ABSTRACT
Objectives
This scoping review aims to examine the caregiving experiences of Korean American caregivers of persons with dementia.
Methods
A comprehensive electronic search was conducted within 5 databases (PubMed, CINAHL, Web of Science, Embase, PsycINFO-ProQuest) for papers published from 01/01/00 −01/24/22. Seventeen articles met the inclusion criteria. Thematic analysis was used to summarize key findings from these papers.
Results
Most Korean American dementia caregivers were immigrants and wives/daughters/daughters-in-law. Two themes emerged: 1) how Korean American caregivers perceived their caregiving experiences, and 2) how Korean American caregivers perceived their caregiving support services. Korean American caregivers often experience poor mental health and burden. Social support and familism were found to be two of the most important factors that determine their attitudes toward caregiving. Most reported barriers to utilizing public services. Challenges in finding culturally relevant resources were common.
Conclusions
Dementia caregiving is a significant public health problem facing Korean Americans. Recommendations for future research are provided.
Introduction
Dementia and dementia caregiving pose significant public health concerns in the United States (US). One-third of older US adults die from dementia – a range of conditions associated with cognitive decline that can interfere with daily function and independence (Alzheimer’s Association, Citation2022). The most prevalent form of dementia among older adults aged 65 and older is Alzheimer’s disease (AD) (60–80%) (Alzheimer’s Association, Citation2021).
Older adults living with Alzheimer’s disease and related dementias (ADRD) tend to receive assistance from family or informal caregivers (92%) (Kasper, Freedman, Spillman, & Wolff, Citation2015). In 2019, more than 16 million Americans provided unpaid care for persons with dementia (PWD): these hours of unpaid care amount to 18 billion hours (valued at $44 billion) (Alzheimer’s Association, Citation2020). Of importance, informal caregivers of people with dementia report poorer physical and mental health than those of other chronic conditions (Jones et al., Citation2017).
Despite the public health significance of dementia caregiving, there is limited research in this area on Asian Americans, who are the fastest growing racial group and projected to become the largest group of immigrants in the US in the coming decades (Pew Research Center, Citation2017). Korean Americans in particular are one of the largest Asian American populations, with an estimated 1,908,000 residing in the US as of 2019, 59% of whom are foreign-born, and 12% are 65 years old and older (with a higher proportion of 20% among those who are foreign-born) (Budiman, Citation2021). A higher proportion of older Korean Americans are living in poverty compared to Asian Americans overall (19% vs. 12%, respectively) (Budiman, Citation2021), and half of foreign-born Korean Americans have limited English proficiency (Migration Policy Institute, Citation2017). In 2019, the median annual household income for Koreans in the US ($72,200) was lower compared to the median for all Asian Americans ($85,800) (Budiman, Citation2021). These unique characteristics of Korean Americans including the high proportion of limited English proficiency may pose as a challenge for Korean American caregivers of persons with dementia.
Moreover, caregiving for Korean Americans is greatly influenced by cultural beliefs, customs, and values. The majority of older Korean Americans tend to retain traditional Korean cultural values (Jang, Kim, Chiriboga, & Kallimanis, Citation2007). Korean culture is heavily shaped by collectivism and Confucianism (Oak & Martin, Citation2000) contrary to the Western emphasis on individualism and autonomy. Collectivism is a significant element of Korean culture and Koreans identify strongly with their in-group (e.g., family), thus, Koreans place greater value on interpersonal relationships and interdependence. Confucian values – built upon principles of social order and clear hierarchy – are ingrained into Korean family structures and customs: these practices include filial piety (showing care and respect to one’s elders), authority of fathers/husbands, submission of individual to family, etc. (Lehrer, Citation1996).
Another factor that may potentially affect the caregiving experiences of Korean Americans is related to the US health and social services systems. For example, although Asian American caregivers including Korean Americans, are more likely than other racial/ethnic populations to want doctors and other health care professionals to ask them about what their care recipient’s needs are (AARP Public Policy Institute, Citation2020), Korean Americans with limited English proficiency are at increased odds of not having a usual source of care or regular health checkups (Jang & Kim, Citation2019). Compared to other older Asian Americans, fewer Korean American older adults have reported accessing healthcare systems on a regular basis (Nguyen, Citation2012). Moreover, more Asian American caregivers, including Korean Americans, find their role to be emotionally stressful compared to African American or Hispanic caregivers, and most Asian American caregivers report feeling that they do not have a choice in taking on their caregiving responsibility (AARP Public Policy Institute, Citation2020).
Given the rapidly growing Korean American population and dementia caregiving needs that will also increase significantly, it is important to understand what we know and what has been done in dementia caregiving for Korean Americans. We therefore used a scoping review methodology to examine the knowledge, attitudes, and experiences about dementia caregiving among Korean Americans. Findings from this review will provide directions for future research and inform the development of culturally and linguistically appropriate caregiving programs for Korean American dementia caregivers.
Methods
A scoping review was conducted to identify the knowledge gaps and scope the body of literature about Korean American dementia caregiving (Munn et al., Citation2018). Covidence, a web-based software platform that streamlines the production of systematic reviews (CitationCovidence systematic review software, No date) and is effective in identifying duplicate references (McKeown & Mir, Citation2021), was used to organize this scoping review search. The review was conducted by two primary reviewers (QL & JVL) and a secondary reviewer (VP). This review was developed using the scoping review methodological framework proposed by Arkley and O’Malley (Arksey & O’Malley, Citation2005) which consists of five steps:
Step 1: identifying the research question
Our research question is: What are Korean American dementia caregivers’ experiences including with dementia caregiving programs/interventions?
Step 2: identifying relevant studies
The search period was from 01/01/2000 to 01/24/2022 on five databases: Embase, PsycINFO ProQuest, PubMed, CINAHL, and Web of Science. Three primary terms within the research question were identified and used to develop the search strategy and identify relevant papers: Korean American, dementia, and caregiver.
To broaden the number of potentially relevant papers, similar search terms were subsequently developed for each concept. To capture articles relevant to Korean Americans, the following search terms were included: Korean Americans, Asian Americans, and Koreans. Search terms related to dementia, such as Alzheimer’s, mild cognitive impairment, and memory loss were identified and included in the second part of the search. For the third set of search terms, to capture articles relevant to caregivers’ experience and the use of resources, the search was expanded to include terms such as caregiver attitude, caregiver burden, caregiver burnout, caregiver health, caregiver network, caregiver support, and caregiver self-help.
Other information sources included reference lists in published papers, and consultation with field experts for other known published articles that were not found from the other sources.
Step 3: study selection
The studies were selected using a two-stage screening process. For the initial phase of the article identification process, the title and abstract of citations were screened independently by two members of the research team (QL & JVL). Studies that did not meet the minimum criteria were eliminated. The articles that did not have abstracts available were included for review of the full article. During the subsequent phase of the review, the full texts of articles that met the minimum inclusion criteria were further reviewed. Discrepancies related to study selection during these two phases were discussed and resolved by a third reviewer (VP) if they could not be addressed by the two initial reviewers alone.
Studies were eligible for inclusion if they broadly appeared to reference the target demographic and topic (). Both quantitative and qualitative studies were eligible for inclusion. Studies were included if they involved Korean American caregivers of people who had dementia (and/or other dementia-related conditions), and how caregivers perceived caregiving experiences and/or caregiving support services. Papers that “lumped” Korean Americans under “Asian” or “Asian American” were also retrieved and reviewed. Only original research papers that study Koreans who live in the US were included. Only English language papers were reviewed. Exclusion criteria was used to eliminate ineligible studies.
Table 1. Inclusion and exclusion criteria.
Citations were imported from each database the web-based systematic review software Covidence for title and abstract relevance screening and data characterization of full articles. The citations were imported and reviewed one database at time, and duplicates were removed after we reviewed the duplicate list that Covidence captured.
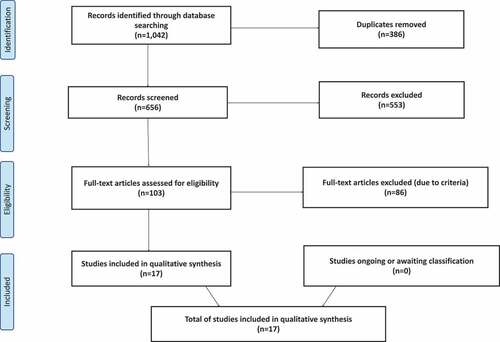
Of the 1,042 papers that were identified through the database screening, 17 papers met the inclusion and exclusion criteria for this literature review paper. Data were reported in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMAScR) (Tricco et al., Citation2018) ().
Step 4: charting the data
The data extracted from eligible studies were general study characteristics, such as location and year of publication; design; study aims; outcomes; participant information including ethnicity, age, gender, sample size, place of birth, years in the US, and type of caregiving relationship.
Step 5: collating, summarizing, and reporting results
The results section describes the bibliometric and other pertinent study information as well as the thematic analyses. The bibliometric metrics included authors, publication year, study aims, study sample size, study location, sample description, and main findings, which were presented by type of study (quantitative and qualitative).
Thematic analysis was conducted by analyzing the main objective and findings of the selected articles according to this paper’s research question. Two primary reviewers independently conducted thematic coding of the qualitative data using Luborsky’s thematic analysis approach (Luborsky, Citation1994) which is widely used in qualitative studies. Thematic analysis entails two approaches that are identifying repetition and analyzing central meaning; both complement each other through introducing emergent themes and reinforcing recurrent ones via systematic comparison. After the initial thematic analysis, the reviewers discussed discrepancies about the major themes until agreement was achieved. The combined analysis was then reviewed by two secondary reviewers to ensure accuracy and clarity of the themes. Data saturation, defined as no additional data were found, was reached for the prevalent themes (Glaser & Strauss, Citation1967).
Results
Of the 1,042 papers that were identified through the database screening, 17 papers met the inclusion and exclusion criteria for this review. There were 8 quantitative papers and 9 qualitative papers. Data were reported in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMAScR) (Tricco et al., Citation2018).
The results were summarized by type of methodological approach in (quantitative studies) and (qualitative studies). All the quantitative studies utilized cross-sectional surveys and the qualitative studies included focus groups or interviews. Half of the quantitative studies (Chun, Knight, & Youn, Citation2007; Jang, Yoon, Park, Rhee, & Chiriboga, Citation2018; Lee & Farran, Citation2004; Lee et al., Citation2017) while only one qualitative study (Richardson et al., Citation2019) had study samples that included Korean Americans along with other populations (e.g., Koreans from South Korea; other US subgroups). Common aims found in both qualitative and quantitative studies included exploring the knowledge about ADRD among caregivers, examining experiences and concerns related to ADRD caregiving, and identifying cultural factors that influence decisions to seek support from community services.
Table 2. Summary of quantitative papers on dementia caregiving among Korean Americans.
Table 3. Summary of Qualitative Papers on Dementia Caregiving among Korean Americans.
Regarding sample characteristics across studies, the average age range for Korean American caregivers was 54–72 years old. Majority of Korean American caregivers were married, wives/daughters/daughters-in-law of the care recipients, and first-generation immigrants from Korea. There was one study that included Korean American non-family caregivers who were professional personal care aids (Lee, Casado, & Hong, Citation2018). The average number of years that caregivers reported living in the US ranged between 12 and 33.
Of the 8 quantitative studies, the majority focused on factors influencing the attitudes and experiences of Korean American dementia caregivers. Two studies compared mental health outcomes between Korean American, South Korean, and Caucasian American caregivers (Chun et al., Citation2007; Lee & Farran, Citation2004). Three studies compared outcomes between child and spouse caregivers (Chun et al., Citation2007; Lee & Farran, Citation2004; Lee & Bronstein, Citation2010), and five studies examined how cultural factors influence the caregiving experience (Casado, Hong, & Lee, Citation2018; Chun et al., Citation2007; Lee & Farran, Citation2004; Lee & Bronstein, Citation2010; Lee & Choi, Citation2013). Five studies discussed community services, care-seeking behaviors and other resources related to ADRD (Casado et al., Citation2018; Jang et al., Citation2018; Lee et al., Citation2017; Lee & Casado, Citation2011; Lee & Choi, Citation2013).
Out of 9 qualitative studies, there were 2 studies that focused on experiences among former caregivers (Kim, Citation2009; Kong, Deatrick, & Evans, Citation2010) and the remaining 7 studies focused on experiences among current caregivers (Kim, Kehoe, Gibbs, & Lee, Citation2019; Lee Casado, Lee, Hong, & Hong, Citation2015; Lee et al., Citation2018; Lee & Smith, Citation2012; Lee & Yim, Citation2013; Richardson et al., Citation2019; Yong & McCallion, Citation2003).
Two key themes emerged from the review: 1) How Korean American caregivers perceived their caregiving experiences, and 2) How Korean American caregivers perceived their caregiving support services.
Theme 1: how Korean American dementia caregivers perceived their caregiving experiences
Knowledge and beliefs about ADRD among Korean American caregivers
Several of the studies reported on stigmatizing beliefs and the availability and impact of ADRD knowledge and resources. Three of these studies measured cultural stigma and beliefs about ADRD (Casado et al., Citation2018; Jang et al., Citation2018; Lee & Casado, Citation2011), and three measured prior exposure to people with dementia and current knowledge of the disease (Casado et al., Citation2018; Jang et al., Citation2018; Lee & Bronstein, Citation2010).
Some studies found that limited English proficiency played a role in how Korean American dementia caregivers generally had limited knowledge and/or held misconceptions regarding ADRD and how to take care of people with ADRD (Kim et al., Citation2019). One study found that when Korean American caregivers searched online for dementia-related information, they often did not do so in English (Lee et al., Citation2017).
Korean American caregivers expressed strong beliefs about the stigma of pity toward and public avoidance of persons with ADRD and their family members (Casado et al., Citation2018). Another study reported a misconception held among the majority of participants that dementia is a form of insanity (Lee & Casado, Citation2011). The belief that dementia is an inevitable part of aging was mentioned in four studies (Jang et al., Citation2018; Lee Casado et al., Citation2015; Lee & Casado, Citation2011; Richardson et al., Citation2019).
Many Korean American caregivers expressed their desire to learn more about how to take care of PWD (Lee et al., Citation2018; Lee & Yim, Citation2013). Those with greater knowledge of ADRD typically responded more favorably to care-seeking (Casado et al., Citation2018).
The impact of cultural factors in Korean American caregivers’ perceptions regarding caregiving
Cultural factors appeared to be important in Korean American caregivers’ perceptions about caregiving. For example, while Korean American caregivers in one study reported lower levels of familism than South Korean caregivers (Chun et al., Citation2007), participants in another study (Kong et al., Citation2010) mentioned “the Korean way of thinking” to describe their perceptions on caregiving such as the obligations to take care of their family member with dementia to keep their cultural roles and responsibilities. Similarly, Korean American caregivers from other studies expressed the need to uphold transgenerational continuity of filial piety and familism (Kim et al., Citation2019; Kim, Citation2009; Lee Casado et al., Citation2015). In addition, gender roles, family hierarchy (Richardson et al., Citation2019), marital commitment (of spouse caregivers) and cultural expectations (of child caregivers) (Youjung Lee & Smith, Citation2012) explained the high number of female caregivers in the articles for this review.
Mental and emotional outcomes associated with dementia caregiving
A wide range of psychological and emotional responses was shared by Korean American dementia caregivers including depression, anxiety, uncertainty, isolation, guilt, regret, grief, and loss (Kim et al., Citation2019). In some extreme cases, caregivers thought of suicide and death. Participants felt they were struggling and overwhelmed in caregiving responsibilities (Lee Casado et al., Citation2015). Caregiver burden and emotional distress were correlated with the care recipient’s disruptive behavior, memory problems and depression (Chun et al., Citation2007). Caregivers’ experience with confusion and hopelessness were also commonly reported (Richardson et al., Citation2019). Family stress due to strained relationships among family members when appointing and dividing caregiving responsibilities were also found (Kim et al., Citation2019; Lee Casado et al., Citation2015).
One study examined a culture bound syndrome called, Hwabyung, the most prevalent somatization among Koreans which arises when they are unable to confront their anger as a result of conditions which they perceive to be unfair such as caregiving stress among female Korean American dementia caregivers (Yong & McCallion, Citation2003). The participants of this study, who were daughters-in-law of the care recipients, also expressed the feeling of “being trapped” with their duties and experienced anger toward the fact that being a primary caregiver took away their freedom and joy.
Demographic characteristics and caregiving outcomes
The degree to which Korean American dementia caregivers experienced negative psychological outcomes varied based on the type of relationship they had with the care recipients as well as their socioeconomics. Of the eight quantitative studies, most caregivers were female and related to the care recipients as wives, daughters, or daughters-in-law (Casado et al., Citation2018; Chun et al., Citation2007; Jang et al., Citation2018; Lee & Farran, Citation2004; Lee et al., Citation2017; Lee & Casado, Citation2011; Lee & Bronstein, Citation2010; Lee & Choi, Citation2013). In one of the two studies that compared mental health outcomes among Korean American caregivers with those of Caucasian American and South Korean caregivers, spouse caregivers experienced higher levels of depression compared to child caregivers across all groups, and South Korean wives and daughters-in-law were more depressed than Korean American wives and daughters-in-law (Lee & Farran, Citation2004). Similarly, another study found that child caregivers reported more meaning in caregiving than spouse caregivers (Lee & Bronstein, Citation2010).
One study indicated that Korean American spouse caregivers found less meaning in dementia caregiving when compared to the child caregivers, and income showed a significantly positive correlation with the caregivers’ finding meaning in caregiving (Lee & Bronstein, Citation2010). Korean American child caregivers were generally more acculturated and had higher incomes than spouse caregivers (Chun et al., Citation2007; Lee & Bronstein, Citation2010). Korean American caregivers reported higher incomes and educational levels than South Korean caregivers (Chun et al., Citation2007). Among Korean American caregivers, those who had higher educational levels also had lower caregiver anxiety (Chun et al., Citation2007), and college education was associated with a more positive attitude toward care-seeking with AD specialists (Casado et al., Citation2018).
Theme 2: how Korean American caregivers perceived their caregiving support services
Needs and challenges to find support services
Many articles discussed the needs and challenges in finding support services by Korean American dementia caregivers. In one study, Korean American caregivers shared that they felt guilty when sending their family members with ADRD to nursing homes because that went against their beliefs about familial piety (Kong et al., Citation2010). Other Korean American caregivers expressed their needs for culturally responsive community services, and are often concerned over the differences in language, foods, bathing habits, and sleeping behaviors that may prevent their family members from receiving appropriate care (Lee Casado et al., Citation2015; Richardson et al., Citation2019). Korean American caregivers perceived that staff from community services may not be trained adequately to provide culturally sensitive care (Kim, Citation2009).
In addition, the lack of knowledge about available community-based services was also a barrier for Korean American caregivers to find additional supports (Richardson et al., Citation2019). Only one study found their participants were aware of several community services and had generally favorable attitudes toward people from community services (Lee & Casado, Citation2011). Two studies reported that most Korean American caregivers were not aware of any local organization or resources (Jang et al., Citation2018; Lee et al., Citation2017), and that when they searched online for dementia-related information, they often did not do so in English (Lee et al., Citation2017).
Self-care strategies and social support
Acceptance of dementia varied for caregivers given the various stages of the care recipients’ health (Kim et al., Citation2019; Kim, Citation2009) and some Korean American caregivers turned to self-defining (e.g., “caregiving was a continuation of the marital relationship”) and self-appraising (e.g., “It is God who rules how long we live on the earth. However, it was me … who provided care to him”) of their caregiving experiences (Kim, Citation2009). Korean American caregivers also valued familial support and found comfort in spiritual and religious beliefs (Kim et al., Citation2019; Lee & Smith, Citation2012; Yong & McCallion, Citation2003). Korean American caregivers reported fewer emotional and instrumental support helpers than Caucasian American caregivers but more than South Korean caregivers (Chun et al., Citation2007). Two studies found that caregivers with higher levels of social support found more meaning in caregiving (Lee & Bronstein, Citation2010; Lee & Choi, Citation2013). Greater emotional support was associated with reduced anxiety (Chun et al., Citation2007). Satisfaction with available social support significantly influenced attitudes toward caregiving while the size of the support network did not (Yong & McCallion, Citation2003).
Three studies mentioned the use of support groups among ADRD caregivers who found sharing caregiving experiences with groups helped them gain essential knowledge and emotional support (Kim et al., Citation2019; Lee & Smith, Citation2012; Lee & Yim, Citation2013). Moreover, one study examined post-caregivers’ experiences and their perceptions of making meaning in caregiving (Kim, Citation2009). The participants provided emotional support and shared caregiving experiences with fellow caregivers to find meaning in the hardships they had faced while being an ADRD caregiver (Kim, Citation2009).
Discussion
This scoping review provides a unique overview of the knowledge, attitudes, and experiences of Korean American caregivers by examining 17 quantitative and qualitative studies about dementia caregiving. We also sought to identify clinical, research, and policy implications such as developing and improving culturally/linguistically appropriate caregiving programs for Korean American dementia caregivers. The caregivers in the selected studies were mostly immigrants and wives/daughters/daughters-in-law.
Two major themes were identified among the studies included in this review. The first theme that emerged from our scoping review was how Korean American dementia caregivers perceived their caregiving experiences. Korean American caregivers reported poor mental health and burden. Social support and familism were found to be two of the most important factors that determine Korean American caregivers’ attitudes toward caregiving. The other major theme was related to how Korean American caregivers perceived their caregiving support services. Various factors shape Korean Americans’ underutilization of ADRD and related services: those most reported include the lack of culturally and linguistically appropriate services and the desire to care for their care recipients at home. For instance, discrepancies in foods, bathing tendencies, sleeping behaviors, and language or negative perceptions about nursing homes in Korean culture could hinder patients from utilizing available domestic services.
Strategies to combat caregiving burden were identified as having a strong social network and social support. Similar to Korean American counterparts, spouse dementia caregivers in South Korea have also reported the notable influence that social network and support play in reducing the mental burden (symptoms of depression) associated with dementia caregiving (Kim, De Bellis, & Xiao, Citation2018). In South Korea, the absence of informal support for daughters-in-law were associated with the highest rates of caregiving burden when caring for a PWD (Kim, Lee, Shin, & Park, Citation2017). Lack of social networking has also been found to have a significant association with negative mental health effects of spouse cognitive impairment (Kim et al., Citation2017). The protective effects of social networking should be stressed early on to more vulnerable caregivers (e.g., daughters-in-law) and earlier in adulthood. When considering caregiving-related education or resource allocation, it is especially important to consider differences in family structure and the impact of gender in South Korean vs. Western Korean American families.
Other resources that may provide relief for caregivers include linking clinical practice and community-based service for Korean American dementia family caregivers. Korean American dementia family caregivers’ unique needs and well-being are often ignored and are not routinely assessed. An assessment of any disparities in dementia care will improve engagement between clinical practices (i.e., primary care clinics, dementia, and memory clinics, etc.) and Korean American serving community organizations to meet the unmet needs. Unmet needs may include referrals to receive culturally and linguistically tailored resources/support/programs; to improve delivery of dementia care; and, to support informed decisions made by Korean American dementia family caregivers.
Future research implications
All of the papers were cross-sectional surveys or qualitative studies; hence, none of the papers included intervention research. We recommend that such future intervention research involve collaborations with community partners and consider incorporating “best practices” and new technologies from programs in South Korea. As a part of implementation research, dementia case management should be offered to Korean American dementia family caregivers. Although this service is the most frequently performed intervention for dementia family caregivers, it is far less frequently offered to or utilized by Korean American dementia family caregivers due to cultural and linguistic barriers (Chu, Edwards, Levin, & Thomson, Citation2000; Corvol et al., Citation2017; Francke et al., Citation2017; Khanassov & Vedel, Citation2016; Pimouguet, Lavaud, Dartigues, & Helmer, Citation2010; Somme et al., Citation2012). In addition, developing, testing, and implementing specific types of interventions for specific groups of Korean American family caregivers would be beneficial (e.g., new to dementia family caregiving, late-stage care interventions, respite care, etc.).
Research has indicated the appropriateness and effectiveness of cognitive-behavioral therapies (CBT) and principles for Asian Americans (Iwamasa & Sorocco, Citation2007), but dementia caregiving intervention research with Korean American dementia caregivers are limited. A potential approach to help address this research gap is to culturally tailor an evidence-based CBT dementia caregiving intervention by Gallagher-Thompson et al.’s which have been culturally tailored for Chinese Americans (Gallagher-Thompson et al., Citation2007) and Vietnamese Americans (Ta Park et al., Citation2018; Citation2019; Citation2019). These studies reported improvement in caregiver outcomes and acceptability of the programs.
Policy implications
These findings emphasize the urgent need to develop culturally responsive care for Korean American families. This would include implementing policy changes to mandate the recruitment and training of more bilingual and bicultural Korean health and social service providers. The Healthy People 2030, which establishes the national objectives to improve health and well-being over the next decade, recognizes that language-concordant care improves a variety of health outcomes (Diamond, Izquierdo, Canfield, Matsoukas, & Gany, Citation2019). Hence, a Healthy People 2030 objective (in development) is to “increase the proportion of limited English proficient (LEP) adults who report that their doctors or other health providers always explained things in a way that was easy to understand” (US Department of Health and Human Services, Citation2022).
Potential policy implications may target the needs of Korean American female dementia caregivers since this review found that caregivers tend to be female family members which is similar in South Korea (Jang & Baik, Citation2019; Jang, Avendano, & Kawachi, Citation2012; Jang & Kawachi, Citation2019). In addition, currently, several government programs are available for family members to get paid but such policies are not available across states and may not be available to family members who live with the care recipients (USAGov, Citation2021). In contrast, in South Korea, in 2008, the government subsidized family-care workers, which allowed older patients to be cared for at home by family members (Kim et al., Citation2018). Kim et al. examined the paid family care workers of PWD, and found that although physical, emotional, and financial burdens that come along with caregiving were reported, factors such as financial subsidies, social support, filial piety, and religion encouraged the caregivers to find relief. Potential policy changes could include the implementation of a similar financially subsidized system in the US beyond the existing programs which are very limited.
Strengths and limitations
To the best of our knowledge, this scoping review paper is the first to provide a comprehensive synthesis of the existing literature about Korean American dementia caregiving. Asian American subgroups are frequently combined into a single Asian category in national health data thus conceal the distinct heterogeneity and characteristics among the subgroups (Holland & Palaniappan, Citation2012; Kanaya et al., Citation2022). A major strength of our study was providing a focused review on a single Asian subgroup that allowed us to provide a meaningful review of this topic as cultural values are critical to consider in the Korean American population. Another major strength of our paper was evaluating both quantitative and qualitative papers related to this topic.
A potential limitation may be that our search did not yield all the potential studies, however, we had two reviewers independently search five different databases to identify potential articles, then eligible articles were agreed upon. While the methodology of a scoping review is relatively recent, future research may use the findings of this scoping review paper to conduct a systematic review as a next step and potentially “confirm the relevance of inclusion criteria and potential questions” (pp. 1) (Munn et al., Citation2018).
Conclusions
Given the dementia caregivers’ important roles for PWD, the development and provision of dementia caregiving programs and interventions are necessary. Research has shown that interventions that have the family caregivers’ active involvement, are flexible and adjustable during the disease progression, and the dual engagement of both caregivers and PWD have shown beneficial effects in relieving the caregiving-related physical and emotional stress (Gitlin, Marx, Stanley, & Hodgson, Citation2015). To ensure the successful implementation of an intervention program, including clinical programs, in diverse communities, culturally appropriate approaches are needed (Fauth et al., Citation2019; Gitlin et al., Citation2015; Zarit, Lee, Barrineau, Whitlatch, & Femia, Citation2013).
Clinical implications
Health care providers should more carefully assess caregiver burden and emotional distress of Korean American dementia caregivers in considering their culture of filial piety and familism.
Routine family meetings with Korean American dementia caregivers and health care providers may be needed to discuss progression of dementia, care of PWD, and culturally relevant resources.
Culturally and linguistically appropriate support groups and community services should be referred for Korean American dementia caregivers. Home care services may benefit Korean American caregivers who desire to take care of their PWD at home.
Acknowledgments
We would like to acknowledge Dr. Marian Tzuang for her assistance with the manuscript review.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- AARP Public Policy Institute. (2020). The “typical” Asian caregiver. Retrieved February 3 from https://www.aarp.org/content/dam/aarp/ppi/2020/05/asian-caregiver.doi.10.26419-2Fppi.00103.007.pdf
- Alzheimer’s Association. (2020). 2020 Alzheimer’s disease facts and figures. Retrieved from https://www.alz.org/aaic/downloads2020/2020_Facts_and_Figures_Fact_Sheet.pdf
- Alzheimer’s Association. (2021). 2021 Alzheimer’s disease facts and figures. Retrieved from https://www.alz.org/media/Documents/alzheimers-facts-and-figures.pdf
- Alzheimer’s Association. (2022). What is dementia? Retrieved from https://www.alz.org/alzheimers-dementia/what-is-dementia
- Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. doi:10.1080/1364557032000119616
- Budiman, A. (2021). Koreans in the U.S. fact sheet. Pew Research Center. Retrieved from https://www.pewresearch.org/social-trends/fact-sheet/asian-americans-koreans-in-the-u-s/.
- Casado, B. L., Hong, M., & Lee, S. E. (2018). Attitudes toward Alzheimer’s care-seeking among Korean Americans: Effects of knowledge, stigma, and subjective norm. Gerontologist, 58(2), e25–e34. doi:10.1093/geront/gnw253
- Chu, P., Edwards, J., Levin, R., & Thomson, J. (2000). The use of clinical case management for early stage Alzheimer’s patients and their families. American Journal of Alzheimer’s Disease and Other Dementias, 15(5), 284–290. doi:10.1177/153331750001500506
- Chun, M., Knight, B. G., & Youn, G. (2007). Differences in stress and coping models of emotional distress among Korean, Korean-American and White-American caregivers. Aging & Mental Health, 11(1), 20–29. doi:10.1080/13607860600736232
- Corvol, A., Dreier, A., Prudhomm, J., Thyrian, J. R., Hoffmann, W., & Somme, D. (2017). Consequences of clinical case management for caregivers: A systematic review. International Journal of Geriatric Psychiatry, 32(5), 473–483. doi:10.1002/gps.4679
- Covidence systematic review software. (Nodate). Veritas health innovation www.covidence.org
- Diamond, L., Izquierdo, K., Canfield, D., Matsoukas, K., & Gany, F. (2019). A systematic review of the impact of patient-physician non-english language concordance on quality of care and outcomes. Journal of General Internal Medicine, 34(8), 1591–1606. doi:10.1007/s11606-019-04847-5
- Fauth, E. B., Jackson, M. A., Walberg, D. K., Lee, N. E., Easom, L. R., Alston, G., … Mittelman, M. (2019). External validity of the New York University caregiver intervention: Key caregiver outcomes across multiple demonstration projects. Journal of Applied Gerontology, 38(9), 1253–1281. doi:10.1177/0733464817714564
- Francke, A. L., Verkaik, R., Peeters, J. M., Spreeuwenberg, P., de Lange, J., & Pot, A. M. (2017). Dementia case management through the eyes of informal carers: A national evaluation study. Dementia (London), 16(5), 642–655. doi:10.1177/1471301215614165
- Gallagher-Thompson, D., Gray, H. L., Tang, P. C., Pu, C. Y., Leung, L. Y., Wang, P. C., … Thompson, L. W. (2007). Impact of in-home behavioral management versus telephone support to reduce depressive symptoms and perceived stress in Chinese caregivers: Results of a pilot study [comparative study randomized controlled trial research support, Non-U.S. Gov’t]. The American Journal of Geriatric Psychiatry, 15(5), 425–434. doi:10.1097/JGP.0b013e3180312028
- Gitlin, L. N., Marx, K., Stanley, I. H., & Hodgson, N. (2015). Translating evidence-based dementia caregiving interventions into practice: State-of-the-science and next steps. The Gerontologist, 55(2), 210–226. doi:10.1093/geront/gnu123
- Glaser, B., & Strauss, A. (1967). The discovery of grounded theory: Strategies for qualitative research. New York: Aldine.
- Holland, A. T., & Palaniappan, L. P. (2012). Problems with the collection and interpretation of Asian-American health data: Omission, aggregation, and extrapolation. Annals of Epidemiology, 22(6), 397–405. doi:10.1016/j.annepidem.2012.04.001
- Iwamasa, G., & Sorocco, K. (2007). The psychology of Asian American older adults. In F. T. Leong, A. Inman, A. Ebreo, L. H. Yang, L. Kinoshita, & M. Fu (Eds.), Handbook of Asian American psychology (Second ed.). Thousand Oaks, CA: Sage.
- Jang, S. N., Avendano, M., & Kawachi, I. (2012). Informal caregiving patterns in Korea and European countries: A cross-national comparison. Asian Nursing Research, 6(1), 19–26. doi:10.1016/j.anr.2012.02.002
- Jang, S., & Baik, K. (2019). Disparity in caregiving and family caregiving issue. Seoul, South Korea: I. f. S. Health.
- Jang, S. N., & Kawachi, I. (2019). Care inequality: Care received according to gender, marital status, and socioeconomic status among Korean older adults with disability. International Journal for Equity in Health, 18(1), 105. doi:10.1186/s12939-019-1008-0
- Jang, Y., & Kim, M. T. (2019). Limited English proficiency and health service use in Asian Americans. Journal of Immigrant and Minority Health, 21(2), 264–270. doi:10.1007/s10903-018-0763-0
- Jang, Y., Kim, G., Chiriboga, D., & Kallimanis, B. (2007). A bidimensional model of acculturation for Korean American older adults. Journal of Aging Studies, 21(3), 267–275. doi:10.1016/j.jaging.2006.10.004
- Jang, Y., Yoon, H., Park, N. S., Rhee, M. K., & Chiriboga, D. A. (2018). Asian Americans’ concerns and plans about Alzheimer’s disease: The role of exposure, literacy and cultural beliefs. Health & Social Care in the Community, 26(2), 199–206. doi:10.1111/hsc.12509
- Jones, R. W., Lebrec, J., Kahle-Wrobleski, K., Dell’Agnello, G., Bruno, G., Vellas, B., … Reed, C. (2017). Disease progression in mild dementia due to Alzheimer disease in an 18-month observational study (GERAS): The impact on costs and caregiver outcomes. Dementia and Geriatric Cognitive Disorders Extra, 7(1), 87–100. doi:10.1159/000461577
- Kanaya, A. M., Hsing, A. W., Panapasa, S. V., Kandula, N. R., Mr, G. A., Shimbo, D., … Hong, Y. (2022). Knowledge gaps, challenges, and opportunities in health and prevention research for Asian Americans, Native Hawaiians, and Pacific Islanders: A report from the 2021 national institutes of health workshop. Annals of Internal Medicine, 175(4), 574–589. doi:10.7326/M21-3729
- Kasper, J. D., Freedman, V. A., Spillman, B. C., & Wolff, J. L. (2015). The disproportionate impact of dementia on family and unpaid caregiving to older adults. Health Affairs, 34(10), 1642–1649. doi:10.1377/hlthaff.2015.0536
- Khanassov, V., & Vedel, I. (2016). Family physician-case manager collaboration and needs of patients with dementia and their caregivers: A systematic mixed studies review. The Annals of Family Medicine, 14(2), 166–177. doi:10.1370/afm.1898
- Kim, Y. (2009). Korean American family postcaregivers on dementia caregiving: A phenomenological inquiry. Journal of Gerontological Social Work, 52(6), 600–617. doi:10.1080/01634370903048352
- Kim, J., De Bellis, A. M., & Xiao, L. D. (2018). The experience of paid family-care workers of people with dementia in South Korea. Asian Nursing Research, 12(1), 34–41. doi:10.1016/j.anr.2018.01.002
- Kim, H. J., Kehoe, P., Gibbs, L. M., & Lee, J. A. (2019). Caregiving experience of dementia among Korean American family caregivers. Issues in Mental Health Nursing, 40(2), 158–165. doi:10.1080/01612840.2018.1534909
- Kim, W., Lee, T. H., Shin, J., & Park, E. C. (2017). Depressive symptoms in spouse caregivers of dementia patients: A longitudinal study in South Korea. Geriatrics & Gerontology International, 17(6), 973–983. doi:10.1111/ggi.12820
- Kong, E. H., Deatrick, J. A., & Evans, L. K. (2010). The experiences of Korean immigrant caregivers of non-English-speaking older relatives with dementia in American nursing homes. Qualitative Health Research, 20(3), 319–329. doi:10.1177/1049732309354279
- Lee, Y., & Bronstein, L. R. (2010). When do Korean-American dementia caregivers find meaning in caregiving?: The role of culture and differences between spouse and child caregivers. Journal of Ethnic and Cultural Diversity in Social Work, 19(1), 73–86. doi:10.1080/15313200903547756
- Lee, S. E., & Casado, B. L. (2011). Attitudes toward community services use in dementia care among Korean Americans. Clinical Gerontologist, 34(4), 271–286. doi:10.1080/07317115.2011.572536
- Lee, S. E., Casado, B. L., & Hong, M. (2018). Exploring experience and perspectives of foreign-born direct care workers in dementia care: Accounts of Korean American personal care aides caring for older Korean Americans with dementia symptoms. Dementia (London), 17(4), 423–438. doi:10.1177/1471301216647832
- Lee Casado, B., Lee, S. E., Hong, M., & Hong, S. (2015). The experience of family caregivers of older Korean Americans with dementia symptoms. Clinical Gerontologist, 38(1), 32–48. doi:10.1080/07317115.2014.970316
- Lee, Y., & Choi, S. (2013). Korean American dementia caregivers’ attitudes toward caregiving: The role of social network versus satisfaction with social support. Journal of Applied Gerontology, 32(4), 422–442. doi:10.1177/0733464811431163
- Lee, E. E., & Farran, C. J. (2004). Depression among Korean, Korean American, and Caucasian American family caregivers. Journal of Transcultural Nursing, 15(1), 18–25. doi:10.1177/1043659603260010
- Lee, J. A., Nguyen, H., Park, J., Tran, L., Nguyen, T., & Huynh, Y. (2017). Usages of computers and smartphones to develop dementia care education program for Asian American family caregivers. Healthcare Informatics Research, 23(4), 338–342. doi:10.4258/hir.2017.23.4.338
- Lee, Y., & Smith, L. (2012). Qualitative research on Korean American dementia caregivers’ perception of caregiving: Heterogeneity between spouse caregivers and child caregivers. Journal of Human Behavior in the Social Environment, 22(2), 115–129. doi:10.1080/10911359.2012.646840
- Lee, Y., & Yim, N.-Y. (2013). Korean American dementia family caregivers’ experience of a psychoeducational support group: Investigation of role of culture. Social Work With Groups, 36(1), 13–26. doi:10.1080/01609513.2012.724214
- Lehrer, B. (1996). The Korean American. New York: Chelsea House Publishers.
- Luborsky, M. R. (1994). The identification and analysis of themes and patterns. In J. G. A. Sankar (Ed.), Qualitative methods in aging research (pp. 189–210). Thousand Oaks, CA: SAGE Publications, Inc.
- McKeown, S., & Mir, Z. M. (2021). Considerations for conducting systematic reviews: Evaluating the performance of different methods for de-duplicating references. Systematic Reviews, 10(1), 38. doi:10.1186/s13643-021-01583-y
- Migration Policy Institute. (2017). Korean Immigrants in the United States. Retrieved from https://www.migrationpolicy.org/article/korean-immigrants-united-states
- Munn, Z., Peters, M. D. J., Stern, C., Tufanaru, C., McArthur, A., & Aromataris, E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18(1), 143. doi:10.1186/s12874-018-0611-x
- Nguyen, D. (2012). The effects of sociocultural factors on older Asian Americans’ access to care. Journal of Gerontological Social Work, 55(1), 55–71. doi:10.1080/01634372.2011.618525
- Oak, S., & Martin, V. (2000). American/Korean contrasts: Patterns and expectations in the US and Korea. Elizabeth, NJ: Weatherhill, Incorporated.
- Pew Research Center. (2017). Key findings about U.S. immigrants. Author. Retrieved from http://www.pewresearch.org/fact-tank/2017/05/03/key-findings-about-u-s-immigrants/
- Pimouguet, C., Lavaud, T., Dartigues, J. F., & Helmer, C. (2010). Dementia case management effectiveness on health care costs and resource utilization: A systematic review of randomized controlled trials. The Journal of Nutrition, Health & Aging, 14(8), 669–676. doi:10.1007/s12603-010-0314-4
- Richardson, V. E., Fields, N., Won, S., Bradley, E., Gibson, A., Rivera, G., & Holmes, S. D. (2019). At the intersection of culture: Ethnically diverse dementia caregivers’ service use. Dementia, 18(5), 1790–1809. doi:10.1177/1471301217721304
- Somme, D., Trouve, H., Drame, M., Gagnon, D., Couturier, Y., & Saint-Jean, O. (2012). Analysis of case management programs for patients with dementia: A systematic review. Alzheimer’s & Dementia, 8(5), 426–436. doi:10.1016/j.jalz.2011.06.004
- Ta Park, V., Nguyen, K., Tran, Y., Yeo, G., Tiet, Q., Suen, J., & Gallagher-Thompson, D. (2018). Perspectives and insights from Vietnamese American mental health professionals on how to culturally tailor a Vietnamese dementia caregiving program. Clinical Gerontologist, 41(3), 184–199. doi:10.1080/07317115.2018.1432734
- Ta Park, V. M., Ton, V., Tiet, Q. Q., Vuong, Q., Yeo, G., & Gallagher-Thompson, D. (2019). Promising results from a pilot study to reduce distress in Vietnamese American dementia and memory loss caregivers. Alzheimer’s & Dementia: Translational Research & Clinical Interventions, 5(1), 319–327. doi:10.1016/j.trci.2019.05.006
- Ta Park, V. M., Ton, V., Yeo, G., Tiet, Q. Q., Vuong, Q., & Gallagher-Thompson, D. (2019). Vietnamese American dementia caregivers’ perceptions and experiences of a culturally tailored, evidence-based program to reduce stress and depression. Journal of Gerontological Nursing, 45(9), 39–50. doi:10.3928/00989134-20190813-05
- Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., … Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. doi:10.7326/M18-0850
- USAGov. (2021). Caregiver Support. Retrieved February 18 from https://www.usa.gov/disability-caregiver
- US Department of Health and Human Services. (2022). Increase the proportion of adults with limited English proficiency who say their providers explain things clearly — HC/HIT‑D11. Retrieved July 28, 2022 from https://health.gov/healthypeople/objectives-and-data/browse-objectives/health-communication/increase-proportion-adults-limited-english-proficiency-who-say-their-providers-explain-things-clearly-hchit-d11
- Yong, F., & McCallion, P. (2003). Hwabyung as caregiving stress among Korean-American caregivers of a relative with dementia. Journal of Gerontological Social Work, 42(2), 3–19. doi:10.1300/J083v42n02_02
- Zarit, S. H., Lee, J. E., Barrineau, M. J., Whitlatch, C. J., & Femia, E. E. (2013). Fidelity and acceptability of an adaptive intervention for caregivers: An exploratory study. Aging & Mental Health, 17(2), 197–206. doi:10.1080/13607863.2012.717252