Abstract
Purpose
To determine whether alcohol intake is associated with occurrence of headaches on the following day.
Methods
In this prospective cohort study, adults with episodic migraine completed electronic diaries every morning and evening for at least six weeks in March 2016–October 2017. Every day, participants reported alcohol intake, lifestyle factors, and details about each headache. We constructed within-person fixed-effect models adjusted for time-varying factors to calculate odds ratios for the association between 1,2,3,4, or 5+ servings of alcohol and headache the following day. We also calculated the adjusted risk of headache the following day for each level of intake.
Results
Among 98 participants who reported 825 headaches over 4,467 days, there was a statistically significant linear association (p-trend = 0.03) between alcohol and headache the following day. Compared to no alcohol, 1–2 servings were not associated with headaches, but 5+ servings were associated with a 2.08-fold (95% confidence interval [CI] 1.16–3.73) odds of headache. The adjusted absolute risk of headaches was 20% (95%CI 19%–22%) on days following no alcohol compared with 33% (95%CI 22%–44%) on days following 5+ servings.
Conclusion
1–2 servings of alcoholic beverages were not associated with higher risk of headaches the following day, but 5+ servings were associated with higher risk.
1–2 servings of alcoholic beverages were not associated with a higher risk of headaches on the following day, but higher levels of intake may be associated with higher risk.
Five or more servings were associated with 2.08 times (95% confidence interval 1.16–3.73 the odds of headache on the following day.
The adjusted absolute risk of headaches was 20% (95%CI 19%–22%) on days following no alcohol consumption compared with 33% (95% CI 22%–44%) on days following 5+ servings.
KEY MESSAGES
Background
Migraine headaches may cause debilitating discomfort and commonly involve throbbing pain, nausea and sensitivity to light and sound. Migraine affects more than 1 billion people worldwide [Citation1], and approximately 20% of people experience migraines at some point in their lives. In 2014, patient-reported headache led to 4 million emergency department (ED) visits in the US, representing the fifth leading cause and 3% of all ED visits. It is well known that regardless of headache history, heavy alcohol intake can cause “hangover headaches”, classified as delayed alcohol-induced headaches [Citation2]. However, patients with episodic migraine often report that even small amounts of alcohol consumption may trigger headaches with symptoms similar to their usual migraines [Citation3,Citation4]. As a common but modifiable exposure, elucidating the association between alcoholic beverages and headache risk among patients with episodic migraine may provide insight for clinical recommendations to prevent headaches in this population.
Several studies asked participants whether they believed that alcohol triggers their migraine or tension-type headache [Citation5–8], raising concerns of recall bias whereby participants are more likely to recall alcohol intake preceding a migraine and underreport the frequency of alcohol intake not followed by a headache. Therefore, we conducted a prospective cohort study of adults with episodic migraine to assess an individual’s risk of headache on the day after alcohol intake compared to that same individual’s risk on other days, adjusting for other behaviours that may be temporally associated with alcohol intake and headache occurrence.
Methods
Study population
We previously described the recruitment and enrolment process [Citation9]. In brief, we identified potential participants from three academic medical centres. We enrolled individuals who experienced migraine headaches for at least 3 years, and for the last 3 months, they have experienced at least two migraines per month and fewer than 15 headache-days per month. All individuals met the criteria for International Classification of Headache Disorders for migraine with or without aura [Citation2] based on physician evaluation during the baseline visit, and we excluded participants with potential medication overuse headaches. All participants were ≥18 years of age and able to communicate in English. Exclusion criteria were self-reported chronic pain syndrome; chronic opioid use; high risk for obstructive sleep apnoea assessed via Berlin questionnaire or known untreated moderate or severe sleep apnoea; pregnancy; and failure to complete 4/7 days of a run-in phase diary. 131 individuals completed the screening visit and a run-in phase to ensure adherence with completing daily electronic diaries. Between March 2016 and October 2017, participants completed daily diaries. Among 101 who met inclusion criteria and agreed to participate, three withdrew with <21 days of diary data, resulting in a sample of 98 patients with episodic migraine who completed the study.
Participants provided daily information about health behaviours and headaches by completing secure internet-based diaries every morning and evening. They wore Actiwatch-Spectrum® actigraphs (Philips Respironics, Inc.) on their non-dominant wrist. Each participant provided information for at least six weeks. We collected study data using REDCap electronic data tools hosted at Beth Israel Deaconess Medical Centre (BIDMC) [Citation10]. The study was approved by the BIDMC Committee on Clinical Investigations. All participants provided written consent.
Baseline information
At baseline, participants provided information about menopausal status, medication use, and typical headache symptoms. They completed the Headache Impact Test-6 [Citation11] and reported whether they typically experience visual aura before their headaches (“Do you typically see flashing/shimmering lights or a blind spot before headache?”).
Alcohol and covariates
To characterise the study sample at baseline, we collected information on demographics, medical history, medication use, typical servings of alcohol per week, typical servings of caffeinated beverages per day, habitual physical activity, and measures of psychological stress and depressive symptoms. We showed participants a list of commonly reported triggers of migraine headache, such as alcohol, irregular sleep, and weather changes, and we asked them to report which ones they believed had typically triggered their migraines.
In the daily morning questionnaire, we asked about the number of servings of alcohol consumed on the prior day (0, 1, 2, 3, 4, or 5+) and about sleep and wake times. Every evening in the hour prior to getting into bed, participants recorded the number of servings of caffeinated beverages consumed that day and time spent that day engaged in moderate (e.g. fast walking, average bicycling) or vigorous (e.g. running/jogging, fast bicycling) activities. We objectively measured total minutes of physical activity with wrist actigraphs. Using data from daily diaries and actigraphs, a trained technician blinded to daily headache information used a standardised protocol [Citation12] to identify daily sleep and wake times and calculate sleep duration. In the evening diary, we included two scales of psychological stress. Participants responded to seven items from the Positive and Negative Affect Schedule [Citation13], and they rated their current intensity of feeling upset, nervous, afraid, distressed, scared, enthusiastic, and alert using Likert scales (very slightly or not at all, a little, moderately, moderately, quite a bit, extremely). They also completed seven questions from the Daytime Insomnia Symptom Scale [Citation14]. Using a visual analogue scale ranging from 0 (not at all) to 100 (as much as possible), they rated the intensity of anxiety, tension, sadness, relaxation, energy, and calmness. Pre- and peri-menopausal females also reported whether they experienced menstrual bleeding that day.
Headaches
Every morning and evening, participants reported the onset, duration, pain intensity, and medications used for any headaches that they had experienced since their previous diary. They reported any visual aura and symptoms (e.g. throbbing or pounding head pain, nausea, vomiting, and sensitivity to light and sounds), and whether the headache was similar to their typical migraines. If participants reported that a headache started before the end of a prior headache, it was considered an extension of the earlier headache. A study physician (SMB) blinded to daily exposure data reviewed the diaries on the symptoms of each headache. If a participant reported a headache that lasted <4 h, had an intensity <40/100, involved <1 migrainous feature (e.g. photophobia), and required no abortive medications, the headache was classified as unlikely to be a migraine.
Statistical analysis
We conducted a within-person repeated measures fixed-effect analysis to estimate relative and absolute measures of the association between the number of servings of alcoholic beverages and occurrence of headaches on the following day adjusted for time-varying factors. In primary analyses, we included any type of headache, and in sensitivity analyses, we restricted to headaches classified as likely to be a migraine headache. In all analyses, we included the calendar day when headache symptoms began as the headache day and excluded all subsequent days with the continuation of headache symptoms. In a sensitivity analysis, we further excluded all days with the initiation of headache symptoms if it was on the next calendar day following a headache day. We constructed unconditional logistic regression models with robust sandwich estimators of variance and stratified on participant and day of week as indicator terms. We estimated the odds ratio of a headache on the day following 1, 2, 3, 4, or 5+ servings of alcohol compared to no intake. We conducted a test for linear component of trend by determining the statistical significance of a term for the alcoholic beverage intake as linear continuous variable.
We also calculated the average treatment effect using a causal counterfactual framework to estimate the adjusted marginal risk of a migraine using a potential outcomes approach [Citation15]. In brief, for each level of alcohol intake, we calculated the adjusted average risk per day of having a headache had everyone in the sample consumed that number of alcohol servings. We estimated average treatment effects as the average risk of having a headache had everyone consumed that number of alcohol servings on a given day minus the average risk of having a migraine on that day had everyone consumed no alcohol.
Because the fixed-effect analysis evaluates the risk of headache when exposure changes within an individual, similar to a clinical crossover trial, it eliminates confounding by fixed (e.g. sex, genotype) or slowly-varying (e.g. age) characteristics [Citation15]. We adjusted for day of week to eliminate confounding by weekend versus weekday habits that may impact intake and headache occurrence. There can be confounding by time-varying characteristics (e.g. nightly sleep) related to the timing of alcoholic beverage intake and migraines on a particular day. Therefore, we conducted additional analyses that adjusted for daily levels of caffeinated beverage intake (1, 2, 3, 4, 5+ servings), psychological stress (continuous), self-reported (continuous) and actigraphy-based (continuous) measures of physical activity, day with menstrual bleeding (yes/no), and that day’s difference in minutes from the participant’s usual sleep duration.
We examined whether the association varied by baseline information about self-reported typical frequency of alcoholic beverage intake (<3 vs ≥3 servings per week), self-reported presence of migraine with aura, and whether the participant endorses alcohol as a trigger of their migraines. We calculated the product of indicator variables for alcoholic beverage intake and each potential modifier, and conducted likelihood ratio tests of nested models with and without interaction terms.
We examined the robustness of our findings in secondary analyses: 1) we reclassified migraine headaches starting on consecutive days as a single event; we excluded 2) participants that typically used migraine prophylaxis medications; 3) headaches classified as unlikely to be migraines; 4) headaches that began while participants were asleep 5) headaches that were reported as different from their usual migraine headaches.
Two-sided p values of <.05 were considered statistically significant. Analyses were primarily performed using SAS 9.4 (Institute Inc., Cary, NC). Average treatment effects were estimated using Stata statistical software (version 16.0, StataCorp).
Results
Baseline characteristics of the 98 participants (86 women, 12 men) are included in . Based on the daily diary data collected over the six weeks of follow-up, participants reported consuming an average of 3.9 (standard deviation [SD] = 3.9) servings per week on an average of 1.9 (SD = 1.6) days per week. Eight participants reported no alcohol intake during the study, and therefore, they did not contribute information to this analysis. Participants reported 825 headaches during 4,467 days of observation, with an average of 8.4 (SD = 4.6) headaches per participant. Among 825 reported headaches, 580 (70%) were classified as similar to usual migraines, 175 were reported as different, and for 70 headaches, participants did not report whether or not they were similar to usual migraine headaches.
Table 1. Baseline Characteristics, mean ± standard deviation or frequency (%) among 98 participants with episodic migraines followed for 6 weeksTable Footnotea.
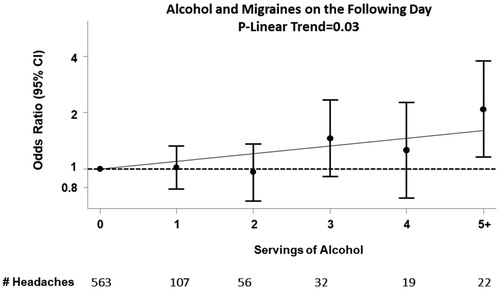
There was a statistically significant linear association between alcoholic beverage intake and the odds of migraine headaches on the following day (p-linear trend = 0.03; ), though most of the individual estimates did not reach statistical significance. There was no association between 1–2 servings of alcoholic beverage intake and the odds of headaches on the following day, but higher odds on days following ≥3 servings, with 2.1-fold higher odds of headache on the day following ≥5 servings (95% confidence interval [CI] 1.2–3.7). Results were similar when we further adjusted for other time-varying factors.
Figure 1. Association between servings of alcohol intake compared to none and occurrence of migraine on the following day among 98 participants with episodic migraines followed for 6 weeks. The observed estimates of the association for each number of servings of alcohol are shown with the circles (odds ratios) and vertical lines (95% confidence intervals), and the linear association is shown with the solid line. The dashed line reflects the null value of no association between alcohol intake and occurrence of migraine headaches.
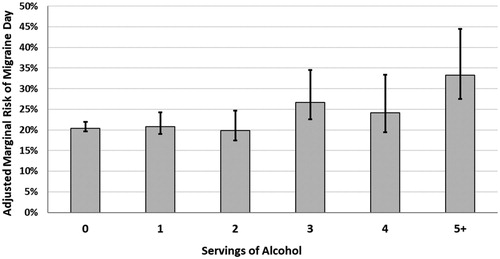
presents the adjusted marginal probability of having a headache day according to alcohol intake ranging from a 20% (95%CI 19% to 22%) risk of headaches on days following no alcohol consumption to a risk of 33% (95%CI 22% to 44%) on days following five or more servings of alcohol. This represents an adjusted absolute 13% (95%CI 1% to 24%) higher risk of having a headache on the day following 5 or more servings compared to no alcohol intake (p = .03).
Figure 2. Adjusted marginal absolute risk of having a migraine headache on the day following alcohol consumption among 98 participants with episodic migraines followed for 6 weeks. The observed adjusted estimates of absolute risk for each number of servings of alcohol are shown with the circles and vertical lines (95% confidence intervals).
We observed similar results in secondary analyses that further accounted for daily changes in caffeinated beverage intake, stress, sleep duration, self-reported physical activity, actigraphs-based levels of total activity time, and menstrual bleeding. The results were also not meaningfully different in sensitivity analyses that reclassified headaches on consecutive days as single events; excluded participants using migraine prophylaxis medications; excluded headaches classified as unlikely to be migraines; excluded headaches that were not similar to usual migraine headaches; or headaches that began while participants were asleep.
There was no evidence that the association varied by self-reported typical frequency of alcoholic beverage intake at baseline of <3 versus ≥3 servings per week (p-interaction = 0.96); whether the participant typically experiences visual aura before headache (p-interaction = 0.72); or whether the participant believes that alcohol triggers the onset of their migraines (p-interaction = 0.68).
Discussion
In this within-person analysis of a prospective cohort study, there was no association between 1–2 servings of alcoholic beverages and the odds of headaches on the following day, but intake of five or more servings was associated with 2.1-fold higher odds of headaches on the following day, even after accounting for potential confounding by other potential triggers. In terms of adjusted absolute risk, there was a 20% risk of headaches on the day following no alcohol intake, and a 33% risk of headaches on the day following five or more servings of alcoholic beverages.
Most prior studies asked participants about potential triggers after their migraines occurred rather than prospectively reporting lifestyle factors and any subsequent headaches. This may have led to recall bias since participants may over-report behaviours immediately preceding migraines in an attempt to find causes for their migraine attacks even though they are often exposed to these potential triggers in daily life with no ensuing migraine [Citation16–19]. In this study, we prospectively collected information on alcohol and other lifestyle factors and examined their potential impact on headache risk on the following day, eliminating concerns of recall bias.
The exact mechanism linking alcohol and headaches is unclear, although several theories have been proposed [Citation20]. Ethanol may directly induce headaches via its metabolite, acetate, which increases the formation of extracellular adenosine and thereby induces pain via stimulation of adenosine A2A [Citation21]. Alternatively, ethanol may trigger the release of calcitonin gene-related peptide from perivascular sensory nerve terminals [Citation22]. Some have suggested that other substances found in alcoholic beverages such as tyramine and tannins may induce headache via changes in serotonin [Citation23], although evidence is limited [Citation4,Citation24,Citation25]. It is also possible that headaches are attributable to the dehydration, worsened mood, stress, heavy food consumption, or sleep disruption associated with an alcohol hangover state [Citation26]. Our findings of heightened risk on the day following alcohol intake remained evident in analyses adjusted for daily changes in stress, sleep, and activity, but we cannot rule out the potential for residual time-varying confounding. Whereas some studies report that any alcoholic beverage can be deleterious [Citation5], others suggest that red wine, but not other types of alcohol, triggers migraines [Citation24]. We did not ask participants what type of alcohol they consumed, so we could not examine whether the association varies between wine, beer, or liquor.
According to the third edition of The International Classification of Headache Disorders [Citation2], alcohol hangover headaches are secondary headaches that occur several hours following alcohol consumption regardless of headache history. Among people with migraine, alcohol may trigger headaches with symptoms that are similar to their usual migraine attacks [Citation4] and they may occur as rapidly as 30 min after even small amounts of alcohol intake [Citation5]. We did not collect data on the time of day that participants consumed alcohol, so we cannot estimate the average time between consumption and potential headache onset and we cannot distinguish between migraines headaches and immediate and delayed alcohol-induced headaches. However, in an analysis restricted to the 580 headaches that participants reported as similar to their usual migraines, the results were not meaningfully altered. Regardless of whether these are alcohol-induced headaches or migraines triggered by alcohol, the association between heavy alcohol consumption and headaches in our study suggests that lowering alcohol consumption to moderate levels may be beneficial. This is concordant with dietary guidelines, recommending that if alcohol is consumed, it should be in moderation—up to 1 drink per day for women and up to 2 drinks per day for men [Citation27].
By comparing alcohol consumption with the risk of headache on the following day rather than the same day, we eliminated concerns of reverse causation whereby migraine symptoms impact subsequent alcohol intake. Furthermore, if prodromal symptoms led participants to lower their intake, we would have expected to observe an inverse association between alcohol intake and migraine headaches rather than the observed heightened risk on days following three or more servings of alcoholic beverages.
There is likely to be inter-individual variability in the susceptibility to alcohol-induced headaches, and individual risk may vary by genetics, hormones, or other factors that may interact with the risk of a headache. Further research is needed to examine the potential heterogeneity in risk and headache intensity across individuals and to assess how this risk may depend on the timing and amount of alcoholic beverage intake.
Conclusions
Even after accounting for day of week, daily caffeine intake, physical activity, and sleep, 1–2 servings of alcoholic beverages were not associated with a headache on the following day, but 3 or more servings may be associated with a higher risk of headache.
| Abbreviations | ||
| SD | = | standard deviation |
| CI | = | 95% confidence interval |
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):459–480.
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders. Cephalalgia. 2018. 38(1):1–211.
- Panconesi A, Bartolozzi ML, Guidi L. Alcohol and migraine: what should we tell patients? Curr Pain Headache Rep. 2011;15(3):177–184.
- Dueland AN. Headache and alcohol. Headache. 2015;55(7):1045–1049.
- Panconesi A. Alcohol and migraine: trigger factor, consumption, mechanisms. A review. J Headache Pain. 2008;9(1):19–27.
- Park JW, Chu MK, Kim JM, et al. Analysis of trigger factors in episodic migraineurs using a smartphone headache diary applications. PloS One. 2016;11(2):e0149577.
- Davis-Martin RE, Polk AN, Smitherman TA. Alcohol use as a comorbidity and precipitant of primary headache: review and meta-analysis. Curr Pain Headache Rep. 2017;21(10):42.
- Onderwater GLJ, Oosterhout WPJ, Schoonman GG, et al. Alcoholic beverages as trigger factor and the effect on alcohol consumption behavior in patients with migraine. Eur J Neurol. 2019;26(4):588–595.
- Bertisch SM, Li W, Buettner C, et al. Nightly sleep duration, fragmentation, and quality and daily risk of migraine. Neurology. 2020;94(5):e489–e496.
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381.
- Kosinski M, Bayliss MS, Bjorner JB, et al. A six-item short-form survey for measuring headache impact: the HIT-6. Qual Life Res. 2003;12(8):963–974.
- Patel SR, Weng J, Rueschman M, et al. Reproducibility of a standardized actigraphy scoring algorithm for sleep in a US Hispanic/Latino population. Sleep. 2015;38(9):1497–1503.
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–1070.
- Buysse DJ, Thompson W, Scott J, et al. Daytime symptoms in primary insomnia: a prospective analysis using ecological momentary assessment. Sleep Med. 2007;8(3):198–208.
- Allison PD. Fixed effects regression methods for longitudinal data using SAS. Cary, NC: SAS Institute; 2005.
- Baldacci F, Vedovello M, Ulivi M, et al. How aware are migraineurs of their triggers? Headache. 2013;53(5):834–837.
- Lipton RB, Pavlovic JM, Haut SR, et al. Methodological issues in studying trigger factors and premonitory features of migraine. Headache. 2014;54(10):1661–1669.
- Hougaard A, Amin FM, Hauge AW, et al. Provocation of migraine with aura using natural trigger factors. Neurology. 2013;80(5):428–431.
- Varkey E, Gruner Svealv B, Edin F, et al. Provocation of migraine after maximal exercise: a test-retest study. Eur Neurol. 2017;78(1–2):22–27.
- Panconesi A. Alcohol-induced headaches: evidence for a central mechanism? J Neurosci Rural Pract. 2016;7(2):269–275.
- Fried NT, Elliott MB, Oshinsky ML. The role of adenosine signaling in headache: a review. Brain Sci. 2017;7(3):30.
- Nicoletti P, Trevisani M, Manconi M, et al. Ethanol causes neurogenic vasodilation by TRPV1 activation and CGRP release in the trigeminovascular system of the guinea pig. (1468-2982 (Electronic)). Cephalalgia. 2008;28(1):9–17.
- Schnedl WJ, Queissner R. Migraines appear more likely to be caused by histamine than ethanol. Eur J Neurol. 2019;26(9):e79.
- Littlewood JT, Gibb C, Glover V, et al. Red wine as a cause of migraine. Lancet. 1988;331(8585):558–559.
- Marmura MJ. Triggers, protectors, and predictors in episodic migraine. Curr Pain Headache Rep. 2018;22(12):81.
- Tipple CT, Benson S, Scholey A. A review of the physiological factors associated with alcohol hangover. Curr Drug Abuse Rev. 9(2):93–98.
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. . 2015– 2020 Dietary Guidelines for Americans. 8th ed. December 2015. Available from: https://health.gov/our-work/food-nutrition/2015-2020-dietary-guidelines/guidelines/appendix-9/
