study agree with other studies, which report a more significant number of unmet SCNs in younger patients [Citation49]. Younger cancer patients may demand more body image and interpersonal relationship information.
QoL is noticed to be worse as the survival duration increases. We found QoL is better among females who had breast cancer less than three years. However, we did not look at QoL at the time of diagnosis. Fear, disbelief and a state of shock usually appear upon initial diagnosis, which might develop psychological crisis [Citation50]. These symptoms vary from woman to woman. However, one sign would interfere with females’ QoL, functioning, commitment, and treatment adherence. Considering females’ needs, particular interventions should be applied to improve their QoL in the long run.
Throughout the past few years, the Ministry of Health and the private sector have been unable to solve the shortage of chemotherapy, especially in Gaza. Further, the political conflict, the difficulty of obtaining chemotherapy in the West Bank facilities, and poor early detection may contribute to the low 5-year survival rate for Palestinian women with breast cancer. It is important to note that the absence of chemotherapy, biological therapy, or radiotherapy for 4–6 months can have a detrimental effect on the quality of life, recovery from cancer, or the effectiveness of the treatment protocol.
Most interviewees (women and husbands) suffer from financial constraints and are in poverty, and life needs outweigh their income. Although cancer patients are provided free care, the affordability of care has been identified as a concern by the vast majority of the women interviewed. Many expenses associated with life and treatment exceed their income; for example, transportation fees both within and outside Gaza and supplementation treatments such as multivitamins, minerals, and food supplements. Cancer affected the patient’s economic situation as they could not work to secure living expenses. These findings are highlighted and approved in the literature [Citation51,Citation52]. Due to the siege imposed on Gaza for the last fifteen years, the economic situation is deteriorating in the Gaza Strip. Community-based and non-governmental organisations are essential in securing most unmet needs and covering the cost of some diagnostic tests for women who can’t afford them. Indeed, these accessories are usually covered by the Women’s Health Center. Otherwise, women must pay the costs. There’s still a need for a synchronised system to bridge that need.
We found that comorbidities significantly worsen HRQOL because they negatively affect physical function and pain status. Wu, Davis, and Chen [Citation53] and Ameja and Brooks [Citation54] also support this finding. Following chemotherapy treatment for breast cancer and having at least one comorbid condition may be associated with worse physical and social functioning, increased discomfort, poorer sleep, and fatigue. The additional physical and mental strain may explain the results of our study that a breast cancer diagnosis places on women who already have other chronic disorders. The severity and complexity of chronic illnesses usually increase over time, decreasing a person’s functional status and, consequently, their quality of life and emotional health. The way that various chronic diseases manifest themselves and how they affect daily functioning can differ.
This research provides an insightful, valuable and rich description of the experiences and everyday unmet needs of females with breast cancer. The findings are added to the existing body of knowledge to shape the care of breast cancer females well and reduce potential gaps. Concerning the current health system in the Gaza strip, we see the partnership with non-governmental organisations as a jump-up solution to cover females’ needs and improve their satisfaction and prediction from the health care system.
The study’s main limitation is the sampling approach used to collect participants. However, this limitation was managed by a large sample size. The sample size was proportionally representing the five governorates of the Gaza strip. One slight limitation was the number of health workers recruited for interviews. Many healthcare workers were reluctant to participate, which the authors believed would make enough significant contributions to determining the unmet medical and health needs of females with breast cancer.
In conclusion, many needs are unmet. Caring for females with breast cancer should be comprehensive to fill gaps, including psychological care, health information and education, physical care and support, and medical care. Additionally, females who participated in interviews had no chronic diseases, and thus we could not explore unmet needs for those with chronic diseases (hypertension, diabetes mellitus, heart diseases…).
Consent for publication
Not applicable
Author contributions
AE, MR, and MA were responsible for the study design. SN and AM did data analysis. AE, MR, and SN interpreted the data. AE, MR, MA, AM and SN wrote the first draft equally. AE and MR did critically revise the first draft and made appropriate amendments. All authors agreed on the final manuscript.
Acknowledgement
The authors are grateful to women, their husbands, and healthcare workers who did not hesitate to participate in our study and make it real. We are grateful to the Health Information Unit - Ministry of Health, especially Mrs Haia Yaghi, for facilitating access to information regarding breast cancer. This study was extracted from a project submitted to and funded by the Qatar Red Crescent Society
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data are available with the corresponding author on request.
Additional information
Funding
References
- Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71(3):209–249.
- Francies FZ, Hull R, Khanyile R, et al. Breast cancer in low-middle income countries: abnormality in splicing and lack of targeted treatment options. Am J Cancer Res. 2020;10(5):1568–1591.
- Ghoncheh M, Pournamdar Z, Salehiniya H. Incidence and mortality and epidemiology of breast cancer in the world. Asian Pac J Cancer Prev. 2016;17(sup3):43–46.
- Iddrisu M, Aziato L, Ohene LA. Socioeconomic impact of breast cancer on young women in Ghana: a qualitative study. Nurs Open. 2021;8(1):29–38.
- Torre LA, Islami F, Siegel RL, et al. Global cancer in women: burden and trends. Cancer. Cancer Epidemiol Biomarkers Prev. 2017;26(4):444–457.
- Ministry of Health. 2020. Annual report 2019. Available at http://www.moh.gov.ps/portal/repyears/. (accessed on 20th March 2021).
- Snyder CF, Blackford AL, Brahmer JR, et al. Needs assessments can identify scores on HRQOL questionnaires that represent patient problems: an illustration with the supportive care needs survey and the QLQ-C30. Qual Life Res. 2010;19(6):837–845.
- Pongthavornkamol K, Lekdamrongkul P, Pinsuntorn P, et al. Physical symptoms, unmet needs, and quality of life in Thai cancer survivors after the completion of primary treatment. Asia-Pac J Oncol Nurs. 2019;6(4):363–371.
- Pachman DR, Barton DL, Swetz KM, et al. Troublesome symptoms in cancer survivors: fatigue, insomnia, neuropathy, and pain. J Clin Oncol. 2012;30(30):3687–3696.
- Zabora J, BrintzenhofeSzoc K, Curbow B, et al. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10(1):19–28.
- Mcillmurray MB, Thomas C, Francis B, et al. The psychosocial needs of cancer patients: findings from an observational study. Eur J Cancer Care. 2001;10(4):261–269.
- Wright AA, Keating NL, Balboni TA, et al. Place of death: correlations with quality of life of patients with cancer and predictors of bereaved caregivers’ mental health. J Clin Oncol. 2010;28(29):4457–4464.
- Clarke N, Mahler C, von Hagens C, et al. The effects of integrated supportive care intervention on quality of life outcomes in outpatients with breast and gynecologic cancer undergoing chemotherapy: results from a randomised controlled trial. Cancer Med. 2019;8(8):3666–3676.
- Haun MW, Estel S, Rücker G, et al. Early palliative care for adults with advanced cancer. Cochrane Database Syst Rev. 2017; 12;6(6: CD011129.
- Mirzaei F, Nourizadeh R, Hemmatzadeh S, et al. Supportive care needs in females with breast cancer under chemotherapy and radiotherapy and its predictors. Int J Women’s Health and Reprod Sci. 2019;7(3):366–371.
- Akechi T, Okuyama T, Endo C, et al. Patient’s perceived need and psychological distress and quality of life in ambulatory breast cancer patients in Japan. Psychooncology. 2011;20(5):497–505.
- Ham C, Jackson A, Peralta L, et al. Perceptions and experience of patients, staff, and clinicians with a social needs assessment. Perm J. 2018;22:18–105.
- Özbayır T, Geçkil ÖS, Aslan A. An adaptation of the short-form supportive care needs survey questionnaire (SCNS-SF 34) into Turkish. Eur J Breast Health. 2017;4;13(4):183–188.
- Abu-Odah H, Molassiotis A, Liu J. Challenges on providing palliative care for patients with cancer in low- and middle-income countries: a systematic review of reviews. BMC Palliat Care. 2020;19(1):55.
- Abu Hamad B, Skaik N, Abu-Odah H. Evaluation of palliative care services provided to cancer patients in the Gaza Strip. J US-China Med Sci. 2016;13(2016):95–107.
- Alawneh A, Yasin H, Khirfan G, et al. Psychometric properties of the Arabic version of EORTC QLQ-C15-PAL among cancer patients in Jordan. Support Care Cancer. 2016; 24(6):2455–2462.
- Boyes A, Girgis A, Lecathelinais C. Brief assessment of adult cancer patients’ perceived needs: development and validation of the 34-item supportive care need survey (SCNS-SF34). J. Eval. Clin. Pract. 2009;15(4):602–606.
- Braun V, Clark V. Using thematic analysis in psychology. Quality. Res. Psychol. 2006;3(2):77–101.
- Edib Z, Kumarasamy V, Binti Abdullah N, et al. Most prevalent unmet supportive care needs and quality of life of breast cancer patients in a tertiary hospital in Malaysia. Health Qual Life Outcomes. 2016;14(1):26.
- Vivar CG, McQueen A. Informational and emotional needs of long-term survivors of breast cancer. J Adv Nurs. 2005;51(5):520–528.
- Wells K. J, Drizin J. h, Ustjanauskas AE, et al. The psychosocial needs of underserved breast cancer survivors and perspectives of their clinicians and support providers. Support Care Cancer. 2022;30(1):105–116.
- Distelhorst SR, Cleary JF, Ganz PA, et al. Optimisation of the continuum of supportive and palliative care for patients with breast cancer in low-income and middle-income countries: executive summary of the breast health global initiative. Lancet Oncol. 2015;16(3):e137–47–e147. 2014
- Liao M-N, Chen S-C, Chen S-C, et al. Changes and predictors of unmet supportive care need in taiwanese women with newly diagnosed breast cancer. Oncology Nursing Forum. 2012;39(5):E380–E389.
- Lam WW, Au AH, Wong JH, et al. Unmet supportive care needs a cross-cultural comparison between Hong Kong Chinese and German Caucasian women with breast cancer. Breast Cancer Res Treat. 2011;130(2):531–541.
- Cheng KKF, Wong WH, Koh C. Unmet needs mediate the relationship between symptoms and quality of life in breast cancer survivors. Support Care Cancer. 2016;24(5):2025–2033.
- Meng Q, Yang Z, Wu Y, et al. Reliability analysis of the chinese version of the functional assessment of cancer therapy – Leukemia (FACT-Leu) scale based on multivariate generalizability theory. Health Qual Life Outcomes. 2017;15(1):93.
- Rutten LJ, Arora NK, Bakos AD, et al. Information needs and sources of information among cancer patients: a systematic review of research (1980–2003). Patient Educ Couns. 2005;57(3):250–261.
- Patel G, Harcourt D, Rumsey N, et al. Exploring the lived experience of breast cancer diagnosis and treatment amongst Gujarati-speaking Indian women. Divers Equal Health Care. 2015;12(1):9–17.
- Yoo GJ, Sudhakar A, Le MN, et al. Exploring coping strategies among young Asian American women breast cancer survivors. J Canc Educ. 2017;32(1):43–50.
- Leung J, Pachana NA, McLaughlin D. Social support and health-related quality of life in women with breast cancer: a longitudinal study. Psychooncology. 2014;23(9):1014–1020.
- Balboni TA, Vanderwerker LC, Block SD, et al. Religiousness and spiritual support among advanced cancer patients and associations with the end of life preferences and quality of life. J Clin Oncol. 2007;25(5):555–560.
- Hasson-Ohayon I, Braun M, Galinsky D, et al. Religiosity and hope: a path for women coping with a breast cancer diagnosis. Psychosomatics. 2009;50(5):525–533.
- Kurt B, Kapucu S. The effect of relaxation exercises on symptom severity in patients with breast cancer undergoing adjuvant chemotherapy: an open-label non-randomized controlled clinical trial. Eur. J. Integr. Med. 2018;22;54–61
- Winters-Stone KM, Medysky ME, Savin MA. Patient-reported and objectively measured physical function in older breast cancer survivors and cancer-free controls. J Geriatr Oncol. 2019;10(2):311–316.
- Shin W, Song S, Jung SY, et al. The association between physical activity and health-related quality of life among breast cancer survivors. Health Qual Life Outcomes. 2017;15(1):132.
- Chang YC, Chang SR, Chiu SC. Sexual problems of patients with breast cancer after treatment: a systematic review. Cancer Nurs. 2019;42(5):418–425.
- Gilbert E, Perz J, Ussher JM. Talking about sex with health professionals: the experience of people with cancer and their partners. Eur J Cancer Care. 2016;25(2):280–293.
- Koçan S, Gürsoy A. Body image of women with breast cancer after mastectomy: qualitative research. J Breast Health. 2016;12(4):145–150.
- Uchida M, Akechi T, Okuyama T, et al. Patients’ supportive care needs and psychological distress in advanced breast cancer patients in Japan. Jpn J Clin Oncol. 2011;41(4):530–536.
- Park BW, Hwang SY. Unmet needs of breast cancer patients relative to survival duration. Yonsei Med J. 2012;53(1):118–125.
- Rainbird K, Perkins J, Sanson-Fisher R, et al. The needs of patients with advanced, incurable cancer. Br J Cancer. 2009;101(5):759–764.
- Yu FF, Bai YN, He H, et al. Identifying the unmet supportive care needs, with concomitant influencing factors, in adult acute leukaemia patients in China. Eur J Oncol Nurs. 2017;30:67–74.
- Park BW, Lee S, Lee AR, et al. Quality of life differences between younger and older breast cancer patients. J Breast Cancer. 2011; 14(2):112–118.
- Li Q, Lin Y, Zhou H, et al. Supportive care needs and associated factors among Chinese cancer survivors: a cross-sectional study. Support Care Cancer. 2019;27(1):287–295.
- Paraskevi T. Quality of life outcomes in patients with breast cancer. Oncol Rev. 2012;6(1):e2.
- Dsouza SM, Vyas N, Narayanan P, et al. A qualitative study on experiences and needs of breast cancer survivors in Karnataka, India. Clin Epidemiol Glob Health. 2018;6(2):69–74.
- Norsa’adah B, Rahmah MA, Rampal KG, et al. Understanding barriers to Malaysian women with breast cancer seeking help. Asian Pac J Cancer Prev. 2012;13(8):3723–3730.
- Wu HS, Davis JE, Chen L. Impact of comorbidity on symptoms and quality of life among patients being treated for breast cancer. Cancer Nurs. 2019;42(5):381–387.
- Ameja J, Brooks JD. The impact of chronic comorbidities at the time of breast cancer diagnosis on quality of life, and emotional health following treatment in Canada. PLOS One. 2021;16(8):e0256536.