Abstract
This review summarizes the evidence of bereavement groups for symptoms of grief and depression. The literature search using Web of Science, EBSCO, PubMed, CINAHL, and MEDLINE yielded 14 studies (N = 1519) meeting the inclusion criteria (i.e., randomized-controlled trials, bereaved adults, bereavement group, validated measures). Overall, bereavement groups were marginally more effective than control groups post-treatment (gG = 0.33, gD = 0.22) but not at follow-up. Although tertiary interventions yielded larger effect sizes than secondary interventions, the difference was not significant. The results imply that the evidence for bereavement groups is weak, although the large heterogeneity of concepts for intervention and control groups limits the generalizability.
The death of a loved one is a universal and also one of the most stressful experiences in life (Zisook et al., Citation2014). Although the majority of mourners are able to cope effectively with their loss over time, about 10% of mourners, with a range between 6.7 and 49%, depending on the time of loss and cause of death, develop symptoms of prolonged grief disorder (Djelantik et al., Citation2020; Kersting et al., Citation2011; Lundorff et al., Citation2017). Prolonged grief disorder (PGD) is characterized by norm exceeding levels of separation distress (longing for or preoccupation with the deceased) and intense emotional pain (e.g., anger, denial, difficulty engaging with activities) at least six months after the death (World Health Organization, Citation2018). However, most mourners with PGD do not seek or obtain adequate support. Some studies show that only about 43% of bereaved caregivers suffering from PGD actively take advantage of professional bereavement services (Lichtenthal et al., Citation2011). Further, 76% of suicide bereaved people with or without PGD report that they did not receive formal (psychological intervention, peer bereavement groups) or informal (family, friends) assistance. These self-report data suggest that mourners might be generally less likely to receive informal support than those bereaved by other causes of death (e.g., Pitman et al., Citation2014).
Those who seek professional help during their grief process can choose between a wide range of support options; for example, grief counseling, individual or group psychotherapy, bereavement groups guided by professionals of the health system, or self-help bereavement groups. Generally, bereavement groups are one of the most common types of professional grief support (Field et al., Citation2004). It is worth mentioning, though, that the term “bereavement group” is not consistently used in the literature. While the term “bereavement group therapy” generally implies the treatment and reduction of behavioral and mental disorders (i.e., pathological levels of grief), the terms “bereavement support groups” or “bereavement groups” might primarily offer emotional and social support, provide information, or facilitate exchange for all mourners (Worden, Citation2018). To our knowledge, there is still no systematic review that explicitly addresses the efficacy of treating grief and grief-related symptoms in a group setting. For these reasons, the present study summarizes the current state of literature specifically on “bereavement groups”, referring to both secondary interventions (i.e., including all bereaved people) or tertiary interventions (i.e., including severe psychopathology such as PGD).
Bereavement groups
Receiving low social support is a risk factor in developing PGD (Burke & Neimeyer, Citation2013). Hence, providing adequate support is important to prevent symptom worsening, and bereavement groups in particular seem to be suited to help avoid social isolation (Vlasto, Citation2010). One of the main advantages of bereavement groups is that they offer members a sense of community and include role models for overcoming difficulties similar to one’s own.
Qualitative research suggests a number of potential effective mechanisms in bereavement groups, although the literature is not yet unambiguous regarding differences between normal grief and PGD. For example, Vlasto (Citation2010) report that bereaved people who had sought therapy valued the “social nature of the group experience” (p. 62) through opportunities to share their feelings and worries as consequences of their grief. Further advantages are the development of hope or coping strategies, normalization of grief reactions, and social support for dealing with difficult social interactions after the loss. Disadvantages of bereavement groups can be the development of unhelpful group dynamics (e.g., jealousy) as well as behaviors of withholding feelings or tabooed thoughts, and competitive expressions. Another adverse reaction to bereavement groups can be an increased distress by listening to others’ stories of loss. Dyregrov et al. (Citation2014) conclude that many negative responses to bereavement groups might be prevented by means of thorough planning, including a screening for and the provision of specialized treatments in case of complicated forms of grief processes. Further, the authors recommended closed and homogenous groups (e.g., suicide bereavement, grieving parents) to enhance positive outcomes.
In recent years, quantitative research increasingly aimed to develop empirically based group therapies for PGD or high-risk samples in particular. For example, they translated established approaches from individual psychotherapy for PGD to the group setting (i.e., cognitive behavioral group therapy [CBT]; Boelen et al., Citation2007) or from face-to-face settings to online group settings (Wagner et al., Citation2020).
Efficacy of bereavement groups
To date, six reviews have been published on the effects of grief interventions (Allumbaugh & Hoyt, Citation1999; Currier et al., Citation2008; Johannsen et al., Citation2019; Kato & Mann, Citation1999; Schut et al., Citation2001; Wittouck et al., Citation2011). The general conclusion from these works is that secondary interventions are largely ineffective in reducing grief and that tertiary interventions yield positive but small to moderate effects. Three reviews addressed bereavement groups in particular (Allumbaugh & Hoyt, Citation1999; Johannsen et al., Citation2019; Kato & Mann, Citation1999), although the information is quite limited. For example, Kato and Mann (Citation1999) report that only two of eight reviewed bereavement groups showed positive effects, that is, were more effective than waitlist control groups on diverse outcomes (e.g., grief, depression, anxiety, adjustment). In two studies, one treatment arm (i.e., a social activity group) even revealed adverse effects on depression, adjustment, and social support. Although the authors did not differentiate explicitly between secondary or tertiary interventions, the described results basically represent secondary interventions as the studies were addressed at all mourners. Allumbaugh and Hoyt (Citation1999) and Johannsen et al. (Citation2019) used delivery format as a moderator in their analyses and found that the efficacy of grief interventions increases when they are individually delivered rather than presented in a group format. While the difference was only marginally significant in the former meta-analysis, which included both participants with low and high risks of complicated grief (secondary and tertiary interventions), it was substantial in the latter review, which included RCTs only.
In sum, bereavement groups seem to be less efficient than individually delivered support; however, the methodological quality of the included studies was criticized and conclusions regarding secondary and tertiary interventions are ambiguous. In addition, no mean effect sizes for bereavement groups have been reported so far.
The current study aims to review concepts of professionally guided bereavement groups. In addition, it meta-analytically summarizes the efficacy of these groups for the reduction of symptoms of grief (primary outcome). Because PGD and depression are distinct states but both normal and pathological levels of grief are highly associated, depression was chosen as a secondary outcome (e.g., Schaal et al., Citation2014). To ensure reliable conclusions from this summary, we only include RCTs. Further, this review is not limited to PGD as defined in the ICD-11, because most studies have been published before the final criteria have been established. Thus, we include normal as well as pathological levels of grief in our analyses, knowing that there might be differences to ICD-11 PGD (Killikelly & Maercker, Citation2017). Besides overall effect sizes per outcome, we also compare the results between secondary and tertiary interventions.
Method
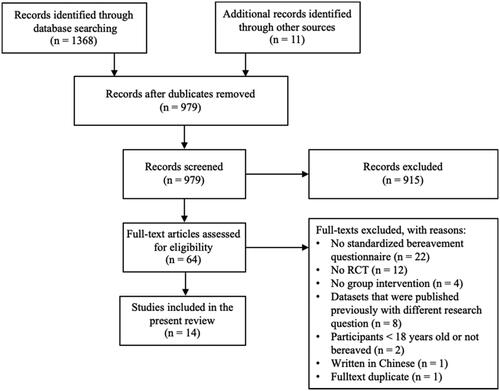
This review was registered with PROSPERO (CRD42019136033) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (PRISMA; Moher et al., Citation2009) was used.
Inclusion criteria
We included all studies that (1) were published in peer-reviewed journals, (2) were RCTs, (3) examined a bereavement group, (4) addressed adults (≥18 years old) who were bereaved by the death of a loved person, and (5) applied validated grief measurements. More precisely, we defined an examined intervention as “bereavement group” when it fulfilled the following general criteria for group interventions (Strauß & Mattke, Citation2018): (1) opportunity for direct communication, (2) a mutual goal (i.e., deal with grief), (3) a certain duration (i.e., we demanded at least three sessions), (4) at least five members (small group). In distinction to self-help groups, which are often guided by an affected person, the bereavement group should be led by a professional within the health system (e.g., therapist, counsellor). We excluded studies that (1) used computer- or online-based bereavement groups, (2) used family-based interventions, and (3) studied grief not resulting from the death of a person (e.g., divorce, loss of a pet or occupation).
Search strategy
The data collection was completed in December 2018 (JP) and updated in September 2019 (UM, JP). The databases EBSCO, PubMed, Web of Science, CINAHL Complete, and MEDLINE Complete were searched using the search strings: grief or bereavement or bereaved or “bereavement group” or “grief group” or “group therapy” or “group intervention” or “group work” or “support group” or “mutual group” or “group counseling” or “self-help group” or “group program” and “control” or “random “(see Supplement 1 for the full research strategy in PICOS terms). At first, the titles and abstracts were scanned for suitability, and then the full texts were scanned. In addition, the reference lists of relevant studies were screened. The interrater reliability was calculated for the full text screening of the updated search before inconsistencies were resolved in mutual discussions. Cohen’s kappa was interpreted as “fair” (0.40–0.59), “good” (0.60–0.74), and “excellent” (≥0.75; Orwin, Citation1994).
Methodological quality and data extraction
The quality rating of (Van Tulder et al., Citation2003) was used to assess the methodological quality of the included studies, because it is based on recommendations by the Cochrane Collaboration Back Review Group (rating scale: yes, no, or unclear) and is less time-consuming. We removed one item (blind outcome assessor) because it is not suitable for the included studies. This results in twelve methodological criteria and a sum score of at least nine was considered representing good quality (van den Berg et al., Citation2007). In addition, two authors (JP, UM) extracted the following information: study characteristics (i.e., author(s), year of publication, number of sessions and group members, duration of treatment, use of protocol, leader information, grief level, randomized sample size, dropout rate, intent-to-treat analysis, follow-up interval), sample characteristics (i.e., age, gender, kinship to deceased, cause of death, time since loss), and intervention content. The grief level and thereby the decision whether a bereavement group was classified as secondary or tertiary intervention was based on the methods description in the original study. That is, it was considered to be tertiary when the authors described according eligibility criteria and used measurements for prolonged grief symptoms. Descriptive statistics were extracted based on the studies’ intention to treat (ITT) data or per protocol (PP) data when ITT data were not reported. In case of dissent during the extraction process, the results were discussed and resolved, or BW was consulted.
Meta-analytical approach
The meta-analyses were executed using RStudio 1.1.456 (RStudio Team, Citation2016) and the metafor package (Viechtbauer, Citation2010). We conducted the analyses as between-group comparisons between the intervention and control groups from pre to post assessment and from pre to follow-up assessments. In addition, we conducted subgroup analyses (secondary vs. tertiary interventions) using random effects models for each subgroup and fixed effects models to test for significance between both subgroups (Viechtbauer, Citation2010). When studies reported several follow-up assessments, we focused on the longest interval (Cochrane Handbook, Citation2011). When the included studies reported multiple measurements for one outcome or multiple subgroups that are compared with the same control group, we combined the ESs, because the outcomes were based on the same participants and would thus produce dependencies within the data (Borenstein et al., Citation2011). Further, Hedge’s g was used as the standardized mean difference, interpreting it as small (g < 0.50), moderate (0.50 ≤ g ≤ 0.80), or large (g > 0.80; Cohen, Citation1988). To meta-analytically summarize Hedge’s g and its variance, we followed the procedure suggested by Borenstein et al. (Citation2011) as well as Morris (Citation2008; as cited by Viechtbauer), which computes the effect sizes particularly for pre-post control group designs using pre-post correlations and random-effects models. Because most studies did not provide pre-post correlations, we assumed a correlation of r = .50 and conducted sensitivity analyses using r = 0.30 and r = 0.70 to test for the robustness of the results. Publication bias was inspected with the Egger’s regression test (Egger et al., Citation1997) for analyses including more than nine studies (Cochrane Handbook, Citation2011). Potential outliers for both outcomes were detected using influential case diagnostics. Heterogeneity was examined using the Q-statistic and the I2 index, which point to low (25%), moderate (50%), or high (75%) levels (Crombie & Davies, Citation2009).
Results
displays the process of the literature search and study selection. Interrater reliability was excellent for the full text screening (κ = 1.00). This review included 14 data sets (Chow et al., Citation2019; Constantino & Bricker, Citation1996; Foster & Holden, Citation2014; Goodkin et al., Citation1999; Johnson et al., Citation2016; MacKinnon et al., Citation2015; McGuinness et al., Citation2015; Murphy et al., Citation1998; Piper et al., Citation2001, Citation2007; Rosner et al., Citation2011; Sikkema et al., Citation2004; Supiano & Luptak, Citation2014; Wenn et al., Citation2019).
Methodical quality
Of the 14 studies included in the review, five (36%; Chow et al., Citation2019; Johnson et al., Citation2016; MacKinnon et al., Citation2015; Supiano & Luptak, Citation2014; Wenn et al., Citation2019) were judged to be of good quality with a score of nine or more (Supplement 2). It is noteworthy that only few studies provided unambiguous information on their randomization procedures. For example, three studies (21%) did not display the sample sizes for each study group after randomization (Piper et al., Citation2001; Rosner et al., Citation2011; Sikkema et al., Citation2004). Further, the study by Rosner et al. (Citation2011) used a pseudo-randomization (participants from a first time period of registrations were assigned to control and participants from a second time period to the treatment condition). Similarly, only half of the participants in Piper et al. (Citation2007) were randomly assigned to the study groups. In most studies, the baseline scores between the study groups were comparable. However, in one study (Constantino & Bricker, Citation1996) the control group had significantly higher scores of anxiety, death anxiety and social adjustment. Three studies (21%) did not describe in which way treatment adherence or compliance with the intervention was addressed (Foster & Holden, Citation2014; McGuinness et al., Citation2015; Rosner et al., Citation2011). Seven studies (50%) used intention-to-treat analyses (ITT; i.e., last observation carried forward method, expectation-maximization algorithms, hierarchical linear models), whereby one study did not describe the ITT method (Wenn et al., Citation2019).
Study, sample, and intervention characteristics
and Supplement 3 present an overview of the study and sample characteristics. Half of the studies examined normal grief and, thus, were considered secondary interventions. Six studies focused on pathological grief and were considered tertiary interventions. One study could not be classified unambiguously (Johnson et al., Citation2016). The average bereavement group had ten sessions (Range: 3–16) and lasted ten weeks (Range: 3–20). Each group session lasted between 90 and 120 min. Four studies (29%) indicated their group sizes with a maximum of ten participants. There was much variety in the occupational background of the group leaders, ranging from mental health nurses, psychologists, researchers, psychotherapists, social workers, to counselors. Most studies (k = 11, 79%) used a treatment protocol. Although six studies (43%) assessed participants at follow-up (Range: 1.5–6), only four studies (29%) reported separate data for the treatment and control group (Chow et al., Citation2019; MacKinnon et al., Citation2015; Murphy et al., Citation1998; Supiano & Luptak, Citation2014). The average dropout rate in the treatment group (i.e., the proportion of all randomized participants in the treatment group who did not complete treatment; irrespective of ITT-analyses or the completion of outcome assessments) was 22.5% (Range: 0–56%). However, it has to be considered that not all studies provided unambiguous information on the number of those completing treatment or used different definitions of completion.
Table 1. Study characteristics.
A total of 1519 (Range: 20–268) randomized subjects were studied in the trials. On average, participants were 48 years old (Range: 30–74), 74% female (Range: 0–100%), 72% Caucasians and had lost someone 2.5 years ago (Range: 0.2–9). Half of the bereavement groups were heterogenous with respect to the kinship of the deceased (Foster & Holden, Citation2014; Goodkin et al., Citation1999; McGuinness et al., Citation2015; Piper et al., Citation2001, Citation2007; Supiano & Luptak, Citation2014; Wenn et al., Citation2019), and four (29%) concentrated solely on partners or parents (Chow et al., Citation2019; Constantino & Bricker, Citation1996; Johnson et al., Citation2016; Murphy et al., Citation1998). Five studies (36%) included heterogenous causes of death (Chow et al., Citation2019; Johnson et al., Citation2016; Murphy et al., Citation1998; Supiano & Luptak, Citation2014; Wenn et al., Citation2019), whereas three studies (21%) focused on bereavement by suicide or AIDS (Constantino & Bricker, Citation1996; Goodkin et al., Citation1999; Sikkema et al., Citation2004). Six studies (43%) did not indicate the cause of death (Foster & Holden, Citation2014; MacKinnon et al., Citation2015; McGuinness et al., Citation2015; Piper et al., Citation2001, Citation2007; Rosner et al., Citation2011).
Supplement 4 summarizes the concepts of the treatment and control groups. Eleven studies (79%) labeled their groups “therapy” or “intervention” (Chow et al., Citation2019; Foster & Holden, Citation2014; Goodkin et al., Citation1999; Johnson et al., Citation2016; Murphy et al., Citation1998; Piper et al., Citation2001, Citation2007; Rosner et al., Citation2011; Sikkema et al., Citation2004; Supiano & Luptak, Citation2014; Wenn et al., Citation2019), although only six of them were addressed at prolonged grief; further terms were “nursing postvention” (Constantino & Bricker, Citation1996), “group counseling” (MacKinnon et al., Citation2015), or “bereavement support group” (McGuinness et al., Citation2015). Five (36%) studies described their concepts to be based on support group principles (Constantino & Bricker, Citation1996; Foster & Holden, Citation2014; Goodkin et al., Citation1999; McGuinness et al., Citation2015; Murphy et al., Citation1998), three studies (21%) described their treatment concepts as being based on CBT principles (Rosner et al., Citation2011; Sikkema et al., Citation2004; Supiano & Luptak, Citation2014), two studies (14%) applied interpretive therapy (IT; Piper et al., Citation2001, Citation2007), and one study (7%) each offered metacognitive grief therapy (MCGT; Wenn et al., Citation2019), interpersonal psychotherapy (IPT; Johnson et al., Citation2016), meaning-based group counseling (MBGC; MacKinnon et al., Citation2015), or a dual-process bereavement group intervention (DPBGI; Chow et al., Citation2019).
Four studies (29%) applied waiting list control groups (Foster & Holden, Citation2014; McGuinness et al., Citation2015; Murphy et al., Citation1998; Wenn et al., Citation2019) and were considered as passive control groups. Ten studies (71%) were categorized as active control groups (Chow et al., Citation2019; Constantino & Bricker, Citation1996; Goodkin et al., Citation1999; Johnson et al., Citation2016; MacKinnon et al., Citation2015; Piper et al., Citation2001, Citation2007; Rosner et al., Citation2011; Sikkema et al., Citation2004; Supiano & Luptak, Citation2014). From these studies, four (29%) compared their intervention with another psychological bereavement group (i.e., Social Group Postvention, two Supportive Therapies, Coping with Depression Program; Constantino & Bricker, Citation1996; Johnson et al., Citation2016; Piper et al., Citation2001, Citation2007) and six studies (43%) used treatment as usual (TAU; Chow et al., Citation2019; Goodkin et al., Citation1999; MacKinnon et al., Citation2015; Rosner et al., Citation2011; Sikkema et al., Citation2004; Supiano & Luptak, Citation2014). However, what constituted TAU differed from study to study (i.e., three support groups, individual treatment on request, standard inpatient care, continuation of former treatment).
Effect sizes
Supplement 5 gives an overview on the studies providing sufficient statistics to be contributing to the comparisons in the following meta-analyses. The comparison between all treatment groups to control groups from pre to post yielded small effect sizes for grief and depression (). Egger’s Tests showed no evidence for publication bias for grief, z = 1.63, p = 0.104, and depression, z = 0.27, p = 0.784. Two studies were identified as influencing the grief effect size (Rosner et al., Citation2011; Wenn et al., Citation2019; Supplement 6). A re-analysis reduced heterogeneity and the effect size, k = 9, Hedge’s ggrief = 0.19, 95% CI [0.02, 0.35], p = 0.027, I2 = 0.0%, Q(8) = 3.4, p = 0.907.
Figure 2. Forest plots for between-subject comparisons: treatment versus control group from pre- to post-intervention.
n: sample size at post assessment. Pre: mean at pre-assessment. Post: mean at post-assessment.
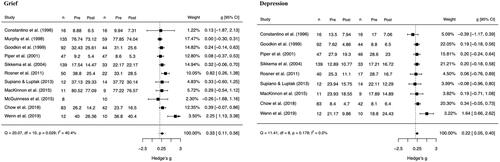
The comparisons from pre to follow-up assessments were statistically nonsignificant for grief, k = 4, Hedge’s gGrief = 0.20, 95% CI [−0.35, 0.75], p = 0.483, I2 = 71.6%, Q(3) = 9.0, p = 0.030, and depression, k = 3, Hedge’s gDepression = 0.22, 95% CI [−0.11, 0.55], p = 0.196, I2 = 0.0%, Q(2) = 0.0, p = 0.981. Two studies were identified as influencing the grief effect size (Murphy et al., Citation1998; Supiano & Luptak, Citation2014; Supplement 6). A re-analysis reduced heterogeneity and the effect size, k = 2, Hedge’s ggrief = 0.15, 95% CI [−0.24, 0.54], p = 0.454, I2 = 0.0%, Q(1) = 0.9, p = 0.331. Sensitivity analyses (Supplement 7) showed that all results did not significantly differ, assuming varying degrees of pre-post or pre-follow-up correlations.
Supplement 8 presents the results of the subgroup analyses. While secondary interventions had no significant effect on grief or depression, tertiary interventions achieved a moderate effect size (g = 0.67) for grief but a non-significant one for depression. However, the differences between secondary and tertiary interventions were not statistically significant.
Discussion
The purpose of the present review was to summarize RCTs that studied the efficacy of bereavement groups for grief and depressive symptoms in adults. The general result from this meta-analysis is that the current state of evidence on bereavement groups is rather weak, because their effects were, in comparison with control groups, only small post-treatment and non-significant at follow-up. In addition, there was no significant difference between secondary (addressing all mourners) and tertiary (addressing pathological grief levels) interventions, although the trend was that tertiary interventions achieved larger effect sizes. These results have to be interpreted with caution, because the comparisons were based on a large diversity of group concepts (i.e., various forms of support groups, CBT, IT, MBGC, IPT, DPBGI-C, MCTG), control conditions (i.e., waiting list, individual treatment, bereavement group, support group, TAU), underlying theories (e.g., Dual Process Model, Yalom’s curative factors, Transference, Theory of Shattered Assumptions, Social Learning Theory, Metacognitive Model), occupational background of the group leaders (i.e., nurse, social workers, counselors, psychologists, psychotherapists), the number of treatment sessions (i.e., 3 to 16), and methodological quality (i.e., 65% low). This is especially surprising, because Kato and Mann (Citation1999) already criticized the lack of methodically sound studies on bereavement groups, which might mask effective interventions, in their review 20 years ago.
Despite this diversity, the results are generally in line with previous meta-analyses on the efficacy of grief interventions (Johannsen et al., Citation2019; Wittouck et al., Citation2011), which also found small to moderate effects compared with control groups. However, tertiary interventions in particular have been demonstrated to be effective while secondary interventions generally yield reduced or non-significant results. Although our subgroup analyses could not confirm this difference for bereavement groups statistically, the results pointed in the same direction. One explanation might be that too few studies contributed to the subgroups, leading to a reduced power to detect such differences. Future studies might test the hypothesis that bereavement groups that are designed as tertiary interventions are more effective than secondary interventions.
Further, although sensitivity analyses indicated that the results of this review were robust, the studies of Wenn et al. (Citation2019) and Rosner et al. (Citation2011) achieved the highest effect sizes in this review and were identified as likely outliers. Since it is still not fully understood which elements of therapy are the most effective ones and, further, how they apply to the group setting, there might be several explanations for the comparably higher effect sizes. For example, both studies addressed prolonged grief and were of comparably high methodological quality. In addition, the bereavement group in Wenn et al. might be so effective because it was compared with a waiting list control group. Rosner et al. explicitly used exposure elements, which is generally seen as effective in treating PGD (Bryant et al., Citation2014). However, its transferability to the group setting seems rather difficult, which might be the reason why the authors added individual sessions. On the other hand, the treatment focus in Wenn et al. was on a detached mindfulness, which is very different from cognitive restructuring and exposure. Thus, it is still difficult to make recommendations regarding the most promising approach to bereavement groups.
It is possible that our results are somewhat biased because we excluded non-published literature. In addition, our eligibility criteria did not consider the formal training of the group leaders but included groups that were guided by non-psychologists as well as psychotherapists. One of the most striking limitations is the low quality of the included studies. Although we included solely RCTs, only one third was considered of good quality. In addition, there was a wide range of dropout rates between the studies, with up to 56% in one of largest and thus most influential studies (i.e., Sikkema et al., Citation2004). However, it should be borne in mind that our strict definition of dropouts (i.e., the non-completion of treatment after randomization to the treatment group) might have contributed to this number and that the authors did not report the exact numbers of dropouts. Unfortunately, there were only few studies available for the follow-up analyses; however, these studies were mostly of medium to high quality and incorporated a reasonable number of participants (i.e., ngrief = 359 and ndepression = 171 at follow-up assessment). Due to strict inclusion criteria, there were some studies that we could not examine. The classic study of Lieberman and Yalom (Citation1992) for example, did not use a validated measurement instrument. A study of Bryant et al. (Citation2014) that addressed PGD comparing two CBT groups needed to be excluded because some participants were below the age of 18 years. Finally, the lack of clear definitions of normal and pathological grief, which is now defined in the ICD-11, limits the generalizability of the results to samples with PGD.
We believe that the results of the current review can serve as groundwork upon which future studies might build, specify their theories and hypotheses, and develop their interventions. For example, researchers should (a) include unambiguous eligibility criteria for participants (e.g., PGD), (b) base their bereavement group concept on a clearly described theoretical framework, (c) define their bereavement groups unambiguously as secondary or tertiary interventions, (d) explain in what way established effective factors in tertiary interventions (e.g., exposure elements) are considered, (e) provide sufficient training for group leaders (i.e., ensure a psychological education in tertiary interventions), and, if an active condition is chosen, (f) state the extent both treatment and control interventions conceptually differ to be able to draw conclusions about particular intervention characteristics (i.e., What differentiates a cognitive-behavioral treatment group from a support group?). In addition, given the finding that bereavement groups might be less effective than individual therapy (Johannsen et al., Citation2019), already validated concepts for bereavement interventions in the individual setting might be compared with an application to the group setting. This might provide knowledge on the extent group factors such as the opportunity to talk to other mourners or role-plays and feedback are particularly conducive. Furthermore, there is still a lack of knowledge of the effectivity of self-help groups in which a lot of bereaved people take part. Finally, it seems advisable to include instruments that assess group processes and effective mechanisms such as group cohesion or cooperation.
Bereavement groups have the general potential to reduce grief and depression to a small degree, in comparison to control groups that wait for treatment, receive TAU or follow another treatment concept. Because the differentiation between, for example, standard bereavement support groups and bereavement group therapy was not always unambiguous, it is the task of future studies to develop evidence-based concepts. Hence, to draw reliable conclusions about the efficacy of bereavement groups, RCTs with high quality, pre-defined target interventions (i.e., secondary vs. tertiary), and clear treatment concepts for both intervention and control groups are needed.
Supplemental Material
Download MS Word (934.5 KB)Disclosure statement
All authors declare no conflict of interest.
Data availability statement
The data that support the findings of this study are openly available in Open Science Framework at https://osf.io/r3teq/?view_only=8ed697e6dec54e62a8c2f855c91dbf5e
References
- Allumbaugh, D. L., & Hoyt, W. T. (1999). Effectiveness of grief therapy: A meta-analysis. Journal of Counseling Psychology, 46(3), 370–380. https://doi.org/https://doi.org/10.1037/0022-0167.46.3.370
- Boelen, P. A., de Keijser, J., van den Hout, M. A., & van den Bout, J. (2007). Treatment of complicated grief: A comparison between cognitive-behavioral therapy and supportive counseling. Journal of Consulting and Clinical Psychology, 75(2), 277–284. https://doi.org/https://doi.org/10.1037/0022-006X.75.2.277
- Borenstein, M., Hedges, L. V., Higgins, J. P., & Rothstein, H. R. (2011). Introduction to meta-analysis. John Wiley & Sons.
- Bryant, R. A., Kenny, L., Joscelyne, A., Rawson, N., Maccallum, F., Cahill, C., Hopwood, S., Aderka, I., & Nickerson, A. (2014). Treating prolonged grief disorder: A randomized clinical trial. JAMA Psychiatry, 71(12), 1332–1339. https://doi.org/https://doi.org/10.1001/jamapsychiatry.2014.1600
- Burke, L. A., & Neimeyer, R. A. (2013). Prospective risk factors for complicated grief: A review of the empirical literature. In M. Stroebe, H. Schut, & J. van den Bout (Eds.), Complicated grief: Scientific foundations for health care professionals (pp. 145–161). Routledge/Taylor & Francis Group.
- Chow, A. Y. M., Caserta, M., Lund, D., Suen, M. H. P., Xiu, D., Chan, I. K. N., & Chu, K. S. M. (2019). Dual-process bereavement group intervention (DPBGI) for widowed older adults. The Gerontologist, 59(5), 983–994. https://doi.org/https://doi.org/10.1093/geront/gny095
- Cochrane Handbook. (2011). Cochrane handbook for systematic reviews of interventions: Vol. 5.1.0 [updated March 2011]. (J. P. T. Higgins, ed.). The Cochrane Collaboration.
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed). Lawrence Erlbaum Associates. https://doi.org/https://doi.org/10.4324/9780203771587
- Constantino, R. E., & Bricker, P. L. (1996). Nursing postvention for spousal survivors of suicide. Issues in Mental Health Nursing, 17(2), 131–152. https://doi.org/https://doi.org/10.3109/01612849609035002
- Crombie, I. K., & Davies, H. T. (2009). What is meta-analysis? http://www.bandolier.org.uk/painres/download/whatis/Meta-An.pdf
- Currier, J. M., Neimeyer, R. A., & Berman, J. S. (2008). The effectiveness of psychotherapeutic interventions for bereaved persons: A comprehensive quantitative review. Psychological Bulletin, 134(5), 648–661. https://doi.org/https://doi.org/10.1037/0033-2909.134.5.648
- Djelantik, A. M. J., Smid, G. E., Mroz, A., Kleber, R. J., & Boelen, P. A. (2020). The prevalence of prolonged grief disorder in bereaved individuals following unnatural losses: Systematic review and meta regression analysis. Journal of Affective Disorders, 265, 146–156. https://doi.org/https://doi.org/10.1016/j.jad.2020.01.034
- Dyregrov, K., Dyregrov, A., & Johnsen, I. (2014). Positive and negative experiences from grief group participation: A qualitative study. Omega, 68(1), 45–62. https://doi.org/https://doi.org/10.2190/om.68.1.c
- Egger, M., Smith, G. D., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical Research Ed.).), 315(7109), 629–634. https://doi.org/https://doi.org/10.1136/bmj.315.7109.629
- Field, D., Reid, D., Payne, S., & Relf, M. (2004). Survey of UK hospice and specialist palliative care adult bereavement services. International Journal of Palliative Nursing, 10(12), 569–576. https://doi.org/https://doi.org/10.12968/ijpn.2004.10.12.17280
- Foster, R. D., & Holden, J. M. (2014). Eternal connection: An exploratory study of the effects of learning about near-death experiences on adult grief. Journal of Loss and Trauma, 19(1), 40–55. https://doi.org/https://doi.org/10.1080/15325024.2012.735189
- Goodkin, K., Blaney, N. T., Feaster, D. J., Baldewicz, T., Burkhalter, J. E., & Leeds, B. (1999). A randomized controlled clinical trial of a bereavement support group intervention in human immunodeficiency virus type 1–seropositive and–seronegative homosexual men. Archives of General Psychiatry, 56(1), 52–59. https://doi.org/https://doi.org/10.1001/archpsyc.56.1.52
- Johannsen, M., Damholdt, M. F., Zachariae, R., Lundorff, M., Farver-Vestergaard, I., & O'Connor, M. (2019). Psychological interventions for grief in adults: A systematic review and meta-analysis of randomized controlled trials. Journal of Affective Disorders, 253, 69–86. https://doi.org/https://doi.org/10.1016/j.jad.2019.04.065
- Johnson, J. E., Price, A. B., Kao, J. C., Fernandes, K., Stout, R., Gobin, R. L., & Zlotnick, C. (2016). Interpersonal psychotherapy (IPT) for major depression following perinatal loss: A pilot randomized controlled trial. Archives of Women's Mental Health, 19(5), 845–859. https://doi.org/https://doi.org/10.1007/s00737-016-0625-5
- Kato, P., & Mann, T. (1999). A synthesis of psychological interventions for the bereaved. Clinical Psychology Review, 19(3), 275–296. https://doi.org/https://doi.org/10.1016/S0272-7358(98)00064-6
- Kersting, A., Brähler, E., Glaesmer, H., & Wagner, B. (2011). Prevalence of complicated grief in a representative population-based sample. Journal of Affective Disorders, 131(1–3), 339–343. https://doi.org/https://doi.org/10.1016/j.jad.2010.11.032
- Killikelly, C., & Maercker, A. (2017). Prolonged grief disorder for ICD-11: The primacy of clinical utility and international applicability. European Journal of Psychotraumatology, 8(Suppl 6), 1476441–1476449. https://doi.org/https://doi.org/10.1080/20008198.2018.1476441
- Lichtenthal, W. G., Nilsson, M., Kissane, D. W., Breitbart, W., Kacel, E., Jones, E. C., & Prigerson, H. G. (2011). Underutilization of mental health services among bereaved caregivers with prolonged grief disorder. Psychiatric Services (Washington, D.C.), 62(10), 1225–1229. https://doi.org/https://doi.org/10.1176/ps.62.10.pss6210_1225
- Lieberman, M. A., & Yalom, I. (1992). Brief group psychotherapy for the spousally bereaved: A controlled study. International Journal of Group Psychotherapy, 42(1), 117–132. https://doi.org/https://doi.org/10.1080/00207284.1992.11732583
- Lundorff, M., Holmgren, H., Zachariae, R., Farver-Vestergaard, I., & O'Connor, M. (2017). Prevalence of prolonged grief disorder in adult bereavement: A systematic review and meta-analysis. Journal of Affective Disorders, 212, 138–149. https://doi.org/https://doi.org/10.1016/j.jad.2017.01.030
- MacKinnon, C. J., Smith, N. G., Henry, M., Milman, E., Chochinov, H. M., Körner, A., Berish, M., Farrace, A. J., Liarikos, N., & Cohen, S. R. (2015). Reconstructing meaning with others in loss: A feasibility pilot randomized controlled trial of a bereavement group. Death Studies, 39(7), 411–421. https://doi.org/https://doi.org/10.1080/07481187.2014.958628
- McGuinness, B., Finucane, N., & Roberts, A. (2015). A hospice-based bereavement support group using creative arts: An exploratory study. Illness, Crisis & Loss, 23(4), 323–342. https://doi.org/https://doi.org/10.1177/1054137315590734
- Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & The, P. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. https://doi.org/https://doi.org/10.1371/journal.pmed.1000097
- Morris, S. B. (2008). Estimating effect sizes from pretest-posttest-control group designs. Organizational Research Methods, 11(2), 364–386. https://doi.org/https://doi.org/10.1177/1094428106291059
- Murphy, S. A., Johnson, C., Cain, K. C., Das Gupta, A., Dimond, M., Lohan, J., & Baugher, R. (1998). Broad-spectrum group treatment for parents bereaved by the violent deaths of their 12- to 28-year-old children: a randomized controlled trial. Death Studies, 22(3), 209–235. https://doi.org/https://doi.org/10.1080/074811898201560
- Orwin, R. G. (1994). Evaluating coding decisions. In H. Cooper & L. V. Hedges (Eds.), The handbook of research synthesis (pp. 139–162). Russell Sage Foundation.
- Piper, W. E., Ogrodniczuk, J. S., Azim, H. F., & Weideman, R. (2001). Prevalence of loss and complicated grief among psychiatric outpatients. Psychiatric Services (Washington, D.C.), 52(8), 1069–1074. https://doi.org/https://doi.org/10.1176/appi.ps.52.8.1069
- Piper, W. E., Ogrodniczuk, J. S., Joyce, A. S., Weideman, R., & Rosie, J. S. (2007). Group composition and group therapy for complicated grief. Journal of Consulting and Clinical Psychology, 75(1), 116–125. https://doi.org/https://doi.org/10.1037/0022-006X.75.1.116
- Pitman, A., Osborn, D., King, M., & Erlangsen, A. (2014). Effects of suicide bereavement on mental health and suicide risk. The Lancet Psychiatry, 1(1), 86–94. https://doi.org/https://doi.org/10.1016/S2215-0366(14)70224-X
- Rosner, R., Lumbeck, G., & Geissner, E. (2011). Effectiveness of an inpatient group therapy for comorbid complicated grief disorder. Psychotherapy Research: Journal of the Society for Psychotherapy Research, 21(2), 210–218. https://doi.org/https://doi.org/10.1080/10503307.2010.545839
- RStudio Team. (2016). RStudio: integrated development for RStudio, Inc. Boston, MA. http://www.rstudio.com/.
- Schaal, S., Richter, A., & Elbert, T. (2014). Prolonged grief disorder and depression in a German community sample. Death Studies, 38(6–10), 476–481. https://doi.org/https://doi.org/10.1080/07481187.2013.809032
- Schut, H., Stroebe, M. S., van den Bout, J., & Terheggen, M. (2001). The efficacy of bereavement interventions: Determining who benefits. In M. S. Stroebe, R. O. Hansson, W. Stroebe, & H. Schut (Eds.), Handbook of bereavement research: Consequences, coping, and care (pp. 705–737). American Psychological Association. https://doi.org/https://doi.org/10.1037/10436-029.
- Sikkema, K. J., Hansen, N. B., Kochman, A., Tate, D. C., & Difranceisco, W. (2004). Outcomes from a randomized controlled trial of a group intervention for HIV positive men and women coping with AIDS-related loss and bereavement. Death Studies, 28(3), 187–209. https://doi.org/https://doi.org/10.1080/07481180490276544
- Strauß, B., & Mattke, D. (Eds.). (2018). Gruppenpsychotherapie: Lehrbuch für die Praxis. Springer. https://doi.org/https://doi.org/10.1007/978-3-662-54644-4
- Supiano, K. P., & Luptak, M. (2014). Complicated grief in older adults: A randomized controlled trial of complicated grief group therapy. The Gerontologist, 54(5), 840–856. https://doi.org/https://doi.org/10.1093/geront/gnt076
- van den Berg, M. H., Schoones, J. W., & Vliet Vlieland, T. P. (2007). Internet-based physical activity interventions: A systematic review of the literature. Journal of Medical Internet Research, 9(3), e26. https://doi.org/https://doi.org/10.2196/jmir.9.3.e26
- Van Tulder, M., Furlan, A., Bombardier, C., & Bouter, L. (2003). Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine, 28(12), 1290–1299. https://doi.org/https://doi.org/10.1097/01.BRS.0000065484.95996.AF
- Viechtbauer, W. (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36(3), 1–48. https://doi.org/https://doi.org/10.18637/jss.v036.i03
- Vlasto, C. (2010). Therapists’ views of the relative benefits and pitfalls of group work and one-to-one counselling for bereavement. Counselling and Psychotherapy Research, 10(1), 60–66. https://doi.org/https://doi.org/10.1080/14733140903171220
- Wagner, B., Hofmann, L., & Maaß, U. (2020). Online-group intervention after suicide bereavement through the use of Webinars: Study protocol for a randomized controlled trial. Trials, 21(1), 45. https://doi.org/https://doi.org/10.1186/s13063-019-3891-5
- Wenn, J. A., O'Connor, M., Kane, R. T., Rees, C. S., & Breen, L. J. (2019). A pilot randomised controlled trial of metacognitive therapy for prolonged grief. BMJ Open, 9(1), e021409. https://doi.org/https://doi.org/10.1136/bmjopen-2017-021409
- Wittouck, C., Van Autreve, S., De Jaegere, E., Portzky, G., & van Heeringen, K. (2011). The prevention and treatment of complicated grief: A meta-analysis. Clinical Psychology Review, 31(1), 69–78. https://doi.org/https://doi.org/10.1016/j.cpr.2010.09.005
- Worden, J. W. (2018). Grief counseling and grief therapy (3rd ed.). Springer Publishing Company.
- World Health Organization. (2018). International classification of diseases for mortality and morbidity statistics (11th Revision). Geneva: World Health Organization. https://icd.who.int/browse11/l-m/en
- Zisook, S., Iglewicz, A., Avanzino, J., Maglione, J., Glorioso, D., Zetumer, S., Seay, K., Vahia, I., Young, I., Lebowitz, B., Pies, R., Reynolds, C., Simon, N., & Shear, M. K. (2014). Bereavement: Course, consequences, and care. Current Psychiatry Reports, 16(10), 482–492. https://doi.org/https://doi.org/10.1007/s11920-014-0482-8