Abstract
Purpose
Axillary Web Syndrome (AWS) is a common sequela after surgical axillary lymph node dissection (ALND) often manifesting with reduced range of motion (ROM) of the limb, which requires rehabilitation. Notwithstanding, a standardized rehabilitation protocol is currently lacking in clinical practice. Our primary objective was therefore to evaluate the effectiveness of the use of a snapping manual maneuver (SMM, used in our clinical practice) to increase ROM during abduction (ABD) when compared with a standardized stretching exercise (SSE) protocol. A three-year follow-up of the enrolled patients was also carried out to determine the incidence of Breast Cancer-Related Lymphedema (BCRL).
Materials and methods
Between July 2013 and January 2019, we conducted a single-blinded randomized clinical trial. A total of 60 patients, who underwent ALND in our hospital, came to our clinic under medical advice or on voluntary access and reported AWS symptoms. The patients were randomly assigned into two equally divided groups. The treatment of group one consists in the execution of a supervised SSEs protocol, while group two additionally received a manual snapping maneuver. Patients of both groups received two treatment sessions within two weeks. At the end of the session, they were asked to continue the exercises autonomously on a daily basis, three times per day, for one month.
Results
There were no statically significant differences in ROM at our one-month follow-up and the incidence of BCRL was equally distributed after three years.
Conclusions
The use of the manual snapping maneuver in addition to stretching once per week for two weeks does not appear to improve the outcome of the patients in comparison with stretching alone and does not appear to be related to lymphedema in our 3 years follow-up.
Introduction
Axillary Web Syndrome (AWS) is a well-known sequela that arises after surgical treatment for breast cancer, with a reported incidence ranging from 6% to 75% [Citation1,Citation2]. This syndrome can affect shoulder mobility, thereby causing functional disability of the limb and may be defined as a thrombophlebitis of veno-lymphatic vessels caused by surgical trauma [Citation3]. In this context, lymph node removal procedures are the most frequently reported causes for the onset of this syndrome, with a lower incidence in sentinel lymph nodes biopsy (SLNB) and a much higher incidence in axillary lymph node dissection (ALND) [Citation1,Citation4].
Notably, the clinical features of AWS partially overlap with those of Mondor’s disease, which is reported in post-traumatic and surgical areas and is characterized by a large presence of veno-lymphatic capillaries (such as the inguinal region) [Citation5,Citation6]. AWS symptoms typically manifest within the first month after surgery, and its complete resolution occurs in 3–24 months [Citation1,Citation7]. The symptoms are frequently described as a sensation of pain and tension in the axillary region, at the elbow, forearm, and wrist, following the lymphatic path [Citation8]. Consequently, patients report a limited mobility of the arm and a reduction of their ability to perform activities that require a moderate amplitude of movement, always associated with the presence of a tendon-like cord [Citation9,Citation10].
It is widely accepted among physiotherapists that AWS requires rehabilitation assistance to prevent possible further complications, such as frozen shoulder or impingement syndrome, which could lead to a reduction of the quality of life of patients as well as to a significant increase in time and cost of treatment [Citation9,Citation11]. Physical therapy treatment consists of patient education, supervised and at-home exercises, and manual therapy including myofascial release, soft tissue mobilization, and cord manipulation and stretching to improve range of motion (ROM) and rapidly decrease pain.
Notwithstanding, a standardized rehabilitation protocol is currently missing in clinical practice [Citation12–21].
A manipulative treatment consisting of a fascial stretching can lead to the rupture of the cord associated with a ‘snap’-like sound, followed by a rapid restoration of pain-free functioning of the shoulder joint [Citation22–24]. In agreement with Elisabeth Josenhans [Citation22] and our clinical experience the use of a snapping manual maneuver (SMM) improves cord flexibility with an immediate reduction of the symptoms of AWS in patients. In this study, the primary aim is to determine the effectiveness of the technique in enhancing ROM with a focus on abduction (ABD) when compared with a standardized stretching exercise (SSE) protocol. It is known that AWS is not a risk factor for Breast Cancer-Related Lymphedema (BCRL) [Citation24], but a possible correlation between the use of a snapping maneuver and the onset of a late BCRL has not been investigated so far. For this reason, we assessed the treatment effect in reducing pain and disability and carried out a three-year follow-up of the enrolled patients in order to determine the incidence of BCRL, a chronic disease which, if not properly treated, can lead to a dramatic reduction of the quality of life of patients.
Material and methods
This single-blinded randomized clinical trial was carried out between July 2013 and January 2019 at the European Institute of Oncology (IEO).
All ALND patients who accessed our physiotherapy clinic under medical advice or by voluntary access were proposed to be part of this trial. Patients were subsequently assessed as eligible, enrolled, and randomized.
Inclusion criteria comprised axillary lymph nodes dissection for breast cancer with subsequent appearance of clinical symptoms of AWS, presence of palpable cord, pain and/or tension in axilla, and reduced ROM, which was assessed by physical examination, inspection, and palpation of the axilla and the arm.
Exclusion criteria applied during the enrollment phase were the following: absent written informed consent, co-existence of physical and psychological disorders with the potential to interfere with rehabilitation, previous axillary dissection or neck lymph node dissection, previous breast reconstruction with flaps or with an expander, bilateral ALND, and diagnosis of primary lymphedema with ongoing AWS treatment.
The enrolled patients were randomly assigned to two treatment groups. Patients of both groups underwent one treatment session per week for two weeks with pre- and post-assessment at each session. After each session, patients were asked to continue the exercises autonomously on a daily basis, three times per day, for one month. A first follow-up examination was scheduled one month after the first session. A second reevaluation was performed three years later.
Exercise protocol consisted of stretching exercise for shoulder ABD and flexion on both supine and standing position. Each exercise had to be repeated for five times and the stretching position had to be maintained for 30 s. Patients were instructed to reach the maximum ROM they could.
Group of standardized stretching exercise (SSE)
During the first and second session, patients in this group followed a SSEs protocol for the upper limb with the assistance of the therapist. [Citation25]
Group of snapping manual maneuver (SMM)
Patients in this group were administered a manual therapy technique in addition to the SSEs protocol already described for SSE group. The manual therapy technique consisted of a snapping maneuver of fibrotic adhesion in the armpit, medial arm, and forearm. This technique is performed with the patient in the supine position with both legs extended. The patient is then asked to reach the maximum point of flexion she can achieve with the affected arm, so that the therapist can place his or her fingers at the extremity of the AWS cord. One hand is placed in the axilla region and the other hand at the elbow or at forearm or wrist. A light perpendicular pressure is applied and combined with a longitudinal traction. If the cord does not snap and break after the first try, the therapist repeats the maneuver for a maximum of six times in the shoulder flexion position, and six additional times in the ABD position. In case of persistence of cording after these 12 repetitions of the maneuver, patients were instructed to continue the stretching exercises.
Assessments and blinding
All recruitments and treatments were performed by the same therapist (SF).
All assessments were performed by two therapists blinded to group allocation throughout the study.
The first measurement and data collection were performed before randomization. Subsequently, patients are informed in which group they will be assigned. ROM and pain were assessed before and after the treatments and during the first follow-up examination (NTLF). The presence or absence of lymphedema was evaluated at the third year (GM). Also, the statistician (GS) performed the dataset analysis in a blinded form.
Shoulder ROM
Patients were evaluated in supine position by using a universal full-circle digital goniometer (Jamar, Anaheim, CA). Flexion, extension, ABD, and medial and lateral rotation of the shoulder were measured till the maximum pain tolerated and without compensation done by patients. No passive support was given to the arm [Citation26].
Pain NRS-11 scale
Using the numerical unidimensional scale as a number between 0 and 10 NRS-11 scale, patients were asked to verbally indicate the pain intensity during the maximal arm ABD in the assessment, 0 corresponding to no pain and 10 to the worst possible pain [Citation27].
Lymphedema evaluation
Circumferential measurement was performed with the patient in the supine position with both arms relaxed and extended. The therapist measured the patient’s arm every four centimeters starting from the ulnar styloid using a tape measure. The presence of lymphedema was confirmed if the difference between the two arms in at least one point was equal to or greater than two centimeters [Citation28].
In addition to circumferential measurements, the therapist used a Moistmeter-D® (Delfin Technologies, Kuopio, Finland) to evaluate the percentage of water under the skin. Five measurement points per arm were chosen: the area of the first dorsal interosseous muscle, two points on the medial part of forearm at 8 and 16 centimeters from the ulnar styloid, and two points on the medial part of the arm at 8 and 16 cm above the medial epicondyle. Lymphedema presence was confirmed if the ratio difference between the two arms in at least one point was higher than 1.26 [Citation29–31].
Subclinical stage of lymphedema was defined as a positive TDC measurement in the presence of a negative circumferential measurement.
Randomization
After enrollment in the study, randomization was performed through the ‘web-based’ TENALEA system [Citation32] and assigned in a ratio 1:1 to one of the two arms, intervention group (SMM) and control group (SSE), using concealed envelope. A progressive identification number was assigned to each subject, and at randomization a link between the subject’s identification number and the arm was established by a third part subject blinded to the randomization procedure.
Statistical analysis
Statistical analysis was performed on an intention-to-treat basis. The statistician was given coded data and thus was blinded to the treatment groups. Categorical variables were reported as frequencies (percentages), whereas continuous variables were summarized with median and interquartile range (25th–75th percentiles). Differences between arms of categorical variables were evaluated with Chi-squared tests whereas Wilcoxon-rank test was employed for continuous variables.
The trend over time of changes from baseline of continuous variables was investigated considering the random effects model for repeated measures. In order to take into account correlation within patients, we applied the repeated measurement analysis. Time effect was included in the model as fixed factor. Residuals from full models were checked to assess normal distribution.
The main outcome is the change in ABD from baseline (T0) to the end of the first treatment (T1). Patients were subsequently evaluated after one week (both before (T2) and after the second treatment (T3)) and after one month (T4). The sample size calculation was obtained to test the hypothesis that the SMM intervention can improve ABD compared to the SSE group. The expected difference in improvement in ABD between study arms ranged from 50 degrees, on average, to 70 degrees, with an estimated standard deviation of around 25 degrees. A sample size of 28 patients per arm reaching 80% of power, to test this hypothesis, considering a Student-T test and Alfa equal to 0.05. The statistical analyses were performed using SAS software version 9.2 (SAS Institute Inc., Cary, NC).
Results
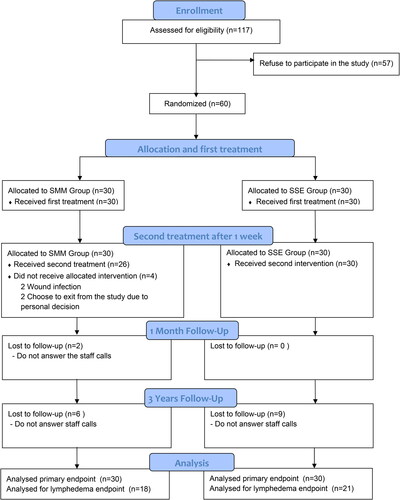
A total of 60 patients were enrolled between June 2013 and December 2015. The enrolled patients were randomized into two groups, comparable in terms of demographic composition and clinical features ().
Table 1. Patients’ general data.
Among the initial population of the study, unfortunately, nine patients of SSE group were lost at the three-year follow up. Conversely, as far as SSM is concerned, two patients experienced wound infection and 2 more decided to interrupt their participation before the second treatment session due to personal matters. Two additional patients dropped out at the one-month follow-up because they did not answer staff calls, whereas six patients were lost at the three-year follow up ().
Regarding our primary outcome (ROM in ABD), after the first treatment, SMM patients displayed a slightly lower ABD gain in comparison to SSE patients, with an average gain of 48° and 56°, respectively. Conversely, after the second treatment, SMM patients had an average gain of 32.5° versus the 22° of the SSE group. Between the first and the second treatment, we observed a reduction of ROM values of 15.5° for the SMM group and 19° for the SSE group.
After one month, both groups had recovered the complete ROM ( and ).
Figure 2. Change in arm abduction ROM. ROM: range of motion; SMM: snapping manual maneuver; SSE standardized stretching exercise; T0-Baseline: First evaluation; T1: Evaluation after first treatment; T2: Evaluation before second treatment; T3: Evaluation after second treatment; T4: Evaluation 1-month follow up.
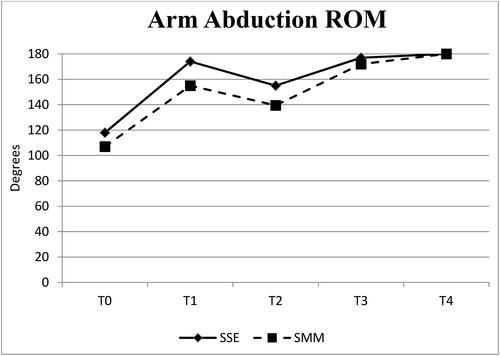
Table 2. Range of motion.
As far as pain was concerned, we observed a reduction of 2 points immediately after the treatment session. After the first session, the values decreased from 7.9 to 5.7 in the SMM group and from 7.3 to 5.3 in the SSE group. After the second session, the values reduced from 6.1 to 3.9 in the SMM group and from 6.2 to 3.9 in the SSE group. The pain further decreased to 2.1 at the one-month follow-up for both groups ().
Table 3. Pain measurement.
Both ROM in ABD and pain outcome showed no significant differences between the groups in all points assessed over time (p = 0.82, ) (p = 0.67, ).
At three years of follow up, 13% of patients presented with BCRL and 21% with subclinical BCRL. Notably, the BCRL was equally distributed in both groups without significant differences (p = 0.51, ).
Table 4. Patients’ follow-up.
Discussion
The rational of our study was the need of evidence regarding safety and effectiveness for the AWS treatment, as this syndrome is still approached without a wide consensus by the therapists. Since the first description by Moskovitz et al. [Citation1], numerous studies have been conducted to define the time of onset, the most appropriate diagnostic methods, and the pathophysiology of AWS.
Although many studies have underlined the importance of starting physiotherapy as early as possible once AWS has been diagnosed, there is still no identifiable most effective treatment, nor are there other studies that assess the efficacy of a rehabilitation protocol [Citation7–9,Citation12–21]. Our study aimed to test the manual treatment protocol compared with the established and SSEs used for treatment of AWS.
As extensively described by many authors, one of the main symptoms of AWS is the reduction of shoulder ROM, especially during ABD [Citation1,Citation9,Citation10]. Accordingly, patients enrolled in this study also presented with a reduction of shoulder ROM, as confirmed by the values measured at the beginning of the treatment. We observed an immediate improvement, not statistically significant, after the first and second treatment for both groups. However, ROM values measured one month after the first treatment appeared to be very similar between the two groups, pointing to the possibility that the two management protocols might have the same efficacy over a longer time period. A reduction of ROM values was subsequently reported in both groups between the first and the second treatment sessions. The possibility that the treatment undertaken at home was insufficient or not performed correctly, as well as the influence of still-ongoing AWS pathophysiological processes, might account for the reduced mobility observed in the patients between the two sessions. However, all patients displayed a complete recovery of the shoulder ROM at the one-month follow-up. This may well be due to the home exercises.
End range pain in the shoulder movement appears to be another symptom caused by AWS [Citation1,Citation33]. Indeed, pain reduction is intimately linked to the resolution of the syndrome. The SMM treatment did not lead to increased pain over time, but it could sometimes be perceived as painful when performed. The sensation of pain experienced by patients during the maneuver has not been evaluated due to its short duration. Reduction of pain occurred in both groups with similar trends, allowing greater mobility of the affected upper limb. Despite patients fully recovered shoulder ROM at the one-month follow-up, 50% of subjects still presented AWS intended as the presence of palpable cords, suggesting that shoulder’s ROM recovery, and AWS resolution each follow its own path. Importantly, after one month, a periodic follow-up aimed at assessing the AWS resolution in both groups was not performed in this study, but the three years follow-up did confirm that all patients had a complete regression of the syndrome without any presence of palpable cord.
Patients were subsequently reexamined three years after initial enrollment in order to evaluate the incidence of lymphedema in both groups, although previous studies had already ruled out that AWS and its management could be a risk factor for lymphedema [Citation24]. Accordingly, the results obtained in our study appear to be in line with the literature [Citation18,Citation34], with no clinical and statistically significant differences between the two treatment groups. We therefore concluded that the additional SMM treatment does not increase the incidence of lymphedema. Notably, the incidence of lymphedema increases when taking into account the data obtained with the TDC method, a method that allows detection of subclinical lymphedema in the absence of clinical manifestations and could represent an additional assessment tool in the surveillance of BCRL overtime.
Our study is one of the first randomized clinical trial to assess the efficacy of an established protocol in this syndrome, and is characterized by certain limitations. The major limitation is linked to patients’ dropout. A total of six patients of the SSE group could not be evaluated at the one-month follow-up and we have no information regarding the personal reasons of two patients who decided to interrupt the study. The more substantial loss occurred at our three-year follow-up, in which a total of 21 patients were lost. As this last follow-up was necessary to assess the incidence of lymphedema, the patients needed to be evaluated in our hospital. Since some of them lived outside the region in which our hospital is located (Lombardy), we were unable to perform this second end point evaluation in these patients. Nevertheless, our data is consistent with the published literature regarding the incidence of lymphedema after AWS treatment [Citation18,Citation24].
Another limitation arises from the lack of verification that the exercises were correctly performed at home by the patients. As there is no valid instrument to assess compliance with our protocol, the data presented here were collected in good faith, under the assumption that all the patients complied correctly with the proposed program. Nevertheless, our research and the results are still relevant, especially in terms of assisting other institutions and physiotherapists how to address treatment options in these populations. Furthermore, our study could be used as a reference for other studies aimed at comparing our protocol with new ones or at studying its efficacy in other patients’ populations, such as those presenting AWS or undergoing BLS or ALND surgery for sarcoma or melanoma.
In conclusion, the addition of the manual snapping maneuver to the rehabilitation protocol might improve shoulder mobility. However, no statistically significant difference was observed in comparison to the stretching exercise protocol. Based on our limited data, this maneuver does not appear to be related to lymphedema. Further studies are still warranted to compare the effectiveness of our protocol with other treatment methods.
Author contribution
FS, LFNT, MCS, and AL contributed to the study conception and design. Recruitment was performed by FS. Data collection were performed by LFNT, MG. Data analysis and interpretation were performed by SG. All the authors made the critical revision of the article and gave the final approval of the version to be published.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the European Institute of Oncology Ethics Committee approved this study (IEO712/412).
Consent to participate
All participants gave written informed consent before data collection began.
Consent for publication
Written informed consent was obtained from all participants included in the study.
Acknowledgments
We would like to thank Dr. Tapani Lahtinen and Delfin Technologies for having us supplied with Moistmeter-D® device, Ilaria Parenti for her constructive comments and William Russell-Edu for revising the English of this manuscript.
Disclosure statement
The authors report no conflict of interest.
Data availability statement
The data that support the findings of this study are available from the corresponding author, F.S, upon reasonable request.
Additional information
Funding
References
- Moskovitz AH, Anderson BO, Yeung RS, et al. Axillary web syndrome after axillary dissection. Am J Surg. 2001;181(5):434–439.
- Koehler LA, Hunter DW, Blaes AH, et al. Function, shoulder motion, pain, and lymphedema in breast cancer with and without axillary web syndrome: an 18-month follow-up. Phys Ther. 2018;98:518–527.
- Rashtak S, Gamble GL, Gibson LE, et al. From furuncle to axillary web syndrome: shedding light on histopathology and pathogenesis. Dermatology. 2012;224(2):110–114. doi: 10.1159/000337210.
- Leidenius M, Leppänen E, Krogerus L, et al. Motion restriction and axillary web syndrome after sentinel node biopsy and axillary clearance in breast cancer. Am J Surg. 2003;185(2):127–130. doi: 10.1016/s0002-9610(02)01214-x.
- Craythorne E, Benton E, Macfarlane S. Axillary web syndrome or cording, a variant of mondor disease, following axillary surgery. Arch Dermatol. 2009;145(10):1199–1200. doi: 10.1001/archdermatol.2009.239.
- Pappo I, Wasserman I, Stahl-Kent V, et al. Mondor’s disease of the axilla: a rare complication of sentinel node biopsy. Breast J. 2004;10:253–255.
- O’Toole J, Miller CL, Specht MC, et al. Cording following treatment for breast cancer. Breast Cancer Res Treat. 2013;140(1):105–111. doi: 10.1007/s10549-013-2616-9.
- Leduc O, Sichere M, Moreau A, et al. Axillary web syndrome: nature and localization. Lymphology. 2009;42(4):176–181.
- Torres Lacomba M, Mayoral Del Moral O, Coperias Zazo JL, et al. Axillary web syndrome after axillary dissection in breast cancer: a prospective study. Breast Cancer Res Treat. 2009;117(3):625–630. doi: 10.1007/s10549-009-0371-8.
- Bergmann A, Mendes VV, de Almeida Dias R, et al. Incidence and risk factors for axillary web syndrome after breast cancer surgery. Breast Cancer Res Treat. 2012;131(3):987–992. doi: 10.1007/s10549-011-1805-7.
- Cheville AL, Tchou J. Barriers to rehabilitation following surgery for primary breast cancer. J Surg Oncol. 2007;95(5):409–418. doi: 10.1002/jso.20782.
- Fourie WJ, Robb KA. Physiotherapy management of axillary web syndrome following breast cancer treatment: discussing the use of soft tissue techniques. Physiotherapy. 2009;95(4):314–320. doi: 10.1016/j.physio.2009.05.001.
- Thomas-MacLean R, Tilley A, Thomas MR. Continuing medical education formation médicale continue lymphatic cording or axillary web syndrome after breast cancer surgery. Can J Surg. 2009;52(4):E105–E106.
- Reedijk M, Boerner S, Ghazarian D, et al. A case of axillary web syndrome with subcutaneous nodules following axillary surgery. Breast. 2006;15:411–413.
- Box RC, Reul-Hirche HM, Bullock-Saxton JE, et al. Shoulder movement after breast cancer surgery: results of a randomised controlled study of postoperative physiotherapy. Breast Cancer Res Treat. 2002;75(1):35–50. doi: 10.1023/a:1016571204924.
- Hase K, Kamisako M, Fujiwara T, et al. The effect of zaltoprofen on physiotherapy for limited shoulder movement in breast cancer patients: a single-blinded before-after trial. Arch Phys Med Rehabil. 2006;87(12):1618–1622. doi: 10.1016/j.apmr.2006.08.339.
- Lauridsen MC, Christiansen P, Hessov I. The effect of physiotherapy on shoulder function in patients surgically treated for breast cancer: a randomized study. Acta Oncol. 2005;44:449–457.
- Pereira R, Koifman ACP, Bergmann RJ. A. Incidence and risk factors of lymphedema after breast cancer treatment: 10 years of follow-up. Breast. 2017;36:67–73.
- Koehler LA, Haddad TC, Hunter DW, et al. Axillary web syndrome following breast cancer surgery: symptoms, complications, and management strategies. Breast Cancer (Dove Med Press). 2019;11:13–19. doi: 10.2147/BCTT.S146635.
- Cho Y, Do J, Jung S, et al. Effects of a physical therapy program combined with manual lymphatic drainage on shoulder function, quality of life, lymphedema incidence, and pain in breast cancer patients with axillary web syndrome following axillary dissection. Support Care Cancer. 2016;24(5):2047–2057. doi: 10.1007/s00520-015-3005-1.
- Agostini F, Attanasi C, Bernetti A, et al. Web axillary pain syndrome—literature evidence and novel rehabilitative suggestions: a narrative review. Int J Environ Res Public Health. 2021;18(19):10383. doi: 10.3390/ijerph181910383.
- Elisabeth J. Physiotherapeutic treatment for axillary cord formation following breast cancer surgery. Pt_Zeitschrif Physiother. 2007;59:868–878.
- Kepics JM. Physical therapy treatment of axillary web syndrome. Rehabil Oncol. 2004;22(1):21–22. doi: 10.1097/01893697-200422010-00010.
- Wariss BR, Costa RM, Pereira ACPR, et al. Axillary web syndrome is not a risk factor for lymphoedema after 10 years of follow-up. Support Care Cancer. 2017;25(2):465–470. doi: 10.1007/s00520-016-3424-7.
- Riabilitazione motoria dopo intervento di dissezione ascellare. 2013. [Internet]. [cited 2023 Apr 14]. Available from: https://www.ieo.it/Documents/Materiale%20infoeducativo/Riabilitazione%20motoria%20dopo%20Dissezione%20Ascllare%20(FIS.DO.4073).pdf
- Norkin CC. Measurement of joint motion: a guide to goniometry. 5th ed. Physiotherapy Canada. Philadelphia (PA): F.A. Davis; 2016.
- Farrar JT, Young JP, LaMoreaux L, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. doi: 10.1016/S0304-3959(01)00349-9.
- Armer JM, Stewart BR. A comparison of four diagnostic criteria for lymphedema in a post-breast cancer population. Lymphat Res Biol. 2005;3:208–217.
- Mayrovitz HN. Assessing local tissue edema in postmastectomy lymphedema. Lymphology. 2007;40(2):87–94.
- Mayrovitz HN. Assessing lymphedema by tissue indentation force and local tissue water. Lymphology. 2009;42:88–98.
- Mayrovitz HN, Weingrad DN, Davey S. Local tissue water in at-risk and contralateral forearms of women with and without breast cancer treatment-related lymphedema. Lymphat Res Biol. 2009;7:153–158.
- AleaClinical [Internet]. [cited 2023 Apr 14]. Available from: https://www.aleaclinical.eu/our-services/
- Alves Nogueira Fabro E, Bergmann A, do Amaral e Silva B, et al. Post-mastectomy pain syndrome: incidence and risks. Breast. 2012;21:321–325.
- DiSipio T, Rye S, Newman B, et al. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013;14(6):500–515. doi: 10.1016/S1470-2045(13)70076-7.