Abstract
Introduction: Distal humerus intercondylar fractures are intra-articular comminuted fractures of the elbow that involve soft tissue injury. We evaluate different surgical approaches and elbow functional outcomes in the treatment of distal humerus fracture.
Materials and methods: Medline, Cochrane, EMBASE, Google Scholar databases were searched up to 29 July 2016. All studies had to have evaluated the treatment of patients with intercondylar fractures of the distal humerus. The primary outcome was the incidence of functional grading of excellent/good.
Results: The methods used to evaluate elbow function were diverse across the studies and included non-surgical, fixation and plating approaches. The most common surgical technique used was olecranon osteotomy (n = 7) and triceps-sparing (n = 5). In general, most procedures were associated with >70% of patients having excellent/good joint function following surgery. The meta-analysis included four studies with 276 patients, and compared olecranon osteotomy with triceps-sparing. The pooled analysis indicated that patients treated using olecranon osteotomy had better functional outcome than patients treated with triceps-sparing (pooled OR = 2.38, 95%CI: 1.25–4.55, p = .009).
Conclusions: This study found that a wide range of surgical procedures were effective in treating most patients with distal humerus intercondylar fractures, and that the approach of olecranon osteotomy may be more effective than that of triceps-sparing in restoring joint function.
Most procedures in treating distal humerus intercondylar fractures were associated with >70% of patients having excellent/good joint function following surgery.
The most common surgical technique used in treating distal humerus intercondylar fractures were olecranon osteotomy and triceps-sparing.
The pooled analysis indicated that patients treated using olecranon osteotomy had better functional outcome than patients treated with triceps-sparing.
Key messages
Introduction
Distal humerus intercondylar fractures are intra-articular comminuted fractures of the elbow that involve soft tissue injury [Citation1]. These types of fractures are relatively rare (<2%) and are difficult to treat due to their epiphyseal location [Citation2]. Complete fractures result from impaction of the proximal ulna onto the articular part (trochlea, capitellum) of the distal humerus, and can occur with the elbow flexed or extended [Citation2]. Due to the fact these fractures are fairly rare, a specific management scheme is challenging to devise [Citation2].
Treatment consists of assessing the mechanism of the injury, defining the diagnostic modalities, and developing a clinical approach which will allow for recovery of full mobility of the elbow [Citation2]. Any approach should aim at mobilizing the elbow joint to avoid stiffening and heterotopic ossification [Citation3,Citation4]. Immobilization is only feasible in situations in which the fractures are non-displaced or as temporary treatment under specific circumstances [Citation2,Citation4]. Normal function can be difficult to restore if the joint is deformed due to malunion and/or stiffened by capsular and ligament contractures or heterotopic ossifications.
Surgery is the common treatment for this type of fracture [Citation5]. Non-surgical treatment can be performed in cases of hemiplegia sequelae that involve the ipsilateral upper limb, advanced osteoporosis and fractures with extensive bone loss [Citation3]. However, function results are typically less than optimal [Citation3,Citation5]. The primary goal of surgical treatment is to obtain fixation with sufficient stability so that the elbow can be mobilized immediately following surgery [Citation2,Citation3]. The type of treatment depends upon the fracture characteristics, with partial and complete fractures requiring different treatment strategies [Citation2,Citation3]. Techniques range from conservative surgical treatment using internal fixation in young patients to elbow joint replacement in older patients with comminuted fractures [Citation2,Citation3]. Olecranon osteotomy is considered the “gold standard” treatment for distal humerus fractures [Citation2,Citation6]. Fixation for complex fractures can consist of reconstruction plates or locking compression plates, with one plate being placed on each column to neutralize disassembly forces, especially rotational ones. Complication following surgery includes loss of reduction, implant failure, nonunion, malunion, ulnar nerve neuropathy, elbow stiffness and heterotopic ossification [Citation7].
The approach that is most effective for treating this fracture is unclear and may depend upon several factors, such as fracture complexity and patient characteristics. In this systematic review and meta-analysis, we evaluated the effectiveness different surgical approaches on elbow functional outcomes in the treatment of distal humerus fracture.
Patients and methods
Search strategy
The study was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Medline, Cochrane, EMBASE and Google Scholar databases were searched up to 29 July 2016 using the search term humerus intercondylar fracture. The purpose of the PRISMA Statement is to help authors improve the reporting of systematic reviews and meta-analyses. Randomized controlled studies (RCTs) and two-arm, prospective, retrospective, cohort, case control and case series studies were included. All studies had to have evaluated the treatment of patients with intercondylar fractures of distal humerus, and to have reported quantitatively outcomes of interest. Letters, comments, editorials, proceedings and personal communications were excluded. Studies that included patients with previously treated intercondylar fracture were also excluded. The reference lists of all included studies were hand-searched to identify other eligible studies. The list of potential studies identified through the database search was reviewed for inclusion by two independent reviewers. Where there was uncertainty regarding eligibility, a third reviewer was consulted.
Data extraction and quality assessment
The following information/data were extracted from studies that met the inclusion criteria: the name of the first author, year of publication, study design, number of participants in each group, participants’ age and gender, types of fracture, follow-up time, and the major outcomes.
We only performed quality assessment on the three retrospective studies used in the meta-analyses by using ACROBAT-NRSI (A Cochrane Risk Of Bias Assessment Tool: for Non-Randomized Studies of Interventions) [Citation8]. ACROBAT-NRSI is concerned with evaluating risk of bias in the results of non-randomized studies that compare the health effects of two or more interventions.
Outcome measures
The primary outcome for the meta-analysis was functional grading of excellent/good between patients treated using olecranon osteotomy and those treated with triceps-sparing.
Statistical analysis
Odds ratio with 95% confidence intervals (CIs) was calculated between patients in the olecranon osteotomy group and triceps-sparing group for each individual study included in the meta-analysis and for all the studies combined. A χ2-based test of homogeneity was performed and the inconsistency index (I2) and Q statistics were determined. Heterogeneity was determined using the I2 statistic and was defined as follows: 0–24% = no heterogeneity; 25–49% = moderate heterogeneity; 50–74% = large heterogeneity; and 75–100% = extreme heterogeneity. As the number of studies included in the meta-analysis was small, heterogeneity tests had low statistical power [Citation9]. When tests for heterogeneity are underpowered, random-effects models are used routinely [Citation10]. The National Research Council report recommends the use of random-effects approaches for meta-analysis and the exploration of sources of variation in study results [Citation11]. Pooled effects were calculated, and a two-sided p value <.05 was considered to indicate statistical significance. Sensitivity analysis was carried out using the leave one-out approach. Publication bias using a funnel plot was not performed as >10 studies are necessary for this type of analysis [Citation12]. All analyses were performed using Comprehensive Meta-Analysis statistical software, version 2.0 (Biostat, Englewood, NJ).
Results
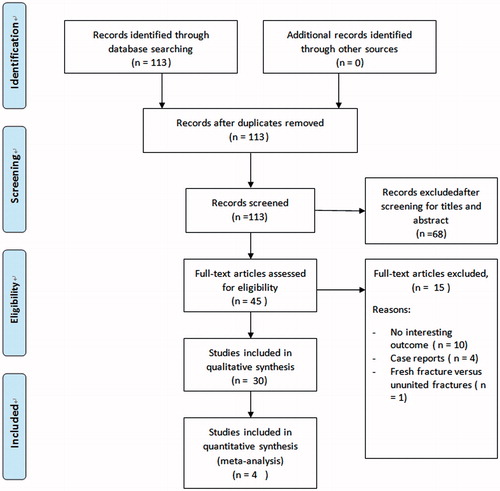
Of the 113 records identified, 68 were removed after the initial screen of titles and abstracts (). Forty-five studies underwent full-text review and 15 were excluded for not reporting outcomes of interest, being case reports, or evaluating fresh fractures versus ununited fractures. Thirty papers were included in the systematic review [Citation5,Citation7,Citation13–40].
Systematic review
The systematic review included 17 retrospective, 11 prospective and two RCTs. Types of treatments varied across studies (). The most common approaches evaluated for treating distal humus intercondylar fracture were olecranon osteotomy (n = 7) and triceps sparing (n = 5). The criteria used to assess the fracture also varied and included Orthopedic Trauma Association (OTA) (n = 1), AO (n = 18), Muller (n = 5), Riseborough and Radin (n = 2), AO/ASIF (n = 1), Gustillo and Anderson (n = 1) criteria. Across the 30 studies, the age ranged from 14 to 78.4 years, the percentage of males ranged from 0% to 85.7%, and follow-up ranged from 12 to 6.9.6 months. The method used to assess elbow function following surgery was diverse and included the Cassebaum (n = 5), Aitken and Rorabeek (n = 2), Jupiter (n = 1), sagittal, frontal, transverse, rotation (SFTR) (n = 1), Mayo Elbow Performance Score (MEPS) (n = 10), OTA (n = 1), Riseborough and Radin (n = 1) and Murray’s (n = 1) systems. The type of fractures ranged from AO criteria C1 to C3 and most were due to a motor vehicle accident or fall.
Table 1. Baseline demographics of the selected studies.
Olecranon osteotomy and triceps-sparring approaches
Of the studies that evaluated olecranon osteotomy, functional outcomes were considered excellent/good in 64.8–89.3% of cases (). Across the studies that assessed triceps-sparing, the range of cases graded as having excellent/good joint function ranged from 70.7% to 100%. In Khalid et al., 89.3% of the cases treated with olecranon osteotomy compared with 70.7% treated with triceps sparing had excellent/good elbow function following surgery [Citation34]. Similarly, Pajarinen and Björkenheim found olecranon osteotomy was associated with 66.7% excellent/good function compared with 33.3% for triceps splitting [Citation36]. Chen et al. found olecranon osteotomy used for open reduction and internal fixation (ORIF) resulted in 81.8% of cases with excellent/good joint function after surgery compared with 79.4% for triceps-sparing for ORIF [Citation35]. The range of flexion, extension, flexion arc, pronation, supination and rotation arc was also comparable between treatments (). Liu et al. found similar joint function after use of trans-olecranon osteotomy, Cambell (Van Gorder), or triceps-sparing approaches with 84.2%, 80.0% and 83.3% of cases, respectively, having excellent/good functional outcomes [Citation37]. In Liu et al., flexion and extension were similar across the three treatments.
Table 2. Summary of outcomes of the selected studies.
Other approaches
A number of single-arm studies evaluated various other approaches for treating distal humerus intercondylar fracture. Dreyfuss and Eidelman used the transolecranon approach for ORIF and found 6/6 (100%) of subjects had excellent/good function following surgery, with a mean flexion of 133° and an extension of 11° [Citation29]. Lakhey et al. used the Bryan and Morrey approach and the patients had a mean flexion of 124°, extension 9° and flexion arc of 115° [Citation7]. Ali et al. treated the fracture using the extensor mechanism sparing paratricipital posterior approach and had 86.4% of cases with excellent/good function after joint repair, with 120° flexion and 6° extension [Citation15]. Two single arm studies investigated the effectiveness of triceps-reflecting anconeus pedicle (TRAP) approach [Citation19,Citation20]. Ozer et al. found that 90.9% of cases were evaluated as having excellent/good functional outcomes after surgery [Citation20]. They found the mean flexion was 119° and mean extension 7°. Using the same approach, Pankaj et al. had similar findings with the mean flexion being 5° and the mean extension 118°. Pankaj et al. did not report functional evaluation [Citation19]. The retrospective study of Jupiter et al. assessed the treatment of intercondylar fracture of the distal end of the humerus using ORIF [Citation27]. They found that 79.4% of the cases had excellent/good elbow function following surgery [Citation27].
Plating and fixation
Various methods were used across the studies for treating distal humerus intercondylar fracture using methods of fixation and plating. Across these studies, the range of patients with functional grading following surgery of excellent/good ranged from 71.4% to 100% (). The studies of Shuang et al. and Tian et al. compared different plating methods for treating the fracture [Citation38,Citation39]. Shuang et al. compared conventional plates with 3D-printed plates and found the 3D-printed plates had a slightly greater percentage of patients (83.3%) with excellent/good functional outcomes than patients treated with conventional plates (71.4%). Tian et al. found no difference in the percentage of patients whose fracture was treated with perpendicular plating compared with Y-shaped plating (84.6% vs. 83.3%, respectively).
Lansinger and Mare compared patients who were treated surgically (n = 28) to those who received conservative treatment (n = 11) [Citation40]. In 26 patients, surgical treatment involved open reduction with various types of fixation such as screws (n = 9), plates (n = 1) and Kirchner wires or metal pins (n = 16). Two patients were treated with open reduction without internal fixation. They found that 36% of the patients whose elbow was repaired surgically had good results compared with 27.3% of patients who received conventional treatment.
Meta-analysis
Four two-arm studies (Khalid et al. (2015), Chen et al. (2011), Liu et al. (2009) and Pajarinen and Björkenheim (2002)) with a total of 276 patients were included in the meta-analysis. Khalid et al. was an RCT and the other three studies were two-arm retrospective in design (). The age of the patients across the four studies ranged from 43 to 53.8 years, the percentage of males ranged from 38.1% to 55.3% and follow-up from 24.2 to 34.3 months.
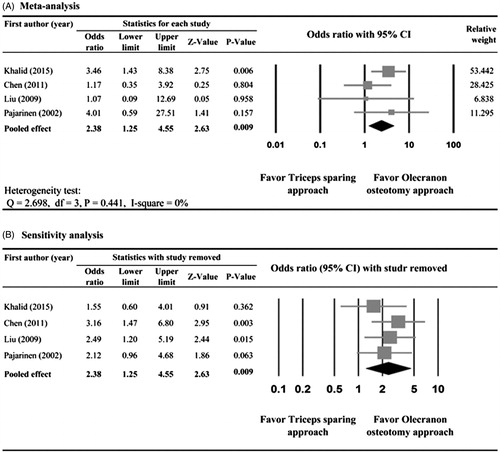
No heterogeneity was observed in the data of functional grading across the four studies (Q statistic = 2.695, I2 = 0%). The pooled analysis found that the patients treated using olecranon osteotomy had better elbow function postsurgery than patients treated with triceps-sparing (pooled OR = 2.38, 95%CI: 1.25–4.55, p = .009) ().
Quality assessment
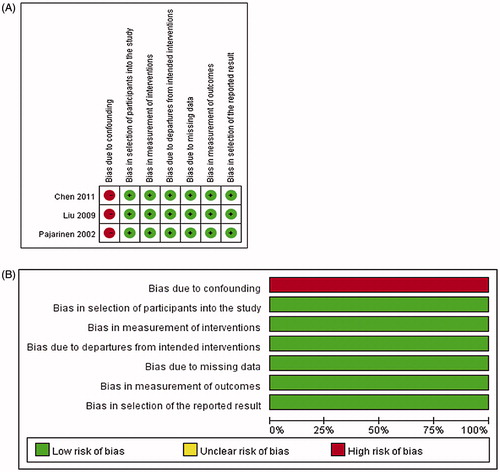
We used ACROBAT-NRSI to evaluate quality of the three retrospective studies included in the meta-analysis (). A high risk of bias due to confounding was observed across the three studies. The three studies had low risk of other possible biases, such as patient selection, measurement of interventions, and missing data. Overall the three studies were of good quality.
Sensitivity analysis
Sensitivity analyses were performed using the leave-one-out approach in which the meta-analysis was performed with each study removed in turn (). The direction of the combined estimates did not vary markedly with the removal of any single study, indicating that the meta-analysis had good reliability and the data were not overly influenced by any one study.
Discussion
Distal humerus intercondylar fractures are relatively rare fractures, and specific management scheme is not clear. Multiple approaches have been used to treat this type of fracture with the aim of treatment to restore elbow joint function. This systematic review and meta-analysis evaluated the effectiveness different surgical approaches on elbow functional outcomes in the treatment of distal humerus fracture. The systematic review included 30 studies: 17 retrospective, 11 prospective and two RCTs. The methods used to evaluate elbow function were diverse across the studies and included non-surgical, fixation and plating approaches. A wide range of different surgical techniques were assessed with the most common being olecranon osteotomy and triceps sparing. In general, most procedures were associated with >70% of patients having excellent/good joint function following surgery. The meta-analysis included four studies with 276 patients. The pooled analysis indicated that patients treated using olecranon osteotomy had better joint function after treatment than patients who were treated with triceps-sparing (p = .009). Our findings are consistent with olecranon osteotomy being the “gold standard” approach for repairing distal humeral fracture. To our knowledge, this is the first systematic review and meta-analysis to evaluate different treatments for distal humerus intercondylar fractures.
The choice of surgery depends upon characteristics of the fracture and depending on the fracture the different approaches may have certain advantages. Although the olecranon osteotomy approach is commonly used, it has potential complications related to prominence/migration of hardware, displacement/nonunion of osteotomy, and triceps weakness [Citation19]. In the study of Ek et al., patients (N = 7) with complex intercondylar fractures were treated using a posterior triceps-sparing approach which resulted in excellent/good joint function in all patients [Citation18]. Pankaj et al. and Ozer et al. used the TRAP approach for distal intercondylar fractures [Citation19,Citation20]. Ozer et al. reported this approach resulted in 91% of patients having excellent/good joint function following surgery [Citation20]. The TRAP procedure has the advantage that it can avoid transolecranon-related complications, negative effect on triceps strength, and reduce the need for postoperative rehabilitation [Citation19,Citation20].
In the studies that reported different types of plating methods, most resulted in a high percentage of patients having excellent/good joint function. Tian et al. found in a retrospective study that perpendicular plating and Y-shaped double plating provided good fixation and satisfactory clinical outcomes [Citation38]. The RCT of Shuang et al. compared the effectiveness of conventional with 3D-printed osteosynthesis plates in treating intercondylar humeral fractures [Citation39]. Using computer tomography (CT), a 3D model of the patient’s fractured elbow was made. Custom osteosynthesis plates with the proper size and number holes were subsequently fabricated based on the model using a 3D printer. The 3D-printed plates gave a slightly higher rate of excellent/good functional evaluations than conventional plates (83.1% vs. 71.4%) indicating that custom 3D printed osteosynthesis plates are safe and effective for repairing intercondylar humeral fractures. The 3D-printed plates were associated with a significantly shorter operative time compared to conventional plates.
A number of factors can influence outcomes. The study of Jupiter et al. reported outcomes in patients with open reduction [Citation27]. They found that factors associated with poor outcomes included multiple trauma and type C3 fracture. This is consistent with Allende et al. who found that the final results following surgical repair was related to the severity of the initial trauma [Citation21]. Wang et al. recommended the use of routine ulnar nerve anterior subcutaneous transposition with a posterior approach to avoid postoperative ulnar nerve compression syndrome [Citation26], and Cannada et al. suggested capsulectomy for patients with postoperatively limited range of motion [Citation31]. Good clinical results were observed for open intercondylar fractures using a mini-external fixator [Citation16,Citation30], as well as for the use of angular stable internal fixation with LCP distal humerus system for patients with supra-intercondylar fractures [Citation17].
Treatment of elderly patients can be complicated by the presence of osteoporosis. Burg et al. used closed reduction and external fixation with a ring as a minimally invasive approach for treating elderly patients with osteoporotic bone [Citation14]. This approach was associated with good clinical outcomes as the mean flexion was 115° and mean extension 22°. Chen et al. reported that the choice of ORIF with olecranon osteotomy, compared with triceps-sparing, resulted in better function outcomes in patients >60 years of age. The rate of excellent/good MEPS was >80% for all ages in the group of patients treated with ORIF via olecranon osteotomy. In contrast, only 37.5% patients in the triceps-sparing group >60 years of age obtained excellent/good MEPS and these patients tended to have more extension loss (mean 23°, range 0–55°) [Citation35]. However, the rate of excellent/good MEPS was 100% in patients <40 years of age treated with triceps-sparing.
The study has several limitations that should be considered. Only a few studies were RCTs. In addition, heterogeneity existed across the studies with respect to the type of fracture, the criteria used to evaluate the severity of the fracture, and the assessment tool used to evaluate joint function following surgery. The definition of excellent/good joint function varied according to different scales. For example, the studies of Khalid et al. and Chen et al. used the MEPS which uses an objective measure of functional outcome [Citation41]. The full score of MEPS is 100, according to pain, stability, morbidity and daily functional activity. The result of MEPS could fall into four grades: ≥90, excellent; 75–89, good; 60–74, fair; and <60, poor. Liu et al. assessed elbow function using the Aitken and Rorabeck [Citation42]. An excellent result had an arc of flexion of 110° or more, full use of the arm including heavy labour, and no pain. A good result had at least 75° of flexion, no more than slight pain, and was able to perform the activities of daily living. The study of Pajarinen and Björkenheim used the Orthapedic Trauma Association (OTA) method for evaluating elbow function [Citation36]. An excellent result has range of motion of >125° and with anatomic restitution; a good result had range of motion of >95° with anatomic restitution. This variability makes it difficult to compare findings across studies. In addition, the sample size for the meta-analysis was small, indicating the need for more RCTs are necessary to further investigate what might be the optimal method(s) for treating this type of fracture.
In summary, a wide range of surgical procedures were effective in treating most patients with distal humerus intercondylar fractures. Olecranon osteotomy may be more effective than triceps-sparing approach with respect to restoring joint function, particularly in the elderly.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Sanchez-Sotelo J, Torchia ME, O'Driscoll SW. Complex distal humeral fractures: internal fixation with a principle-based parallel-plate technique. J Bone Joint Surg Am. 2007;89:961–969.
- Begue T. Articular fractures of the distal humerus. Orthop Traumatol Surg Res. 2014;100:S55–S63.
- Miller AN, Beingessner DM. Intra-articular distal humerus fractures. Orthop Clin N Am. 2013;44:35–45.
- Hausman M, Panozzo A. Treatment of distal humerus fractures in the elderly. Clin Orthopaed Relat Res. 2004;(425):55–63.
- Jung SW, Kang SH, Jeong M, et al. Triangular fixation technique for bicolumn restoration in treatment of distal humerus intercondylar fracture. Clin Orthop Surg. 2016;8:9–18.
- Nauth A, McKee MD, Ristevski B, et al. Distal humeral fractures in adults. J Bone Joint Surg Am. 2011;93:686–700.
- Lakhey S, Sharma S, Pradhan RL, et al. Osteosynthesis of intercondylar humerus fracture using Bryan and Morrey approach. Kathmandu Univ Med J. 2010;8:154–157.
- Sterne JAC, Higgins JPT, Reeves BC, et al. A Cochrane Risk Of Bias Assessment Tool: for Non-Randomized Studies of Interventions (ACROBAT-NRSI), [Internet] Version 1.0.0, 24 September 2014. Available from: http://www.riskofbias.info
- Hardy RJ, Thompson SG. Detecting and describing heterogeneity in meta-analysis. Stat Med. 1998;17:841–856.
- Takkouche B, Cadarso-Suarez C, Spiegelman D. Evaluation of old and new tests of heterogeneity in epidemiologic meta-analysis. Am J Epidemiol. 1999;150:206–215.
- National Research Council. Combing information: statistical issues and opportunities for research. Washington (DC): National Academy Press; 1992.
- Sterne JA, Sutton AJ, Ioannidis JP, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002.
- Julfiqar PA, Huda N, Ahmed W. Closed reductions and percutaneous 'k' wire fixation for adolescent intercondylar fractures of the distal humerus. J Clin Diagn Res: JCDR. 2013;7:1666–1668.
- Burg A, Berenstein M, Engel J, et al. Fractures of the distal humerus in elderly patients treated with a ring fixator. Int Orthopaed (SICOT). 2011;35:101–106.
- Ali AM, Hassanin EY, El-Ganainy AE, et al. Management of intercondylar fractures of the humerus using the extensor mechanism-sparing paratricipital posterior approach. Acta Orthop Belg. 2008;74:747–752.
- Chaudhary S, Patil N, Bagaria V, et al. Open intercondylar fractures of the distal humerus: management using a mini-external fixator construct. J Shoulder Elbow Surg. 2008;17:465–470.
- Greiner S, Haas NP, Bail HJ. Outcome after open reduction and angular stable internal fixation for supra-intercondylar fractures of the distal humerus: preliminary results with the LCP distal humerus system. Arch Orthop Trauma Surg. 2008;128:723–729.
- Ek ET, Goldwasser M, Bonomo AL. Functional outcome of complex intercondylar fractures of the distal humerus treated through a triceps-sparing approach. J Shoulder Elbow Surg. 2008;17:441–446.
- Pankaj A, Mallinath G, Malhotra R, et al. Surgical management of intercondylar fractures of the humerus using triceps reflecting anconeus pedicle (TRAP) approach. Indian J Orthop. 2007;41:219–223.
- Ozer H, Solak S, Turanli S, et al. Intercondylar fractures of the distal humerus treated with the triceps-reflecting anconeus pedicle approach. Arch Orthop Trauma Surg. 2005;125:469–474.
- Allende CA, Allende BT, Allende BL, et al. Intercondylar distal humerus fractures – surgical treatment and results. Chirurgie De La Main. 2004;23:85–95.
- Yang KH, Park HW, Park SJ, et al. Lateral J-plate fixation in comminuted intercondylar fracture of the humerus. Arch Orthop Trauma Surg. 2003;123:234–238.
- McKee MD, Wilson TL, Winston L, et al. Functional outcome following surgical treatment of intra-articular distal humeral fractures through a posterior approach. J Bone Joint Surg Am. 2000;82:1701–1707.
- Jamali AR, Mehboob G, Ahmed S. Extensor mechanism sparing approach to the elbow for reduction and internal fixation of intercondylar fracture of the humerus. J Pak Med Assoc. 1999;49:164–167.
- Low CK, Wong DH, Toh CL, et al. A retrospective study on elbow function after internal fixation of intercondylar fracture of adult humerus. Ann Acad Med Sing. 1997;26:168–171.
- Wang KC, Shih HN, Hsu KY, et al. Intercondylar fractures of the distal humerus: routine anterior subcutaneous transposition of the ulnar nerve in a posterior operative approach. J Trauma. 1994;36:770–773.
- Jupiter JB, Neff U, Holzach P, et al. Intercondylar fractures of the humerus. An operative approach. J Bone Joint Surg Am. 1985;67:226–239.
- Kumar S, Singh S, Kumar D, et al. Intercondylar humerus fracture – parallel plating and its results. J Clin Diagn Res: JCDR. 2015;9:Rc01–Rc04.
- Dreyfuss D, Eidelman M. Treatment of complex intercondylar humeral fractures in adolescents by open reduction and internal fixation through the transolecranon approach. J Pediatr Orthoped B. 2014;23:364–368.
- Banerjee D, Ghosh S, Ghosh PK, et al. A short term experience of management of open and osteoporotic intercondylar fractures of the distal humerus using a mini-external fixator. J Indian Med Assoc. 2011;109:6–8.
- Cannada L, Loeffler B, Zadnik MB, et al. Treatment of high-energy supracondylar/intercondylar fractures of the distal humerus. J Surg Orthopaed Adv. 2011;20:230–235.
- Yang Y, Huang PQ, Fang JW. Treatment of severely comminuted fractures of humeral intercondylar through approach of osteotomy olecranon with double-plate internal fixation. Zhongguo Gu Shang = China J Orthopaed Traumatol. 2009;22:335–336.
- Tang XJ, Zhou CK, Wang XM, et al. Dual steel plate for the surgical management of intercondylar fractures of the humerus through approach of osteotomy of olecranon. Zhongguo Gu Shang = China J Orthopaed Traumatol. 2009;22:331–333.
- Khalid MU, Saeed KM, Akhter M. A comparison of functional outcome of intercondylar fracture of distal humerus managed by olecranon osteotomy approach versus triceps sparing approach in adults. JPMA: J Pak Med Assoc. 2015;65:S119–S122.
- Chen G, Liao Q, Luo W, et al. Triceps-sparing versus olecranon osteotomy for ORIF: analysis of 67 cases of intercondylar fractures of the distal humerus. Injury. 2011;42:366–370.
- Pajarinen J, Björkenheim J-M. Operative treatment of type C intercondylar fractures of the distal humerus: results after a mean follow-up of 2 years in a series of 18 patients. J Should Elbow Surg. 2002;11:48–52.
- Liu YK, Xu H, Liu F, et al. Treatment of type C intercondylar fractures of distal humerus using dual plating. Zhonghua Wai Ke Za Zhi [Chin J Surg]. 2009;47:892–895.
- Tian D, Jing J, Qian J, et al. Comparison of two different double-plate fixation methods with olecranon osteotomy for intercondylar fractures of the distal humeri of young adults. Exp Ther Med. 2013;6:147–151.
- Shuang F, Hu W, Shao Y, et al. Treatment of intercondylar humeral fractures with 3D-printed osteosynthesis plates. Medicine. 2016;95:e2461.
- Lansinger O, Mare K. Intercondylar T-fractures of the humerus in adults. Arch Orthop Trauma Surg. 1982;100:37–42.
- Morrey BF, An KN, Chao EYS. Functional evaluation of the elbow. In: Morrey BF, editor. The elbow and its disorders. 2nd ed. Philadelphia: WB Saunders; 1993. p. 86–89.
- Aitken GK, Rorabeck CH. Distal humeral fractures in the adults. Clin Orthop Relat Res. 1986;207:191–197.