?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background: A substantial proportion of patients with type 2 diabetes mellitus (T2DM) do not reach their target HbA1c level on metformin. The objective of this retrospective observational cohort study is to better characterize the distance between HbA1c target and patient’s actual HbA1c level (the distance to goal), using a target HbA1c of 7.0% (53 mmol/mol), in patients with T2DM who have started metformin monotherapy.
Methods: We used data from the GE Centricity Electronic Medical Record database by IQVIA in 2016 in the United States (US) to identify adults with T2DM who started metformin monotherapy (MM) and received at least 90 days of treatment. Patients were categorized into three groups: those who achieved the goal of HbA1c <7.0%, those who did not achieve the goal of HbA1c <7.0% (i.e. failed MM) and received intensified treatment, and those who failed MM and did not receive intensified treatment. Distance to goal was computed for patients in each group.
Results: We identified 20,704 patients in the US database who started MM; 1741 (8.4%) failed MM and received intensified treatment, while 4977 (24.0%) failed MM and did not receive intensified treatment. The mean post-MM HbA1c for those who failed MM and received intensified treatment was 8.7% (72 mmol/mol) (median 8.2%, 66 mmol/mol) and the mean distance to goal was 1.7% (median 1.2%). The mean post-MM HbA1c for those who failed MM and did not receive intensified treatment was 8.0% (64 mmol/mol) (median 7.5%, 58 mmol/mol) and the mean distance to goal was 1.0% (median 0.5%).
Conclusion: A proportion of US T2DM patients do not achieve glycemic control (target HbA1c < 7.0%) despite 90 days of MM. Patients who failed MM and eventually received intensified treatment did so when their HbA1c distance to goal exceeded the level at which one add-on therapy alone might be sufficient to bring them to goal.
Introduction
Type 2 diabetes mellitus (T2DM) is the result of a progressive loss of insulin secretion, which often occurs in addition to existing insulin resistance and can lead to elevated glycated hemoglobin (HbA1c) levels (i.e. hyperglycemia)Citation1. Diabetes treatment, therefore, is directed towards preventing and controlling hyperglycemia, i.e. achieving glycemic control, along with managing the microvascular and macrovascular complications associated with the diseaseCitation2. These complications, which result from prolonged hyperglycemia, represent the main source of morbidity and mortality in patients with T2DMCitation2,Citation3. Randomized controlled trials have established that close glycemic control can reduce the risk of microvascular complications such as neuropathy, retinopathy, and nephropathyCitation4–7. To achieve and maintain optimal glycemic control, prompt treatment intensification is recommended for patients who do not achieve their glycemic goalsCitation8 and consistent monitoring is necessary to evaluate changes in glycemic control over timeCitation3.
Unless contraindicated or not tolerated, metformin monotherapy (MM), along with lifestyle modifications, such as diet and exercise, is the preferred treatment for patients newly diagnosed with T2DM due to its low risk of hypoglycemia and lasting antihyperglycemic effectCitation8,Citation9. The addition of a second antihyperglycemic agent (AHA) is recommended and selected based on patient and drug characteristics, for patients who fail to achieve glycemic control within three monthsCitation8,Citation9.
A target of HbA1c less than 7.0% (53 mmol/mol), which has been observed to reduce the risks for diabetic complications, is recommended by the American Diabetes Association (ADA) for most nonpregnant adultsCitation3,Citation5,Citation10,Citation11. The ADA and the European Association for the Study of Diabetes (EASD) further recommend that individual targets for HbA1c be established based on patient needs, health status, age, and adverse effects of treatmentCitation3,Citation12. A more aggressive glycemic target of HbA1c < 6.5% may be appropriate for individuals with T2DM who are able to attain glycemic control through lifestyle modifications and metformin alone or those with long life-expectanciesCitation3. Alternatively, a less strict target of HbA1c < 8.0% has been suggested for patients with a history of severe hypoglycemia, short life expectancy, established microvascular or macrovascular complications, significant comorbid conditions, or difficult to manage diabetes. However, despite recommendations published by the ADA and EASD for glycemic control in T2DM and the availability and use of metformin, no more than roughly 50% of patients with diabetes achieve HbA1c < 7.0%Citation13–16.
Treatment intensification in patients with T2DM who have poor glycemic control is often delayed; this phenomenon is known as “clinical inertia.”Citation15 Clinical inertia in T2DM, which exists in over 50% of patients with T2DMCitation17–19 and which negatively impacts glycemic controlCitation20–23, has been defined as the failure by healthcare providers to initiate or intensify treatment when the glycemic targets have not been met. The delay associated with clinical inertia can extend one to three years. For example, Khunti et al. found delays of 2.9, 1.9, and 1.6 years before treatment intensification in UK patients with HbA1c levels of ≥7.0%, ≥7.5%, and ≥8.0%, respectivelyCitation14 and Fu et al. reported that the median time to treatment intensification was 14.0 months for US patients who failed metformin monotherapy after six months of treatment and 19.0, 8.7 and 4.5 months for patients with HbA1c levels of 7.0 to < 8.0%, 8.0% to < 9.0% and ≥9.0%, respectivelyCitation24.
Despite the plethora of published data on the prevalence of suboptimal glycemic control (i.e. HbA1c < 7.0%), the HbA1c level and distance to goal at which providers intensify patients’ treatment regimens, by adding a second AHA, has not been well characterized. The primary objective of this study is to quantify the distance to the target goal of HbA1c < 7.0% after MM for patients who did not achieve that HbA1c target (i.e. who failed MM after 90 days of treatment). The secondary objective is to describe the characteristics of patients who (1) achieved glycemic control; (2) who failed MM and received intensified treatment; and (3) who failed MM and did not receive intensified treatment.
Methods
Data source, study design, and study sample selection
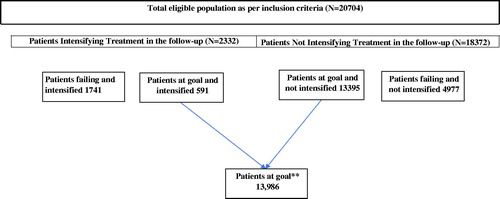
Following a retrospective cohort study design (), patient-level data from the GE Centricity Electronic Medical Record (EMR) database by IQVIA in the United States (US) were used to identify adults (≥18 years old) with T2DM who started metformin monotherapy in 2016 and received at least 90 days of treatment. The GE Centricity EMR database contains information longitudinally collected from over 30,000, mostly primary care, healthcare providers across 49 states in the US. In addition to demographic data such as age, sex, and race/ethnicity, the database also contains information on the use of healthcare services, physician visits, diagnostic tests, and drug prescriptions that patients receivedCitation25,Citation26.
T2DM was identified using the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes (Appendix 1).
Members of our analytic cohort were also required to have been continuously enrolled in the database for 12 months prior to the index date, defined as the first prescription for metformin, and have at least one HbA1c measure during the follow-up period, which started 90 days after the index date and ended 365 days after the index date. Diabetes diagnosis codes must have been present from 12 months before to six months after the index date. Patients who used any AHA, including metformin or insulin, during the 12-month pre-index period were excluded, as were patients who were pregnant or who had any evidence of a diagnosis of type 1, gestational, or other forms of diabetes mellitus during the pre-index period. We categorized patients into three analytic groups: those who achieved the goal of HbA1c < 7.0%, those who failed MM and received intensified treatment, and those who failed MM and did not receive intensified treatment. Treatment intensification was defined as the addition of another oral or injectable AHA.
Study measures
Post-Metformin monotherapy HbA1c and distance to HbA1c goal
The primary outcome of interest was distance to HbA1c goal, which was calculated for patients who failed MM. Distance to goal, measured in percentage points, is calculated as mean and median difference from HbA1c of 7% (53 mmol/mol). Patient’s post-MM HbA1c level corresponds to the HbA1c level measured within 6-months of the treatment intensification for those patients who added another AHA to their MM regimen or the HbA1c measured between 90 and 365 days after the index date for those patients who did not add another AHA to their MM regimen.
Demographic and clinical characteristics
Baseline clinical and characteristics of patients included age, sex, body mass index (BMI; ), baseline HbA1c (defined as the most recent HbA1c measure within 6 months prior to index date), presence of microvascular or macrovascular complications, history of severe or recurrent (>once per year) hypoglycemic events, history of smoking, and history of alcohol consumption. The definitions of the comorbid conditions, which appear in , are available in Appendix 1. Age and sex were assessed on the index date; the other characteristics were assessed during the baseline period (i.e. during the 12-month pre-index period).
Table 1. Demographic and clinical characteristics of the GE centricity electronic medical record cohort, United States (N = 20,704).
In addition, days of metformin between the index date and the date a patient received intensified treatment or the end of follow-up (365 days after the index date) for those who did not intensify was assessed.
Statistical analyses
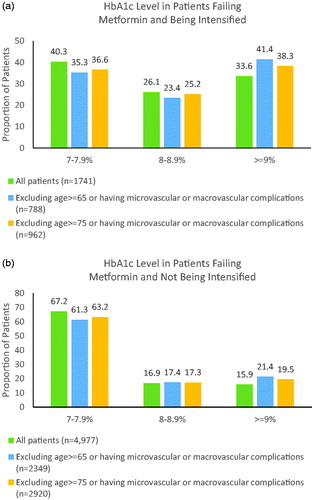
Continuous measures were summarized by their means, standard deviations, medians, minimum values, and maximum values; categorical variables were described as proportions. Baseline characteristics were stratified by analytic group; post-MM HbA1c and distance to goal were stratified by treatment intensification status. Because HbA1c targets >7.0% may be more appropriate for older patients or those with diabetes-related complications, we performed two sensitivity analyses in which we recomputed post-MM HbA1c: (1) distance to goal was computed for patients who were younger than 65 and who also did not have a history of microvascular or macrovascular complications or severe or recurrent hypoglycemia during the baseline period; (2) distance to goal was computed for patients who were younger than 75 and who also did not have a history of microvascular or macrovascular complications or severe or recurrent hypoglycemia during the baseline period.
Results
We identified 20,704 patients in the GE Centricity EMR database with T2DM who started MM. Most patients (67.6%) achieved HbA1c < 7.0%, while approximately one-third (32.4%) failed MM. The patients’ baseline clinical and demographic characteristics are shown in . Those who achieved HbA1c < 7.0% were slightly older, were more likely to be female and white, and had lower baseline HbA1c values than patients who failed MM. Patients who failed MM and received intensified treatment were slightly younger, more likely to be white, had higher baseline HbA1c and were more likely to have had microvascular complications than patients who failed MM and did not receive intensified treatment.
displays the data on post-MM HbA1c levels and distance to goal for patients failed MM. By the time patients intensified their treatment, their mean HbA1c level was 8.7% (72 mmol/mol) (median, 8.2%, 66 mmol/mol)) and their mean distance to goal was, therefore, 1.7% (median, 1.2%), with median days to intensification of 181 days (IQR 126, 262). The mean post-MM HbA1c level for patients who did not receive intensified treatment was 8.0% (64 mmol/mol) (median, 7.5%, 58 mmol/mol)) and their mean distance to goal was, therefore, 1.0% (median, 0.5%). Overall, for patients failing metformin, 27.8% of patients were ≥1.5% away from the glycemic target. After exclusion of patients ≥65 years or with history of severe hypoglycemia or microvascular or macrovascular complications, 33.8% of patients failing were ≥1.5% away from the glycemic target. After exclusion of patients ≥75 years or with history of severe hypoglycemia or microvascular or macrovascular complications, 31.7% of patients failing were ≥1.5% away from the glycemic target from the glycemic target. Compared to patients who failed MM and received intensification, 26.1% and 33.6% had HbA1c 8.0–8.9% and ≥9.0%, respectively, compared with 16.9% and 15.9% for those who failed MM and did receive intensified treatment ().
Table 2. Distance to glycemic goal of HbA1c < 7.0% in patients who failed metformin monotherapy, GE centricity electronic medical record cohort, United States (N = 3718).
Discussion
This study contributes to the literature on T2DM treatment patterns and on T2DM treatment intensification by quantifying post-MM HbA1c and distance to goal for patients who failed MM. We found that 32.4% of US patients initiating MM failed therapy within one year of initiation, 8.4% failed MM and received intensified treatment, while 24.0% failed MM and did not receive intensified treatment. A substantial proportion of patients (33.6%) who failed MM and received intensified treatment did so when their HbA1c levels were 9.0% (75 mmol/mol) or higher. The mean post-MM distance to goal when patients received intensified treatment was 1.7% in the US, which exceeded the recent ADA’s distance to goal threshold for starting combination therapy of 1.5%Citation27. Our results resemble those of the few studies that have reported distance to goal. For example, Mata-Cases et al. reported a mean distance to HbA1c < 7.0% of 1.4% using a primary care-based sample of Spanish patients managed with a variety of regimens from lifestyle modification alone to multiple AHACitation28. Khunti et al. reported a mean distance to goal of 1.7% using a sample of patients managed with one oral AHA from the Clinical Practice Research Datalink (CPRD) in the UKCitation14.
In addition, this study showed that patients who failed MM and received intensified treatment were slightly younger, more likely to be white, had higher baseline HbA1c and were more likely to have had microvascular complications than patients who failed MM and did not receive intensified treatment. These findings were like those of Yu et al. who reported that younger age, higher HbA1c, and presence of certain comorbid conditions were associated with prescribing an additional AHA to patients with T2DM using metformin with suboptimal glycemic controlCitation29. In addition, a recent study reported that 42.9% of patients did not reach an HbA1c goal of <7% within 3 months of MM initiation and showed Asian ethnicity was associated with an increased risk of clinical inertia (i.e. treatment for T2DM was not appropriately intensified for a patient not under control) and congestive heart failure (CHF), chronic kidney disease (CKD) and cardiovascular/cerebrovascular disease trended towards decreased likelihood of clinical inertiaCitation30.
The impact of suboptimal glycemic control is well-described in the literature. Patients who fail to meet their HbA1c targets face elevated risks of negative long-term health consequences, such as microvascular complicationsCitation5,Citation10,Citation11, myocardial infarctionCitation11, and deathCitation11. Pantalone et al. reported that patients who failed MM and received intensified treatment within six months were more likely to achieve glycemic control that persisted over time than those who received intensified treatment after six months, suggesting that failure to intervene early may prevent patients from achieving and maintaining glycemic controlCitation15. The results of our study indicate that many patients with T2DM may face these elevated risks due to clinical inertia and should receive intensified treatment earlier in the treatment paradigm.
Limitations
These results should be interpreted considering the study’s inherent limitations. We were unable to determine each patient’s individualized HbA1c target, nor were we able to determine if patients were titrating their metformin dose before adding another AHA to their regimens. Furthermore, we were not able to assess patients’ compliance with their physicians’ instructions or if they filled their prescriptions. Studies that include dose of metformin and prescription filling data would help to further ascribe poor glycemic control to clinical inertia.
The GE Centricity EMR database collected information mostly from primary care physicians and, therefore, data about visits to specialists and hospitalizations may not be included. Serious comorbid conditions that require hospitalization, drug use during hospitalization, specialists care, or prescriptions written by specialists may, similarly, be underreported. Unobserved physician factors, such as age, level of training, and experience and unobserved patient factors, such as medication compliance, lifestyle choices, attitudes and health behaviors, and ability to afford medication may be important determinants of intensification timing and glycemic goal attainment. However, to the extent the patient factors are correlated with smoking status, body mass index, age, and sex, which were observed, potential bias due to omitted factors is minimized. Furthermore, patients who did not achieve glycemic control were only included in the sample if post-MM HbA1c measures were available. HbA1c measures obtained by specialists or while patients were in hospital could explain the absence of those measures.
Although the inability to account for salient, yet unobserved, factors may confound the comparison of post-MM distance to goal between patients who did and did not receive intensified treatment after 90 days of MM without achieving glycemic control, it was not our objective to make that comparison. While recognizing that those unobserved factors may be important for explaining the variation in observed post-MM HbA1c and distance to goal, we also recognize that those values reflect clinical reality and can serve as benchmarks to which future data can be compared.
Conclusion
A proportion of patients in the US with T2DM using MM do not achieve glycemic control (HbA1c < 7.0%) after 90 days of treatment and almost a quarter of these patients do not receive treatment intensification. Patients who failed MM and eventually received intensified treatment did so when their HbA1c distance to goal exceeded the level at which one add-on therapy alone might be sufficient to bring them to goal. These results are consistent with previous research on HbA1c at time of treatment intensification among patients who have not reached glycemic control. In addition to confirming previous research, our results also provide new information on HbA1c and distance to goal specifically for patients who failed MM. Future research to understand why clinical inertia exists in diabetes management and how to overcome the barriers to timely intensification is warranted to improve care for T2DM patients.
Transparency
Declaration of funding
This study was funded by Merck & Co., Inc., Kenilworth, NJ, USA.
Declaration of financial/other relationships
GF, TW and SR are employees of Merck & Co., Inc., Kenilworth, NJ, USA. HH, JL, AM and KI were employees of Merck & Co., Inc., Kenilworth, NJ, USA. at the time of the analysis. BS and AF are external contractors whose analysis services were paid for by Merck & Co., Inc., Kenilworth, NJ, USA. Peer reviewers on this manuscript have received an honorarium from CMRO for their review work but have no other relevant financial relationships to disclose.
Acknowledgements
None reported.
References
- American Diabetes Association. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S13–s27.
- Fowler MJ. Microvascular and macrovascular complications of diabetes. Clin Diabetes. 2008;26(2):77–82.
- American Diabetes Association. Glycemic targets: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S55–S64.
- Nathan DM, Genuth S, Lachin J, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–986.
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837–853.
- Ohkubo Y, Kishikawa H, Araki E, et al. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Diabetes Res Clin Pract. 1995;28(2):103–117.
- Reichard P, Nilsson BY, Rosenqvist U. The effect of long-term intensified insulin treatment on the development of microvascular complications of diabetes mellitus. N Engl J Med. 1993;329(5):304–309.
- American Diabetes Association. Pharmacologic approaches to glycemic treatment: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S73–S85.
- National Institute for Health and Care Excellence. NICE clinical guideline. Type 2 diabetes in adults: management. [updated 2015 Dec 02; cited 2018 July 16]. Available from: http://nice.org.uk/guidance/ng28.
- Reichard P. Are there any glycemic thresholds for the serious microvascular diabetic complications?. J Diabetes Complications. 1995;9(1):25–30.
- Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–412.
- Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35(6):1364–1379.
- Fox KM, Gerber Pharmd RA, Bolinder B, et al. Prevalence of inadequate glycemic control among patients with type 2 diabetes in the United Kingdom general practice research database: a series of retrospective analyses of data from 1998 through 2002. Clin Ther. 2006;28(3):388–395.
- Khunti K, Wolden ML, Thorsted BL, et al. Clinical inertia in people with type 2 diabetes: a retrospective cohort study of more than 80,000 people. Diabetes Care. 2013;36(11):3411–3417.
- Pantalone KM, Wells BJ, Chagin KM, et al. Intensification of Diabetes Therapy and Time Until A1C Goal Attainment Among Patients With Newly Diagnosed Type 2 Diabetes Who Fail Metformin Monotherapy Within a Large Integrated Health System. Dia Care. 2016;39(9):1527–1534.
- Stark Casagrande S, Fradkin JE, Saydah SH, et al. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988–2010. Diabetes Care. 2013;36(8):2271–2279.
- Shah BR, Hux JE, Laupacis A, et al. Clinical inertia in response to inadequate glycemic control: do specialists differ from primary care physicians? Diabetes Care. 2005;28(3):600–606.
- Wetzler HP, Snyder JW. Linking pharmacy and laboratory data to assess the appropriateness of care in patients with diabetes. Diabetes Care. 2000;23(11):1637–1641.
- Zafar A, Davies M, Azhar A, et al. Clinical inertia in management of T2DM. Prim Care Diabetes. 2010;4(4):203–207.
- Berlowitz DR, Ash AS, Glickman M, et al. Developing a quality measure for clinical inertia in diabetes care. Health Serv Res. 2005;40(6 Pt 1):1836–1853.
- Schmittdiel JA, Uratsu CS, Karter AJ, et al. Why don’t diabetes patients achieve recommended risk factor targets? Poor adherence versus lack of treatment intensification. J Gen Intern Med. 2008;23(5):588–594.
- Sidorenkov G, Haaijer-Ruskamp FM, de Zeeuw D, et al. A longitudinal study examining adherence to guidelines in diabetes care according to different definitions of adequacy and timeliness. PLoS One. 2011;6(9):e24278.
- Ziemer DC, Miller CD, Rhee MK, et al. Clinical inertia contributes to poor diabetes control in a primary care setting. Diabetes Educ. 2005;31(4):564–571.
- Fu AZ, Qiu Y, Davies MJ, et al. Treatment intensification in patients with type 2 diabetes who failed metformin monotherapy. Diabetes Obes Metab. 2011;13(8):765–769.
- Crawford AG, Cote C, Couto J, et al. Prevalence of obesity, type II diabetes mellitus, hyperlipidemia, and hypertension in the United States: findings from the GE Centricity Electronic Medical Record database. Popul Health Manag. 2010;13(3):151–161.
- Crawford AG, Cote C, Couto J, et al. Comparison of GE centricity electronic medical record database and national ambulatory medical care survey findings on the prevalence of major conditions in the United States. Popul Health Manag. 2010;13(3):139–150.
- Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2018;61(12):2461–2498.
- Mata-Cases M, Benito-Badorrey B, Roura-Olmeda P, et al. Clinical inertia in the treatment of hyperglycemia in type 2 diabetes patients in primary care. Cur Med Res Opin. 2013;29(11):1495–1502.
- Yu S, Schwab P, Bian B, et al. Use of add-on treatment to metformin monotherapy for patients with type 2 diabetes and suboptimal glycemic control: A U.S. database study. J Manag Care Spec Pharm . 2016;22(3):272–280.
- Kartoun U, Iglay K, Shankar RR, et al. Factors associated with clinical inertia in type 2 diabetes mellitus patients treated with metformin monotherapy. Cur Med Res Opin. 2019;35(12):2063–2070.