Abstract
Objective
Human Immunodeficiency Virus (HIV) prevalence has substantially increased over the years, leading to increased direct medical costs. The aim of the present study was to assess the long-term cost of HIV care in Greece incurred over the last decade.
Methods
In order to assess the long-term cost of HIV care, a cost analysis was undertaken for three discrete time points (which reflect major changes in the HIV treatment paradigm), incorporating the evolution of the cost of pharmaceuticals, hospitalization, primary care visits and diagnostic tests. The cost per life year gained (LYG) was also estimated.
Results
Total cost of HIV care increased by 57% over the last decade (€53.7 million in 2010 vs €84.5 million in 2019), which can be mainly attributed to a 107% (5084 in 2010 vs. 10,523 in 2019) increase observed in the number of people living with HIV (PLWH) under care. As a result, the cost per person on treatment has decreased by 24.0% (€10,567 in 2010 vs €8032 in 2019). Lifetime cost was lower and life expectancy higher in 2019 compared to 2010, leading to a – €711 cost per LYG, suggesting that the current treatment paradigm produces better health outcomes at a lower cost compared to a decade ago, implying that resources are used in a more efficient way.
Conclusion
The paper presents some evidence towards the direction that HIV management in Greece can be considered efficient in both clinical and financial terms, as it offers measurable clinical outcomes at well-controlled, almost inelastic spending.
Introduction
HIV is one of the world’s most serious public health challenges. Since the approval of zidovudine in 1987, the first medication for Acquired Immunodeficiency Syndrome (AIDS), significant advancements in antiretroviral therapy (ART) have contributed to transforming a life-threatening disease for people living with HIV (PLWH) into a chronic conditionCitation1. The life expectancy of adults with HIV infection is similar to the life expectancy of the general populationCitation2. This is attributable to a great extent to newer, innovative ART that offers improved results not only in terms of viral suppression but also in terms of improved tolerability and greater adherence to medication due to reduced pill burdenCitation3. Consequently, an increase in direct medical costs is observedCitation4,Citation5 as HIV prevalence has grown over the years and PLWH are treated over their lifetimeCitation6.
In alignment with literature observationsCitation6, HIV prevalence in Greece has been growing with time, although new diagnoses have been generally declining since 2012Citation7. In 2019, women represented 22.4% of new HIV diagnoses, a rate close to that of the European Union (EU) average, where the male to female ratio was 3:1Citation8. Additionally, the main transmission mode of HIV both in Greece (41.0% of new diagnoses)Citation7 and the EU (38.7%)Citation8 is sex between men.
As Greece is still recovering from a long recession period, the country’s healthcare has faced significant reductions in its funding. This underfunding of healthcare can be largely reflected in the overall reduction of public health expenditure between 2010 and 2018 (by 42.1%)Citation9. Characteristically, in 2009, public health expenditure accounted for 6.5% of gross domestic product (GDP), while in 2018 for 4.5%, leaving Greece far below the European average (7.9%)Citation9. In order for the healthcare system to respond to these contractions in healthcare funding, a cost-containment policy has been implemented, affecting decision-making in healthcare, removing the focus of decisions away from epidemiologic or efficiency considerations, across all areas of care, including communicable diseases.
Despite the challenges that healthcare has been facing over the past decade, HIV management in Greece can be considered a well-organized area of provision of care. The systematic epidemiological surveillance by the National Public Health Organization (EODY), the operation of a registry for PLWH under care, the consistent recording of treatment regimens dispensed, physician’s freedom in treatment choice according to individualized conditions and needs of PLWH and patient management by Infection Disease Units (IDUs), have all contributed to an improved and efficient disease management.
Bearing in mind the above, the aim of the present study was to assess the long-term cost of HIV care during the period 2010–2020, in order to assess the efficiency of HIV management in the Greek healthcare system. Such an assessment of HIV care cost and in conjunction with the expected health outcomes could facilitate future decision-making regarding the funding of HIV, highlighting the need to safeguard the sustainability of the improvements achieved in the overall disease management so far and providing a platform for integrating cost-efficiency into policy decisions in health.
Methods
A costing study was undertaken to estimate both pharmaceutical treatment costs and disease management costs of HIV during the period 2010–2020 incurred by the healthcare system. Drug acquisition costs, diagnostic tests costs and hospitalization and primary care costs were included in the analysis.
As a time-series analysis could not be conducted due to limitations in available epidemiological data regarding the number of PLWH that are under care, discrete-time points that constituted benchmarks in the evolution of HIV management were selected. Time points selected refer to: 2010 – the year when the first available single-tablet regimen was recommended as a first-line treatment option in the adopted guidelinesCitation10; 2015 – results from The INSIGHT START Study GroupCitation11 were published and WHO guidelinesCitation12 recommended the immediate initiation of ART, regardless of the clinical stage and the number of cluster of differentiation 4 (CD4) lymphocytes and 2019 – current clinical practice with the use of newer ART and focus on long-term health for PLWH.
For the estimation of the respective costs, all available sources were used including both international and grey literature. The number of PLWH on treatment for each investigated year was estimated based on data from official national sources and expert opinion. More specifically, as data regarding the number of PLWH on treatment were not available for the year 2010, the most recent available data (number of PLWH and number of PLWH on treatment) were used to assess the proportion of PLWH on treatment for the year 2011Citation13. Experts, then, validated that the proportion of PLWH on treatment in 2010 was the same as in 2011. Subsequently, this rate was applied to the available epidemiological 2010 data to derive the number of PLWH on treatmentCitation14. For the year 2015, the number of PLWH receiving treatment was assessed based on data from the Hellenic Public Health OrganizationCitation15 and validated by expert opinion. Finally, the number of PLWH on treatment in 2019 was sourced directly from the Hellenic Public Health OrganizationCitation7. Expert opinion was elicited from three experts with long-term professional and/or academic experience with the management of HIV infection.
Pharmaceutical cost represented the cost of all available treatment options at each time-point, including the cost and utilization of generic drugs in cases where generic options were available. Pharmaceutical costs were estimated in accordance with the number of patients receiving each treatment per year, dosages and drug acquisition costs. Dosages were sourced from the respective Summaries of Product Characteristics (SmPCs) and validated by the experts. Drug acquisition costs were derived from the respective Official Medication Price BulletinsCitation16–20, deducting mandatory discounts for hospitals and state pharmacies, according to current legislationCitation21,Citation22. In cases where there were multiple Price Bulletins in the reference year, a weighted average was used. In Greece, HIV-positive people are exempted from co-payment for ART, and thus, ART cost was assumed to be solely borne by the third-party payerCitation23. Drug costs are expressed in par values.
The number of patients receiving each treatment was estimated by applying the corresponding market share to the number of PLWH on treatment per investigated year. As there is no publicly available database to retrieve exact market shares of all available ART in the market, these were derived from a long-run HIV panel survey conducted by IQVIA for 2015 and 2019Citation24. For 2010, an approximation of the market (treatments and the corresponding market ratios) was used based on expert opinion, as no other source was available.
Since there were no available data regarding the fluctuation of annual hospitalizationsCitation25–29 and primary care visitsCitation25,Citation30–32 for PLWH in Greece, these were derived from the literature and, subsequently, validated by the three experts in the management of HIV infection. Hospitalization costs were estimated based on the rate of PLWH on treatment that requires inpatient care for all causes (applied to the number of PLWH receiving treatment each year) and the mean hospital stayCitation25–29, as well as the corresponding inpatient stay costs, as derived from the Greek Diagnosis-Related Groups (DRG) listCitation33. Primary care visit costs were estimated based on the frequency of primary care visits per investigated yearCitation25,Citation30–32 of PLWH on treatment and the cost per physician visit according to the published legislated feesCitation34. The costs of tests/examinations were estimated taking into account the types and number of tests/examinations and the corresponding unit costs. The number and types of tests/examinations per investigated year were derived from national and international guidelines for the management of HIV infectionCitation35–37 and validated by the experts, while the cost per test/examination from the National Organization for the Provision of Health ServicesCitation38. Costs of primary care visits and tests/examinations were applied to the total number of PLWH on treatment each year.
Finally, the analysis also included an estimation of the cost per life year gained (LYG), to assess the long-term efficiency of HIV treatment in 2015 and 2019 versus 2010. Due to the lack of country-specific data on patient outcomes, the required data were sourced from a relevant appropriate studyCitation2. According to the latest available data published by Marcus et al., overall life expectancy at 21 years of age increased from approximately 50.0 to 56.0 years for individuals with HIV infection in 2016Citation2. As there are no more recently available data, a conservative assumption was made for 2019, that is, no further improvements in life expectancy are accounted for. Lifetime treatment costs were estimated based on treatment cost per PLWH for overall life expectancy, applying a 3% discount rate per annum. An assumption was made that all individuals will remain on the same treatment for the rest of their lives and potential changes in costs from switching, non-adherence or discontinuations are not accounted for in the analysis.
Results
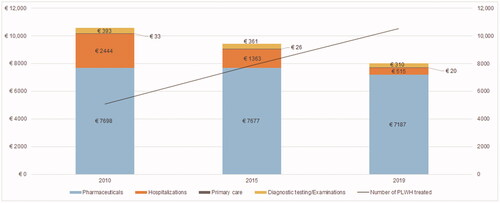
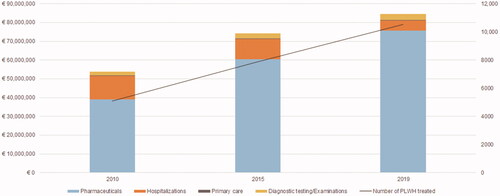
The total pharmaceutical cost, in nominal values, for 2010, 2015 and 2019 was estimated at €39.1 million, €60.5 million and €75.6 million, respectively (). This can be mainly attributed to the fact that the number of PLWH receiving ART doubled (107%) between 2010 and 2019 (5084 in 2010 vs. 10,523 in 2019) (). The average pharmaceutical cost per patient has decreased by 6.6%, from €7698 in 2010 to €7187 in 2019, despite the introduction in the market of a noteworthy number of newer ART. The rate of increase in the total treatment expenditure is lower than the rate of increase of PLWH under care.
Table 1. HIV treatment cost, 2010, 2015, 2019 (par values), Greece.
Other costs related to HIV care were found to have significantly decreased during the last decade (). More specifically, the cost of hospitalizations has decreased from €12.4 million in 2010 to €5.4 million in 2019, which is a 56.4% reduction. shows the respective variation for the independent components of resource use, confirming that the average total per patient HIV management cost (including pharmaceuticals) has declined by 24.0% in the last decade, from €10,567 in 2010 to €8032 in 2019.
In health economics terms, the lifetime treatment cost per person living with HIV and receiving ART was estimated to be lower in 2019 compared to previous years, namely €193,801 versus €207,014 in 2015 and €198,068 in 2010, respectively. The results of our analysis demonstrate that cost per LYG in 2019 was negative compared to 2010, indicating that current treatment is both more effective and produces savings, thus, proving to be a more efficient allocation of resources for the healthcare system in Greece. shows life expectancy, life treatment cost and cost per life-year gained in detail.
Table 2. Life expectancy, life treatment cost and cost per life-year gained of PLWH, 2010, 2015, 2019, Greece.
Discussion
Globally, health expenditures continue to rise mainly due to the ageing population, changes in epidemiology and expensive technological advancements. There is an increasing need for modern healthcare systems to examine how to contain healthcare costs while ensuring equitable access to and high quality of services, without compromising the status quo.
The present study estimated the pharmaceutical costs and disease management costs of HIV for the past decade, with an aim to assess the long-term efficiency of HIV therapeutic management in Greece from the healthcare system perspective.
In Greece, by end of 2019, more than 18,000 persons had been diagnosed with HIV, while recorded deaths among people with AIDS were estimated at 2070Citation39. Latest estimations show that approximately 81% of PLWH are diagnosed, of whom 88% ever initiated ART, resulting in almost 10,500 people with HIV under care in GreeceCitation40. Additionally, due to the increasing effectiveness of the pharmaceutical management of HIV, the present study also recorded savings in other forms of care such as hospitalization, diagnostic testing or primary care visits.
The results of the analysis show that the overall HIV treatment cost has almost doubled between 2010 and 2019, which is in line with relevant research findings from the United States (US)Citation41. However, the results of the present analysis also demonstrate that, despite the increasing number of PLWH under care during the past decade, both the average pharmaceutical cost and overall HIV care cost per person on ART have decreased by 6.6% and 24.0%, respectively. On the contrary, an older study conducted in Italy had estimated that per capita cost increased by approximately 25% between 2003–2005 and 2012–2014 with ART accounting for the larger proportion of the cost (61.4% and 72.9% respectively)Citation42.
Despite the estimated reductions in per person on ART and overall HIV cost, the present study might underestimate the financial benefits of ART as, according to findings from the international literature, when costs of treatment are compared to full income benefits, the benefits in all regions substantially exceed the costsCitation43. Notably, it has been estimated that ART has led to the aversion of 9.5 million deaths worldwide in 1995–2015, accounting for $1.05 trillion in benefitCitation43.
If one also considers the (established) efficiency of ART on HIV infection prevention, as well as the increasing prevalence, life expectancy and the improved quality of life of PLWHCitation2,Citation6,Citation44,Citation45, such reductions on per person cost indicate that HIV funding is an efficient use of the National Health System (NHS) resources. Overall, in health economics terms, the present study suggests that HIV treatment may be considered “cost-effective” and an example of improved efficiency over time.
Epidemiological surveillance, early diagnosis, rapid treatment initiation and ongoing treatment monitoring and access to innovation according to personalized needs have contributed to the improvement of health outcomes of HIV care and the economic efficiency of the national healthcare system. In order to maintain and improve those outcomes, it is highly important that availability of and accessibility to the abovementioned services according to need, now and for the future are guaranteed.
Previously conducted studies have suggested that higher CD4 (cluster of differentiation 4) cell count is associated with lower HIV management cost compared to those with lower CD4 cell countCitation46 and that the lifetime HIV management cost (including the cost for managing opportunistic infections) is significantly lower for those diagnosed at early stage comparing to those diagnosed in more advanced stages (lower CD4 count)Citation47. Those findings demonstrate that early use of ART leads to reduced HIV care cost, making early diagnosis and immediate start of ART of utmost importance, not only in terms of health outcomes but also in terms of financial benefits.
In addition, according to a study conducted in Greece, the ageing of PLWH has led to an increased prevalence of comorbidities such as hypertension, dyslipidemia and chronic kidney diseaseCitation48. Bearing in mind that the life expectancy of PLWH will most likely keep increasing, more comorbidities associated with HIV or aging are expected to become more prevalent, especially cardiovascular and chronic kidney diseasesCitation49, highlighting the need to develop comprehensive management models for PLWH in the future.
Despite the significance of the present findings, the study bears some limitations that should be acknowledged. In particular, the life expectancy used in the analysis for 2019 was assumed to be the same as in 2016, since no more recent relevant data were available. Considering the improvement of life expectancy for PLWH in the last yearsCitation2, it can be expected that life expectancy in 2019 will be higher than the one used in the analysis, and, thus, its effect on the cost estimations may be underestimated.
Furthermore, the assumption that all individuals will remain on the same treatment for the rest of their lives and the fact that potential changes in costs from switching, non-adherence or discontinuations are not accounted for, may underestimate cost estimationsCitation50,Citation51. Despite that, the study managed to provide an insight regarding the lifetime ART cost in conjunction with the corresponding treatment efficacy in terms of life expectancy. The results of this analysis suggest that, from the third-party payer perspective, resource allocation in ART is more efficient today compared to a decade ago.
The present analysis relied on cumulative data for the consumption of ART and healthcare services for PLWH in Greece, while the use of medical data/files would result in more accurate estimations. However, as access to such data was not possible, the study utilized official resources and published data, which were validated by experts, in order to produce a reliable and documented estimation of costs.
Furthermore, a time series analysis was not available due to a lack of publicly available, epidemiological data regarding the number of PLWH under care. However, the use of the selected time points, which are major therapeutic benchmarks that transformed HIV management in Greece, reflect the respective trends.
Conclusion
The paper presents some evidence towards the direction that HIV management in Greece may be considered efficient in both clinical and financial terms, as it offers measurable clinical outcomes at a well-controlled, almost inelastic spending. In this light, HIV care spending can be viewed as an efficient investment for the NHS.
Transparency
Declaration of funding
The present study has been supported and funded by Gilead Sciences.
Declaration of financial/other relationships
D Theodoratou is an employee of Gilead Sciences. The authors report no other potential conflicts of interest for this work. Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author contributions
Athanasakis K: Conceptualization, data curation, methodology, data interpretation, manuscript revision; Naoum V: Formal analysis, investigation, data interpretation, manuscript drafting, manuscript revision; Naoum P: Formal analysis, investigation, manuscript drafting, manuscript revision; Nomikos N: Formal analysis, investigation, manuscript revision; Theodoratou D: Data curation, manuscript revision; Kyriopoulos J: Conceptualization, funding acquisition, methodology, manuscript revision. All authors gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Data availability statement
All sources of data supporting the results reported in the manuscript have been cited. Data sourced from expert opinion cannot be shared, as participants gave the researchers permission to use the provided data only for the analysis, but did not agree to sharing them or making them publicly available. Data from the IQVIA HIV panel survey cannot be shared due to business privacy restrictions. Retracted material can be made available from the corresponding author upon reasonable request.
References
- Mahungu TW, Rodger AJ, Johnson MA. HIV as a chronic disease. Clin Med. 2009;9(2):125–128.
- Marcus JL, Leyden WA, Alexeeff SE, et al. Comparison of overall and comorbidity-free life expectancy between insured adults with and without HIV infection, 2000-2016. JAMA Netw Open. 2020;3(6):e207954.
- Astuti N, Maggiolo F. Single-tablet regimens in HIV therapy. Infect Dis Ther. 2014;3(1):1–17.
- McCann NC, Horn TH, Hyle EP, et al. HIV antiretroviral therapy costs in the United States, 2012-2018. JAMA Intern Med. 2020;180(4):601–603.
- Ritchwood TD, Bishu KG, Egede LE. Trends in healthcare expenditure among people living with HIV/AIDS in the United States: evidence from 10 Years of nationally representative data. Int J Equity Health. 2017;16(1):188.
- GBD 2017 HIV collaborators. Global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2017, and forecasts to 2030, for 195 countries and territories: a systematic analysis for the global burden of diseases, injuries, and risk factors study 2017. Lancet HIV. 2019;6(12):e831–e859.
- Hellenic Public Health Organization. HIV λοίμωξη: προκαταρκτικά επιδημιολογικά δεδομένα, Οκτώβριος 2019 [HIV infection: preliminary epidemiological data, October 2019]. Hellenic Public Health Organization, Οffice of HIV infection and STDs; 2019. Greek. [retracted material]
- European Centre for Disease Prevention and Control, World Health Organization. HIV/AIDS surveillance in Europe 2020. 2019 data. Sweden: ECDC/Denmark: WHO. 2020.
- Hellenic Association of Pharmaceutical Companies. The pharmaceutical market in Greece. Facts & figures 2019. Athens: Hellenic Association of Pharmaceutical Companies; 2020. [cited 2021 May 21]. Available from: https://sfee.gr/wp-content/uploads/2020/07/F-F-2019-ENG-new.pdf
- European AIDS Clinical Society. Clinical management and treatment of HIV infected adults in Europe. Guidelines. Version 5. November 2009. Paris: European AIDS Clinical Society; 2009. [cited 2021 May 21]. Available from: https://www.eacsociety.org/files/2009_eacsguidelines-v5-english.pdf
- Lundgren JD, Babiker AG, Gordin F, et al. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015;373(9):795–807.
- World Health Organization. Guideline on when to start antiretroviral therapy and on Pre-Exposure prophylaxis for HIV. Switzerland: World Health Organization; 2015. [cited 2021 May 21]. Available from: https://apps.who.int/iris/bitstream/handle/10665/186275/9789241509565_eng.pdf.;jsessionid=BEF1EB0E516EC5CFD1ACD4BD98B0601C?sequence=1
- European Centre for Disease Prevention and Control. Joint technical mission: HIV in Greece 28–29 May 2012. Stockholm; 2013.
- Hellenic Centre for Disease Control and Prevention. HIV/AIDS Surveillance Report in Greece, 31-10-2010 (Issue 25). Athens 2010. Hellenic Centre for Disease Control and Prevention, 2010. [cited 2021 May 21]. Available from: https://eody.gov.gr/wp-content/uploads/2018/12/epidimiologiko-2010.pdf
- Hellenic Centre for Disease Control and Prevention. HIV λοίμωξη: νεότερα επιδημιολογικά δεδομένα, Οκτώβριος 2015 [HIV infection: latest epidemiological data, October 2015]. Hellenic Centre for Disease Control and Prevention, Office for HIV and STDs; 2015. Greek. [retracted material]
- Hellenic Ministry of Health. Medication Price Bulletin. [cited 2021 May 21]. Available from: https://www.sfee.gr/enieo-deltio-timon-farmakon-05-2009/
- Hellenic Ministry of Health. Medication Price Bulletin. [cited 2021 May 21]. Available from: https://www.sfee.gr/deltio-timon-farmakon-01-2010/
- Hellenic Ministry of Health. Medication Price Bulletin. [cited 2021 May 21]. Available from: https://www.sfee.gr/deltio-timon-farmakon-04-2010/
- Helenic Ministry of Health. Medication Price Bulletin. Available from: https://www.moh.gov.gr/articles/times-farmakwn/deltia-timwn/2681-deltio-timwn-farmakwn-anthrwpinhs-xrhshs-12-8-2014. Αccessed May 21, 2021.
- Hellenic Ministry of Health. Medication Price Bulletin. [cited 2021 May 21]. Available from: https://www.moh.gov.gr/articles/times-farmakwn/deltia-timwn/5546-deltio-timwn-farmakwn-anthrwpinhs-xrhshs-maioy-2018-11062018
- The President of the Hellenic Republic. ΦΕΚ Α 74/19.05.2017, Νόμος Υπ’ αριθμ. 4472 [Government Gazette Issue A 74/19.05.2017, Law Νο. 4472]; Athens: National Printing Office. Greek. [cited 2021 May 21]. Available from: http://www.et.gr/idocs-nph/search/pdfViewerForm.html?args=5C7QrtC22wEsrjP0JAlxBXdtvSoClrL8R5ab1UmX_HjtIl9LGdkF53UIxsx942CdyqxSQYNuqAGCF0IfB9HI6qSYtMQEkEHLwnFqmgJSA5WIsluV-nRwO1oKqSe4BlOTSpEWYhszF8P8UqWb_zFijAs3sW_wqEaAtER_qx6Ix3u0EXkm1g8CgA3p_dBREYUS
- Hellenic Ministry of Health. ΦΕΚ Β 4274/22.11.2019: Αριθμ. Δ3(α)οικ.82331 [Government Gazette Issue Β 4274/22.11.2019: Ministerial Decision Δ3(α)οικ.82331]; Athens: National Printing Office. Greek. [cited 2021 May 21]. Available from: https://www.moh.gov.gr/articles/times-farmakwn/ypoyrgikes-apofaseis-agoranomikes-diatakseis/5556-diatakseis-timologhshs-farmakwn-g5-a-oik-90552-fek-3890-b-2016?fdl=15704
- The President of the Hellenic Republic. ΦΕΚ Α 1/05.01.1999, Νόμος Υπ’ αριθ. 2676 [government gazette issue a 1/05.01.1999, law 2676]. Athens: National Printing Office. [cited 2021 October 15]. Available from: https://www.taxheaven.gr/law/2676/1999
- IQVIA Institute for Human Data Science. HIV Panel Database. HIV Audit, December 2019.
- Mostardt S, Hanhoff N, Wasem J, et al. Cost of HIV and determinants of health care costs in HIV-positive patients in Germany: results of the DAGNÄ K3A study. Eur J Health Econ. 2013;14(5):799–808.
- Coelho LE, Ribeiro SR, Veloso VG, et al. Hospitalization rates, length of stay and in-hospital mortality in a cohort of HIV infected patients from Rio De Janeiro, Brazil. Brazilian J Infect Dis. 2017;21(2):190–195.
- Mahlab-Guri K, Asher I, Bezalel-Rosenberg S, et al. Hospitalizations of HIV patients in a major israeli HIV/AIDS center during the years 2000 to 2012. Medicine. 2017;96(18):e6812.
- Taramasso L, Demma F, Bitonti R, et al. How has the cost of antiretroviral therapy changed over the years? A database analysis in Italy. BMC Health Serv Res. 2018;18(1):691.
- Bellino S, Borghetti A, Lombardi F, et al. Trends of hospitalisations rates in a cohort of HIV-infected persons followed in an Italian hospital from 1998 to 2016. Epidemiol Infect. 2019;147:e89.
- Johnson TL, Toliver JC, Mao L, et al. Differences in outpatient care and treatment utilization for patients with HIV/HCV coinfection, HIV, and HCV monoinfection, a cross-sectional study. BMC Infect Dis. 2014;14(1):217.
- Brennan-Ing M, Seidel L, Rodgers L, et al. The impact of comprehensive case management on HIV client Outcomes. PLOS One. 2016;11(2):e0148865.
- Krentz H, Vu Q, Gill M. Updated direct costs of medical care for HIV‐infected patients within a regional population from 2006 to 2017. HIV Med. 2020;21(5):289–298.
- Greek Diagnostic Related Groups System. [cited 2021 May 21]. Available from: http://kenicd.e-healthnet.gr/
- Hellenic Ministry of Health, Hellenic Ministry of Finance. ΦΕΚ Β 1181/08.05.2014: Αριθμ Υ9α/οικ 37139 [Government Gazette Issue Β 1181/08.05.2014; Joint Ministerial Decision Υ9α/οικ 37139]; Athens: National Printing Office. Greek. [cited 2021 May 21]. Available from: http://www.dsanet.gr/Epikairothta/Nomothesia/ya%20%CE%A59%CE%B1_14.htm
- European AIDS Clinical Society. Guidelines for the clinical management and treatment of HIV infected adults in Europe. Paris: European AIDS Clinical Society; 2007. [cited 2021 May 21]. Available from: https://www.eacsociety.org/files/2007_eacsguidelines-v1-english_oct_madrid_1.pdf
- European AIDS Clinical Society. Guidelines. Version 6- October 2011. Paris: European AIDS Clinical Society; 2011. [cited 2021 May 21]. Available from: https://www.eacsociety.org/files/2011_eacsguidelines-v6.0-english_oct.pdf
- Hellenic Centre for Disease Control and Prevention. Κατευθυντήριες οδηγίες χορήγησης αντιρετροϊκής αγωγής και θεραπείας καιροσκοπικών λοιμώξεων σε ενήλικες και εφήβους με HIV λοίμωξη [guidelines for the administration of antiretroviral treatment and treatment of opportunistic infections in adults and adolescents with HIV infection]. Athens: Hellenic Centre for Disease Control and Prevention; 2018. Greek. [cited 2021 May 21]. Available from: https://eody.gov.gr/wp-content/uploads/2018/12/antiretroiki-agogi-11-05-2018.pdf
- National Organization for the Provision of Health Services. Κατηγορίες ιατρικών πράξεων [Categories of Medical Procedures]. Greek. [cited 2021 May 21]. Available from: https://eopyyfiles.blob.core.windows.net/eopyysite/ServiceCategories/038dc470-fbe3-409b-bdd7-7efb3b37f984.pdf
- National Public Health Organization. HIV/AIDS surveillance report in Greece, 31-12-2019 (issue 34). Athens: National Public Health Organization; 2020. [cited 2021 May 21]. Available from: https://eody.gov.gr/wp-content/uploads/2018/12/epidimiologiko-deltio-hiv-2019.pdf
- Vourli G, Noori T, Pharris A, et al. Human immunodeficiency virus continuum of care in 11 European Union Countries at the end of 2016 overall and by key population: have we made progress? Clin Infect Dis. 2020;71(11):2905–2916.
- IQVIA Institute for Human Data Science. Medicine use and spending in the U.S. A review of 2018 and outlook to 2023. USA: IQVIA; 2019. Available from: https://www.iqvia.com/insights/the-iqvia-institute/reports/medicine-use-and-spending-in-the-us-a-review-of-2018-and-outlook-to-2023
- Quiros-Roldan E, Magoni M, Raffetti E, et al. The burden of chronic diseases and cost-of-care in subjects with HIV infection in a health district of Northern Italy over a 12-year period compared to that of the general population. BMC Public Health. 2016;16(1):1146.
- Forsythe SS, McGreevey W, Whiteside A, et al. Twenty years of antiretroviral therapy for people living with HIV: global costs, health achievements, economic Benefits. Health Aff. 2019;38(7):1163–1172.
- Oguntibeju OO. Quality of life of people living with HIV and AIDS and antiretroviral therapy. HIV AIDS. 2012;4:117–124.
- Pimentel GS, Ceccato MDGB, Costa JO, et al. Quality of life in individuals initiating antiretroviral therapy: a cohort study. Rev Saude Publica. 2020;54:146.
- Colin X, Lafuma A, Costagliola D, et al. The cost of managing HIV infection in highly treatment-experienced, HIV-infected adults in France. Pharmacoeconomics. 2010;28 Suppl 1:59–68.
- Farnham P, Gopalappa C, Sansom S, et al. Updates of lifetime costs of care and quality-of-life estimates for HIV-infected persons in the United States: late versus early diagnosis and entry into care. J Acquir Immune Defic Syndr. 2013;64(2):183–189.
- Pantazis N, Chini M, Antoniadou A, et al. The HIV patient profile in 2013 and 2003: Results from the Greek AMACS cohort. PLOS One. 2018;13(9):e0203601.
- Pelchen-Matthews A, Ryom L, Borges ÁH, et al. Aging and the evolution of comorbidities among HIV-positive individuals in a European Cohort. AIDS. 2018;32(16):2405–2416.
- Dunn K, Lafeuille MH, Jiao X, et al. Risk factors, health care resource utilization, and costs associated with nonadherence to antiretrovirals in Medicaid-Insured patients with HIV. JMCP. 2018;24(10):1040–1051.
- Kangethe A, Polson M, Lord TC, et al. Real-World health plan data analysis: key trends in medication adherence and overall costs in patients with HIV. JMCP. 2019;25(1):88–93.