Abstract
The infection caused by COVID-19 (i.e. corona virus disease 2019) has caused more than 5.2 million cases and more than 337,000 deaths worldwide. Italy was the European epicenter for virus spread and one with most cases and deaths. The first Italian patient was diagnosed on February 18th, a young man hospitalized in Lombardy (Northern Italy). The Italian government not only isolated the village where he lived, but a few days later put the entire country in lockdown. We have here analyzed the COVID-19 Italian data during the first three months after the outbreak and the effect of lockdown. COVID-19 virus has a high transmission rate and is associated with high fatality rate especially in the older population. The initial reproduction rate of the virus (R0) in Italy was between 2.1 and 3.3 in different Italian regions, with a doubling time between 2.7 and 3.2 days. The number of confirmed cases has now reached 229,000 but after the lockdown R0 is finally below 1. Despite the lockdown, the number of infected and deceased patients in Italy was very high, with a lethality rate higher than in other countries. It is likely that number of cases is underestimating the real since the number of asymptomatic and paucisymptomatic is relatively high. It is important to investigate which patients are more vulnerable and also if other co-factors can account for this high fatality rate, since this pandemia is far from being resolved.
Keywords:
Introduction
The COVID-19 (i.e. corona virus disease 2019) has caused more than 5.2 million cases and more than 337,000 deaths worldwide.Citation1 After China, Italy became the second country for virus spread, the first in Europe, and now has more than 229,000 confirmed cases and over 32,700 deaths.Citation1 In this paper we have analyzed the COVID-19 Italian data during the first three months since the beginning of the epidemic in our country and the effect of lockdown.
The first two documented cases of COVID-19 in Italy were a couple of Chinese tourists on January 30th, which were hospitalized in Rome. The next day the Italian Council of Ministers declared the state of health emergency for the new coronavirus epidemic, activating all the precautionary regulatory tools provided in Italy in these cases. After confirming the first 2 cases in Italy, the Government deemed it appropriate to terminate air links with China.Citation2
After the two Chinese tourists, no case was reported until February 18th when a young Italian man (38 y old) was hospitalized in the intensive care unit (ICU) of the hospital Codogno (in Lombardy, Northern Italy), for a pneumonia that was developing rapidly. The patient reported no travel to China or any contact with Chinese people, so initially he was not considered at risk for COVID-19, but he was tested because his condition was critical and he was not responding to treatment (data from Italian Health Ministry). During the following 24 hours, 36 additional cases were identified, without links to patient 1 or previously identified positive. On February 22nd, Italy registered the first patient to die of COVID in Italy, a 77 year old male resident in Vo’. No relationship was found between the cases in the two sites indicating that the virus was already present in the country. Two areas were indicated as clusters and placed under quarantine, 10 municipalities near Lodi and Milan, in Lombardy, and Vo’ near Padova in Veneto. However, as the number of positive cases was rapidly rising, the Italian Prime Minister decided to establish a national lockdown to try to stop the spread of the epidemy. The lockdown started on March 11th, that same day the WHO declared COVID-19 a global pandemic.
Italy was the first Western country to establish a national lockdown; this became a necessary procedure not only in Europe but also in Northern America. After almost 2 months of lockdown (Phase 1) till May 4th (Phase 2).
Data sources and analysis
For the analysis presented here we used publicly available data and de-identified
Data for number of cases, recovered, deceased and hospitalized persons in Italy were collected from the Italian Ministry of Health (Health http://www.salute.gov.it/ last access May 23, 2020).
Age and sex distribution and Lethality rates were obtained from Italian Istituto Superiore di Sanità.Citation3,Citation4
Global data were obtained from WHO websiteCitation1,Citation5 and from ECDC websiteCitation6 (data accessed till May 23, 2020).
European all-cause mortality was obtained by EuroMOMO monitoring system (https://www.euromomo.eu data accessed till May 23, 2020)
Timeline and management of COVID-19 in Italy
February 18th the first internal case of COVID-19 was diagnosed in Codogno (Lombardy, Northern Italy). The patient reported no travel to China or any contact with Chinese people, so he was not considered at risk for COVID-19. However, his wife remembered a dinner with a colleague that was in China during the previous weeks. Thanks to this information and the intuition of the doctors of the ICU they decided to test if he was positive for COVID-19 and this is how the patient 1 was found. Patient 0 was never found, the colleague of patient 1 that traveled to China tested negative for COVID-19, but during the following 24 hours, 36 additional cases were identified, without links to patient 1 or the previously identified positive individual.
On the 22nd of February 2020 a resident of the municipality of Vo, a small town near Padua, died of pneumonia due to COVID-19 infection.
On February 23rd, after the Ministry of Health defined the area around Codogno and the municipality of Vo’ (that are more than 200 km away) as two different “clusters of infection”. The Italian Prime Minister decided to place 10 municipalities in Lombardy region and the municipality of Vo’ in the Veneto region in quarantine for 2 weeks, with suspension of all work and educational activities and prohibition of exit from and access to the aforementioned municipalities. Most of the regions of Northern Italy closed schools and Universities.
On March 5th, the Italian Prime Minister announced that all schools and universities should be closed throughout Italy. At the same time, the new requirements included a) the suspensions of meetings and social events involving either healthcare personnel or personnel in charge of carrying out essential public services (e.g., health system, pharmacy, grocery stores) or of public utility (e.g., postal system, bank); b) stop of any kind of community events that did not allow for the interpersonal distance of at least one meter; c) sports events were allowed without in person audience; d) remote working was encouraged.
On March 8th, the situation was still critical and the entire territory of the Lombardy Region and 14 other Provinces (5 in Emilia-Romagna, 5 in Piedmont, 3 in Veneto and 1 in Marche) became “Red Zones”. People living in the “Red Zones” were told to absolutely avoid any movement into and out of these areas that was allowed only for emergencies or “proven working needs” and after authorization by the prefect.
The following day, March 9th, a new provision was announced that extended the measures pursuant to Article 1 of the Presidential Decree of March 8th to the whole national territory, in effect from March 10th . People were told to avoid leaving the house unless they have to go to work, for health reasons or other needs, e.g., the purchase of necessary goods (pharmacy or grocery stores).
Phase 1: lockdown
On March 11th the WHO declared COVID-19 a global pandemic. The same day the Italian Prime Minister announced the complete closure of commercial (including restaurants and pubs) and non-essential activities since there were still too many people moving in the cities, in particular in Lombardy region. With the fear of a blockade of public transport, thousands of people poured into stations in northern Italy heading south, i.e. returning to a family home.
On March 20th, however, the Minister of Health signed the first of two ordinances prohibiting: public access to parks, villas, play areas and public gardens, as well as to carry out recreational or recreational activities outdoors .
On March 21st, the Italian Prime Minister announced further restrictions within the nationwide lockdown, by halting all non-essential production, industries and businesses in Italy, following the rise in the number of new cases and deaths in the previous days. Italians were also banned from moving across Municipalities other than for “non-deferrable and proven business or health reasons or other urgent matters”
Many countries followed Italy in these lockdown procedures.
Phase 2: partial re-opening
On May 4th Italy started reopening some activities.
Trend in infection rates before and after lockdown
Two months after the first case, Italy has registered a total of 178,972 cases (April 19th),Citation3 that reached 227,204 on May 20thCitation4 (, Panel A). The number of hospitalized patients started to decease since April 4th (, Panel B), not only because of lockdown but also because early diagnose and better treatment. The number of active cases continued to rise till (April 19th) when it started to decrease slowly but they are still above 62,000 (, Panel B).
Figure 1. Panel A: distribution over time of total positive cases, recovered and deceased in the 3 months of the COVID-19 epidemy in Italy. Panel B: distribution over time of active cases, in hospital or in intensive care unit (ICU) or at home in quarantine. Panel C: distribution of total positive cases in various region of Italy at the end of May. Panel D: distribution of symptoms in positive cases: asymptomatic (with no apparent signs or symptoms of disease), paucisymptomatic (with general mild symptoms like general malaise and l ow grade fever, but no clear signs of disease); symptomatic includes mild symptomatic, ie those with clear but mild symptoms (e.g., respiratory disease) but not severe enough to require hospitalization, severe symptomatic, i.e., those that required hospitalization, and critical symptomatic, those requiring the admission to an Intensive Care Unit (ICU).
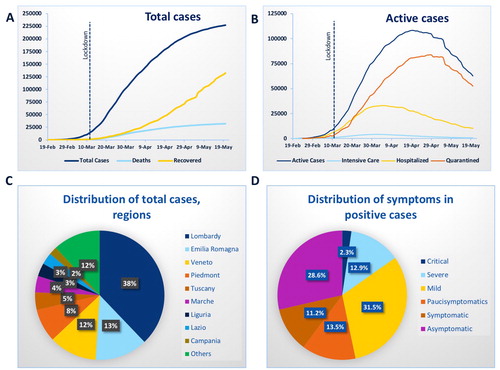
The great majority of cases were registered in Northern Italy, i.e., the most industrialized area; 38% of the patients in Lombardy, 13% in Emilia Romagna, 12% in Veneto, 8% in PiedmontCitation4 (, Panel C).
The virus has a high infectious capacity, but it is clear that thousands of people were already infected at the time of lockdown. We have data of the initial prevalence of the infection from the “Vo’ study”, where the first death due to COVID-19 was registered on February 22nd . After putting the village in quarantine, the Veneto region decided to test the entire population of Vo’.Citation7 The swab tests were done in 2,812 subjects at the beginning and end of 14 days of quarantine (total population 3,275 subjects, median age 47 y). After the tests were carried out it was found that 73 people (2.6% of the tested population) were already infected. The “Vo’ study” showed a higher prevalence of positive cases among those with age greater than 65 y (4.2%) while in the rest of the population the prevalence at the beginning of the pandemic was 1.2%. Moreover, most of the positive cases in Vo’ were asymptomatic. Thus, when the first Italian victim was identified (at the end of February), the infection had already reached very high levels, with a high prevalence of asymptomatic positive cases. The new serological tests confirmed that the virus was circulating in Milan at the outbreak start.Citation8
In the Vo’ study the entire population was tested again after 2 weeks of quarantine. They found that 29 subjects were still positive, 8 of which were new cases, showing a 90% drop in the infection rate (from 2.4% to 1.2% of tested people).Citation7
The lockdown was effective in reducing the number of cases, but the infection rate at the end of March was very high overall. ISS estimated that the initial reproduction rate of the virus (R0) was between 2.1 and 3.3 in different Italian regions, with a doubling time between 2.7 and 3.2 days.Citation9 We are currently (end of may 2020) with a reproduction rate below 1.
Symptomatic vs asymptomatic cases
The study in the village of Vo’ reported that at the beginning of the epidemy the number of asymptomatic subjects was 30.Citation7 Considering that the number of positive cases was 73, the prevalence of asymptomatic cases was 40%.Citation7
The current data (from the ISS reportCitation4) show how the number of asymptomatic (with no apparent signs or symptoms of disease), paucisymptomatic (with general mild symptoms like general malaise and l ow grade fever, but no clear signs of disease), and symptomatic, which includes mild symptomatic, ie those with clear but mild symptoms (e.g., respiratory disease) but not severe enough to require hospitalization, severe symptomatic, i.e., those that required hospitalization, and critical symptomatic, those requiring the admission to an Intensive Care Unit (ICU), is still quite relevant (, Panel D).Citation4
Valenti et al evaluated the prevalence of subjects with positive antibodies among apparently healthy blood donors in Milan between February 24th and April 8th and found that 5.1% had positive antibodies.Citation8
Hospitalization and recovery
Number of people that required hospitalization was very high at the beginning of March (65% as at March 10th), but started to decrease from April 4th, being 25% and 16% of active cases 2 and 3 months after COVID-19 outbreak respectively (). Similarly, those that required intensive care unit (ICU) decreased from 10% to 1% of active cases.
The number of recovered was still low at the end of April (28% of total cases) and at the end of May is 58% (, Panel B). These data show that positive patients with severe symptoms recover after several weeks.
Age and sex distribution of positive and deceased cases
ISS reported also data on age and sex distribution of positive and deceased patients. The initial data, 1 month from the first internal case, showed that the majority of infected people were men and the median age of infected was 62 years (, panel B), while at the end of May the sex distribution of infected reflects the Italian distribution, i.e., 46% of cases are of male sex, vs 54% females (, Panel C).
Figure 2. Sex distribution in Italy (total population Jan 1st,2020 n = 60.3 millions) (Panel A) and of total positive cases after 1 month (n = 101,739) (Panel B) and 3 months (n = 227,364) (Panel C) from the first case. Age distribution in Italy (Panel D) and of total positive cases after 1 month (Panel E) and 3 months (Panel F) from the first case.
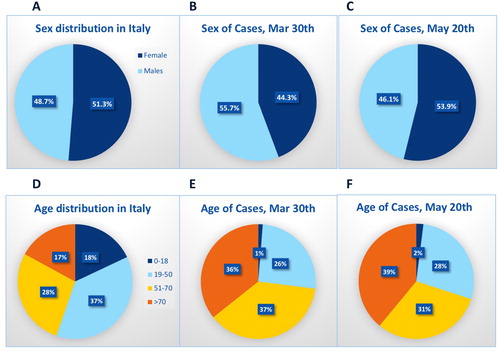
reports also the age distribution of positive cases that remained similar despite the lockdown, with more than 1/3 of people infected were above 70 years, with a median age of 62 yearsCitation4 (, Panel E and F).
Fatality rate and comorbidities in positive deceased patients
Case fatality rate (CFR) among positive cases was in average around 7% on March 17th (but much higher in the elderly population, i.e., between 12-22% in people older than 70 y) and the report on deceased published by the ISS on April 20th showed a CFR of 13.4%, that remained stable, (CFR 13.7% on May 20th) with higher CFR among people older than 70 y,Citation3,Citation4,Citation9 (, Panel B).
Figure 3. Sex (Panel A) and age (Panel B) distribution of deceased cases. Panel C Most common comorbidities observed in SARS-CoV-2 positive deceased patients by gender.
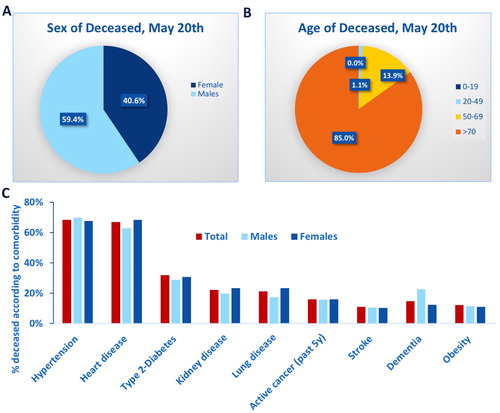
Most common comorbidities in positive Italian deceased patients during COVID-19 are shown in , Panel C. We observed a high prevalence of cardiovascular disease, mainly hypertension (68%), heart disease (that included a history of ischemic heart disease, 28%; Atrial Fibrillation 23%; Heart failure 16%), type 2 diabetes (30%), kidney (22%) and lung disease (21%).
Why infection and fatality rate are so high?
Overall, large increases in COVID-19 cases and deaths continue to be reported from the EU/EEA countries and the UK. The European Center for Disease prevention and Control (ECDC, https://www.ecdc.europa.eu) reported that the number of new cases and new deaths reported daily in few EU/EEA countries appears to have decreased. However, many EU/EEA countries are currently only testing severe or hospitalized cases, therefore these trends should be interpreted with caution.
It is now well established that the virus is transmitted through aerosol that may remain in the air. A document published on April 1st by the National Academies of Sciences, Engineering, and Medicine concluded that the virus might be spread also with normal breathing.Citation10 Moreover, it has been suggested that virus-laden aerosol might be resuspended by the doffing of personal protective equipment (PPE), the cleaning of floors, or the movement of staff.Citation10,Citation11 The paper by van Doremalen et al reported that COVID-19 virus nebulized in the ambient “remained viable in aerosols throughout the duration of the experiment (3 hours)”, with an estimated half-life of 1.09 hours while it is able to survive up to 3 days on plastic and steel.Citation12 The initial estimate (before lockdown) of the reproduction rate of the virus (R0), was between 2 and 3, which means that each infected person was spreading the infection to additional two-three persons. This high R0 explains the high case-load and rapid geographical spread observed in Italy. The lockdown was effective in reducing the index of the contagiousness and/or transmissibility of the virus and decreased the daily number of positive cases. However, the number of active cases is still high given that the average time of recovery is 4-5 weeks.Citation13
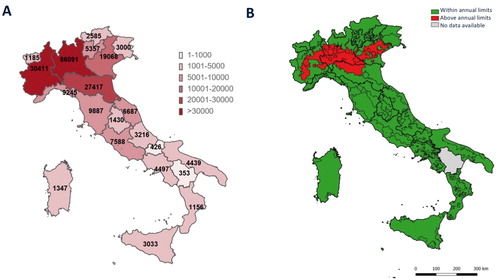
The great majority of positive cases with symptoms are older people that explains the high fatality rate. The European all-cause mortality monitoring system (EuroMOMO, https://www.euromomo.eu) showed all-cause excess mortality above the expected rate in recent weeks, in Belgium, France, Italy, Malta, Spain, Switzerland and the United Kingdom, mainly in the age group of 65 years and above. The fatality rate for COVID-19 in May in Italy (14.3%)Citation4 is much higher than in China (5.5%), USA (6.0%), Germany (4.6%), Spain (12.2%), while France (15.5%), UK (14.2%), Belgium (16.3%) show similar or higher CFR (data from WHO).Citation5 It is important also to highlight that the fatality rate in Italy was much higher in Northern Italy; on May 22nd CFR was 18.2% in Lombardy vs 14.7% in Emilia Romagna, 9.8% in Veneto, 10.1% in Tuscany, 8.9% in Lazio, 8.5% in Campania and 7.5% in Sicily). The reasons for these differences are in part due to the fact that the region in Northern Italy are more industrialized than Central or Southern regions and the outbreak was in Lombardy and Veneto.
However, differences among the different distribution of cases in regions of Northern Italy (, Panel C) are still not completed elucidated, since they have similar population density, age distribution, industrialization, and quality of the health system. One of the hypotheses is that since in this area there is high pollution for particulate matter PM2.5 and PM10,Citation14, this might have concurred to increase vulnerability of the subjects.Citation15 Moreover, traces of COVID-19 virus RNA were found in samples of PM10.Citation16 Several studies have shown that people living in highly polluted areas are at high risk of developing cardiovascular, cerebrovascular and respiratory diseases.Citation17,Citation18 Particulate matters are capable of penetrating deep into lung passageways, particularly PM2.5, and entering the bloodstream.Citation17 However, a direct cause -effect is difficult to prove, also because none of the abovementioned reports have investigated how long the virus might survive outdoors or proven if the virus might prolong its stability and viability by binding to fine particles (e.g., PM2.5 and PM10) present in high concentration in polluted air.Citation16
Figure 4. Panel A Total number of cases in different regions on May 20th. Panel B PM2.5 in red the areas where PM2.5 were above the annual limit (2017 data from ISPRA report “Analysis of trend of main atmospheric pollutants in Italy (2008-2017)”, ref.Citation14)
Importance of diet during COVID-19
Obesity, underweight and sedentary lifestyle are associated with an impairment in the immune system and worse response to viral and bacterial infections.Citation19 Western diet, rich in fat and sucrose and low in fiber, not only increases the risk of obesity and metabolic diseases, but also triggers basal immune response and inflammation, with lower acute response to lipopolysaccaradies (LPS)-driven sepsis leading to lead to more severe disease and poorer outcomes.Citation20 Thus, a healthy diet is important also to fight COVID-19 infection.
The quarantine and lockdown changed many people’s daily habits around the globe, and put them at risk of weight gain and sedentary lifestyle. However, it seems that weight gain was in average half of a pound or less,Citation21 although some gained weight. One explanation might be a healthier diet, due to the increased trend to home-cooked meals, so that people eat more nutritious foods and take in fewer calories.Citation22 It is well established that diet and certain nutrients have an impact on the immune system and are able to change the gut microbiota, thus helping also in fighting COVID-19.Citation23 A balanced diet, like the Mediterranean diet, gives the best intake of vitamins, minerals (e.g., zinc, iron, selenium, magnesium, and copper), antioxidants (live flavonoids and polyphenols), functional lipids like Omega-3 fatty acids, eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), or short chain fatty acids (SCFA), all known to have a positive effect on the immune system.Citation24,Citation25 Moreover, the adherence to the Mediterranean diet attenuates inflammation and coagulation process.Citation26 This is particularly important for COVID-19 since it is now established the immune response of patients with severe symptoms is characterized by overproduction of proinflammatory cytokines, activation of coagulation pathways, disruption of the endothelial function leading to multiorgan injury.Citation27,Citation28 On the other hand, a diet rich in protein and with low carbohydrates, like the ketogenic diet, might not be optimal during COVID-19. It has been shown that COVID-19 infection may cause ketosis and ketoacidosis even in subjects without diabetes.Citation29
Conclusions
The COVID-19 virus has a high transmission rate and is associated with high fatality rate especially in the older population. Patients with more than 1 comorbidity, mainly cardiovascular disease (hypertension) and diabetes were more likely to die because of COVID-19 virus, although the causes are still unclear. Despite the lockdown, the number of infected and deceased patients in Italy was very high, more than in other European countries, with a lethality rate higher than in USA or China. It is likely that number of positive cases is underestimating the real prevalence since the new tests are showing that number of asymptomatic and paucisymptomatic is relatively high. Although treatments of positive cases with symptoms are giving encouraging results, by decreasing number of hospitalized patients especially in ICU, it is important to try to prevent further infections. In this regard, it will be important to investigate which patients are more vulnerable and if other co-factors can account for this high fatality rate. A healthy lifestyle, including diets that strength the immune system, might help during the next months since COVID-19 pandemic is far from being resolved.
Author contributions
A.G. and S.B. designed research; A.G., M.G. and S.B. performed research; A.G. wrote the paper; M.G. and S.B. revised the paper.
| Abbreviations | ||
| COVID-19 | = | corona virus disease 2019) |
| R0 | = | reproduction rate of the virus |
| CFR | = | case fatality rates (CFR) |
| ICU | = | intensive care unit |
| ISS | = | Italian Health Institute |
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- WHO. “Who coronavirus disease (covid-19) dashboard”. 2020. https://covid19.who.int., Accessed 24 May 2020.
- Salute Md. Misure profilattiche contro il nuovo coronavirus (2019 - ncov). (20a00738). In: Health IMo editor. Misure profilattiche contro il nuovo coronavirus (2019 - ncov). (20a00738); Gazzetta ufficiale n.26, 1 February 2020; 2020.
- COVID-19 Task force of the Department of Infectious Diseases of the ISS. “Integrated surveillance of covid-19 in italy, april 20th, 2020”. Istituto Superiore di Sanita’. 2020. https://www.epicentro.iss.it/en/coronavirus/. Accessed 23 April 2020.
- COVID-19 Task force of the Department of Infectious Diseases of the ISS. “Integrated surveillance of covid-19 in italy, may 20th, 2020”. Istituto Superiore di Sanita’. 2020. https://www.epicentro.iss.it/en/coronavirus/., Accessed 24 May 2020.
- WHO. “Coronavirus disease (covid-2019) situation reports”. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/. Accessed 23 April 2020.
- European Center for Disease Prevention and Control E. “Coronavirus disease 2019 (covid-19) in the eu/eea and the uk– ninth update”. https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-rapid-risk-assessment-coronavirus-disease-2019-ninth-update-23-april-2020.pdf.
- Lavezzo E., Franchin E., Ciavarella C., Cuomo-Dannenburg G., Barzon L., Del Vecchio C., Rossi L., Manganelli R., Loregian A., Navarin N., Abate D., Sciro M., Merigliano S., De Canale E., Vanuzzo M. C., Besutti V., Saluzzo F., Onelia F., Pacenti M., Parisi S., Carretta G., Donato D., Flor L., Cocchio S., Masi G., Sperduti A., Cattarino L., Salvador R., Nicoletti M., Caldart F., Castelli G., Nieddu E., Labella B., Fava L., Drigo M., Gaythorpe K. A. M., Imperial College C.-R. T., Brazzale A. R., Toppo S., Trevisan M., Baldo V., Donnelly C. A., Ferguson N. M., Dorigatti I. Crisanti A. Suppression of a SARS-CoV-2 outbreak in the Italian municipality of Vo. Nature. Jun 30 2020. doi:10.1038/s41586-020-2488-1.
- Valenti L., Bergna A., Pelusi S., Facciotti F., Lai A., Tarkowski M., Berzuini A., Caprioli F., Santoro L., Baselli G., Della Ventura C., Erba E., Bosari S., Galli M., Zehender G. Prati D. SARS-CoV-2 seroprevalence trends in healthy blood donors during the COVID-19 Milan outbreak. medRxiv. 2020. doi:10.1101/2020.05.11.20098442. https://www.medrxiv.org/content/10.1101/2020.05.11.20098442v2
- Riccardo, F., Ajelli M., Andrianou X., Bella A., Del Manso M., Fabiani M., Bellino S., Boros S., Mateo Urdiales A., Marziano V., Rota M. C., Filia A., Ancona F., Siddu A., Punzo O., Trentini F., Guzzetta G., Poletti P., Stefanelli P., Castrucci M. R., Ciervo A., Benedetto C. Di, Tallon M., Piccioli A., Brusaferro S., Rezza G., Merler S. Pezzotti P. Epidemiological characteristics of COVID-19 cases in Italy and estimates of the reproductive numbers one month into the epidemic. medRxiv. 2020. doi:10.1101/2020.04.08.20056861. https://www.medrxiv.org/content/10.1101/2020.04.08.20056861v1
- Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats (2020). Rapid Expert Consultation on the Possibility of Bioaerosol Spread of SARS-CoV-2 for the COVID-19 Pandemic (April 1, 2020). The National Academies Press. Washington, DC. doi:10.17226/25769. http://nap.edu/25769
- Liu, Y., Ning Z., Chen Y., Guo M., Liu Y., Gali N. K., Sun L., Duan Y., Cai J., Westerdahl D., Liu X., Xu K., Ho K. F., Kan H., Fu Q. Lan K. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. Jun 2020. 582(7813), 557–560 doi:10.1038/s41586-020-2271-3.
- van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, et al. Aerosol and surface stability of sars-cov-2 as compared with sars-cov-1. N Engl J Med. 2020;382(16):1564–7. doi:10.1056/NEJMc2004973.
- Zhou, F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L., Wei Y., Li H., Wu X., Xu J., Tu S., Zhang Y., Chen H. Cao B.. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. Mar 28 2020., 395(10229), 1054–1062. doi:10.1016/S0140-6736(20)30566-3.
- ISPRA - Istituto Superiore per la Protezione e la Ricerca Ambientale: Analysis of trend of main atmospheric pollutants in italy (2008-2017). “Aria, cambiamenti climatici.” 2018. http://www.isprambiente.gov.it/it/pubblicazioni/rapporti/analisi-dei-trend-dei-principali-inquinanti-atmosferici-in-italia-2008-2013-2017.
- Conticini E, Frediani B, Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of sars-cov-2 lethality in northern Italy? Environ Pollut. 2020;261:114465. doi:10.1016/j.envpol.2020.114465.
- Setti, L., Passarini F., De Gennaro G., Barbieri P., Perrone M. G., Borelli M., Palmisani J., Gilio A. Di, Torboli V., Fontana F., Clemente L., Pallavicini A., Ruscio M., Piscitelli P. Miani A.. SARS-Cov-2RNA found on particulate matter of Bergamo in Northern Italy: First evidence. Environ Res. May 30 2020. 188, 109754. doi:10.1016/j.envres.2020.109754.
- WHO. “Ambient air pollution: Health impacts”. 2020. https://www.who.int/airpollution/ambient/health-impacts/en/. Accessed April 23, 2020.
- Crouse DL, Peters PA, Hystad P, Brook JR, van Donkelaar A, Martin RV, Villeneuve PJ, Jerrett M, Goldberg MS, Pope CA, 3rd, et al. Ambient pm2.5, O₃, and NOâ‚‚ Exposures and Associations with Mortality over 16 Years of Follow-Up in the Canadian Census Health and Environment Cohort (CanCHEC). Environ Health Perspect. 2015;123(11):1180–6. doi:10.1289/ehp.1409276.
- Moser J-A, Galindo-Fraga A, Ortiz-Hernández AA, Gu W, Hunsberger S, Galán-Herrera J-F, Guerrero ML, Ruiz-Palacios GM, Beigel JH, The La Red ILISG. Underweight, overweight, and obesity as independent risk factors for hospitalization in adults and children from influenza and other respiratory viruses. Influenza Other Respir Viruses. 2019;13(1):3–9. doi:10.1111/irv.12618.
- Napier BA, Andres-Terre M, Massis LM, Hryckowian AJ, Higginbottom SK, Cumnock K, Casey KM, Haileselassie B, Lugo KA, Schneider DS, et al. Western diet regulates immune status and the response to lps-driven sepsis independent of diet-associated microbiome. Proc Natl Acad Sci USA. 2019;116(9):3688–94. doi:10.1073/pnas.1814273116.
- Felber S. “Quarantine isn’t making us gain weight or slow down”. 2020. Accessed May 28, 2020.
- Wolfson JA, Bleich SN. Is cooking at home associated with better diet quality or weight-loss intention? Public Health Nutr. 2015;18(8):1397–406. doi:10.1017/S1368980014001943.
- Kau AL, Ahern PP, Griffin NW, Goodman AL, Gordon JI. Human nutrition, the gut microbiome and the immune system. Nature. 2011;474(7351):327–36. doi:10.1038/nature10213.
- Prasad AS. Zinc in human health: Effect of zinc on immune cells. Mol Med. 2008;14(5–6):353–7. doi:10.2119/2008-00033.Prasad.
- Calder PC, Carr AC, Gombart AF, Eggersdorfer M. Optimal nutritional status for a well-functioning immune system is an important factor to protect against viral infections. Nutrients. 2020;12(4):1181. doi:10.3390/nu1204
- Chrysohoou C, Panagiotakos DB, Pitsavos C, Das UN, Stefanadis C. Adherence to the mediterranean diet attenuates inflammation and coagulation process in healthy adults: The Attica study. J Am Coll Cardiol. 2004;44(1):152–8. doi:10.1016/j.jacc.2004.03.039.
- Jose, R. J. Manuel, A. COVID-19 cytokine storm: the interplay between inflammation and coagulation. Lancet Respir Med. Jun 2020. 8(6), e46–e47. doi:10.1016/S2213-2600(20)30216-2.
- Levi, M., Thachil J., Iba T. Levy J. H. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. Jun 2020. 7(6), e438–e440. doi:10.1016/S2352-3026(20)30145-9.
- Li, J., Wang X., Chen J., Zuo X., Zhang H. Deng A.. COVID-19 infection may cause ketosis and ketoacidosis. Diabetes Obes Metab. Apr 20 2020. doi:10.1111/dom.14057
