Abstract
Aim: The aim of this systematic review and meta-analysis was to identify, evaluate, and synthesize the evidence from studies that have investigated the treatment effect via telemedicine interventions on depressive symptoms, quality of life, and work and social functioning in patients with depression.
Methods: Six electronic databases (MEDLINE [1916–2021], PubMED [1950–2021], PsycINFO [1971–2021], Scopus [2004–2021], Embase [1972–2021], and CINAHL [1937–2021]) were systematically searched in March 2021. Reference lists of identified articles were hand searched. Randomized controlled trials were included if they investigated the treatment effects via telemedicine interventions in patients who had a depression diagnosis. Quality assessment was evaluated using the critical appraisal checklists developed by the Joanna Briggs Institute.
Results: Seventeen (17) trials (n = 2,394) met eligibility criteria and were included in the analysis. Eleven (11) randomized controlled trials shared common outcome measures, allowing meta-analysis. The results provided evidence that treatment via telemedicine interventions were beneficial for depressive symptoms (standardized mean difference= −0.44; 95% CI= −0.64 to −0.25; p < .001) and quality of life (standardized mean difference= 0.25, 95% CI −0.01 to 0.49, p = .04) in patients of depression. There were insufficient data for meta-analysis of work and social functioning.
Conclusion: This study showed the positive effects of treatment via telemedicine interventions on depressive symptoms and quality of life in patients with depression and supported the idea for clinical practice to establish a well-organized telepsychiatry system.
Telemedicine is effective at reducing symptoms of depression.
Telemedicine can improve quality of life in persons with depression.
KEY MESSAGES
Introduction
The term ‘telemedicine’ encompasses the use of technology to deliver clinical care at a distance. It ensures that people with limited access to care receive help when they need it [Citation1]. With the advancement of telecommunication techniques, telemedicine has gradually been adapted by clinicians [Citation2] to care for people who live at a distance from medical facilities, have weak social networks, and/or are unable to leave their homes for a medical appointment.
Depressive disorder is the leading contributor to the global health-related burden [Citation3]. The risk factors include adversity, personality, neuroticism, and substance abuse. Depression is a mental and behavioral disorder that causes people to experience anhedonia. Symptoms are sadness, cognitive difficulties, changes in appetite, and sleep disorders. These symptoms reduce patients’ quality of life [Citation4,Citation5] and work and social functioning [Citation6,Citation7].
During the outbreak of the COVID-19 pandemic, health services accelerated the global use of telemedicine. Numerous studies have revealed the advantages of telemedicine, such as reducing healthcare expenditure, improving the efficiency of healthcare delivery, and producing good clinical outcomes [Citation8]. Patients with depression require regular mental consultation and deprescribing. Telemedicine is widely adapted in depression care [Citation9] and for acute medical conditions in psychology practice [Citation10–14]. Recent systematic review has reported the effectiveness of video-based psychotherapy in reducing depressive symptoms compared with in-person services [Citation15]. However, an important literature gap still exists in terms of the treatment effects via telemedicine interventions quality of life and work and social functioning in patients with depression.
This study aimed to evaluate the treatment effects via telemedicine interventions on depressive symptoms, quality of life, and work and social functioning in patients with depression. The present outcomes will provide a reference for psychological practices, to improve the quality of care for patients with depression.
Methods
This systematic review is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement [Citation16]. A protocol for this review was registered on the PROSPERO International prospective register of systematic reviews (Registration No. PROSPERO CRD42021264916).
Six electronic databases (MEDLINE 1916-2021, PUBMED 1950-2021, PsycINFO 1971-2021, SCOPUS 2004-2021, EMBASE 1972-2021, and CINAHL 1937-2021) were searched in March 2021 using combinations of the following terms including American English/British English spelling variations, prefixes/suffixes, and pluralization: depression; depressive disorder; depressive symptoms; telemedicine; telehealth; telepsychiatry; telepsychology; telemental health; digital mental health interventions; web-based information and communication technology; digital psychological intervention; digital communication devices; websites; SMS text messages; emails; smartphone apps; videos; audio files; computer programs; live video; videoconferencing; Symptoms of mental illness; well-being; function; quality of life. Electronic databases were accessed through Asia University, Taiwan. The publication dates or language were not restricted. An example of search strategy is presented as online supplementary material. The additional articles were searched by the reference lists of identified articles.
Two reviewers (JYW, YHS) independently assessed the titles/abstracts of studies for inclusion. Then, full texts of potential studies were screened to determine eligibility by two reviewers (JYW, YHS). Discrepancies between the two reviewers in the study selection processes were discussed for agreement, and a third reviewer (KHL) was consulted if necessary. The criteria for considering studies for this review were the following:
Types of studies
We included randomized controlled trials (RCTs) (including cluster and cross-over trials). Studies published in English were included. Studies published in non-peer reviewed journals, conference abstracts, letters to the Editor, any forms of literature review, and case studies were excluded.
Types of participants
Any patients and populations with a depression diagnosis (as diagnosed using any recognized diagnostic criteria) were included.
Types of interventions
According to the World Health Organization (WHO), telemedicine is defined as ‘the delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.’ [Citation17]. We considered all types of telemedicine interventions (including telephone, smartphone, internet-based). Acceptable control interventions were usual care, placebo treatment or wait list controls. We excluded studies in which the control group had, or might have received telemedicine treatments.
Types of outcome measures
Patient-reported outcome measures of depressive symptoms or quality of life, or work and social functioning were included.
Data extraction and quality assessment were undertaken independently by two reviewers (JYW, YHS) and cross-checked by a third independent reviewer (KHL). The following data items were extracted from included studies: author’s name; year of publication; author and year of publication, country of study, study subject, sample size, intervention group, control group, duration, frequency, outcome measures, and results of outcome measures. Where trial data were not reported or in a form that could not be used in the formal comparisons, we sought further clarification by contacting the authors of included studies. All included trial data were extracted and processed as described in the Cochrane Handbook for Systematic Reviews of Interventions [Citation18]. Methodological quality and bias of each included study was assessed utilizing the critical appraisal checklists developed by the Joanna Briggs Institute (JBI) [Citation19]. JBI critical appraisal checklist for randomized controlled trials have 13 items, and each item was scored as ‘yes’, ‘no’, ‘unclear’, and ‘not applicable.’ Any disagreements were resolved through discussion.
SPSS for Windows statistical software package (SPSS Inc., Version 25, Chicago, IL, USA) was used to analyze the Kappa statistics and agreement, which represented the agreement between reviewers for study selection and quality assessment [Citation20]. Values of the Kappa greater than 0.75 were indicated excellent agreement [Citation18]. Meta-analyses were performed in Review Manager (Review Manager (RevMan) Version 5.3. to identify the treatment effect via telemedicine intervention. Only studies which provided pre- and post-intervention data and evaluated outcome of interest in at least two RCTs were included for meta-analysis. Cochran’s Q test and I2 were used to assess the heterogeneity among the included studies. The Mantel-Haenszel methods with a fixed-effects model was used in the meta-analyses to pool data from different studies. If heterogeneity was statistically significant (Chi2 test, p < .05) or I2>50%, a more conservative random-effects model was suggested for meta-analysis [Citation18]. The standardized mean differences and 95% confidence intervals (CIs) were computed when the outcome of included studies measured on the different scales. Forest plots were provided to display the mean differences and 95% CIs in the measures between the intervention and control groups. A p-value < .05 was considered statistically significant.
Results
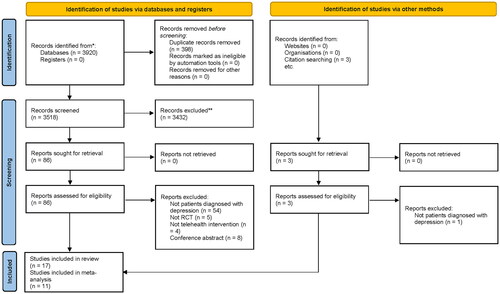
presents the PRISMA flow diagram of study selection process. The search of six electronic databases generated 3,920 studies and three additional studies. After removal of duplicate and assessment of eligibility of articles, 17 studies were included for final review, of which 11 studies were entered into meta-analyses. Kappa statistics and agreement between two reviewers on title/abstracts and full text were 0.81 (90% agreement) and 0.73 (84% agreement), respectively. The quality of included studies evaluated by the JBI critical appraisal checklist is shown in online supplementary material.
Seventeen RCTs studies were included, and study characteristics are shown in . All included studies were published between 2000 and 2020 and written in English. The geographical distribution revealed that of the included studies, eight were conducted in the USA [Citation10,Citation11,Citation22,Citation25,Citation28,Citation31–33], three in Germany [Citation12,Citation13,Citation24], one in Canada [Citation21], one in Korea [Citation23], one in Spain [Citation26], one in Australia [Citation27], one in Chile [Citation29], and one in Sweden [Citation30].
Table 1. Participants and intervention programs in reviewed randomized controlled trials.
The characteristics of participants in the included studies are shown in . Ten of the seventeen studies only included participants with diagnosed depression [Citation10,Citation11,Citation21,Citation22,Citation24,Citation29–33]. Four studies recruited participants with comorbid depression and certain diseases, including diabetes mellitus [Citation27], active epilepsy [Citation13], breast cancer [Citation23], or Parkinson’s disease [Citation28]. Two studies included a mixed cohort of participants with depression or dysthymia [Citation12,Citation26]. One study included participants with varying mental health and physical diagnoses [Citation25]. A total of 2,394 participants were included in the RCTs. Among them, 1,286 participants were allocated to the intervention groups, and 1,108 were allocated to the control groups.
All studies included interventions with some forms of telemedicine, and control interventions included usual care [Citation10,Citation11,Citation13,Citation22,Citation23,Citation25,Citation27,Citation30], enhanced usual care [Citation26,Citation28,Citation29], placebo treatment [Citation31], face-to-face behavioral activation [Citation32,Citation33], and waitlist controls [Citation12,Citation21,Citation24]. The frequency and duration of the intervention programs varied between the studies (). Three studies provided internet cognitive behavioral therapy (ICBT), which was based on a structured web-based CBT approach with strong emphasis on behavioral activation [Citation13,Citation27,Citation30]; three studies provided video/mobile game interventions [Citation12,Citation23,Citation31]; two studies provided internet-based psychological intervention programmes, which included structured interactive sessions [Citation24] and interactive therapeutic modules [Citation26]; two studies used in-home videoconferencing operating via the standard telephone service [Citation32,Citation33]; one study provided a Webcam intervention (Internet videoconferencing), which consisted of six monthly Webcam sessions with the psychiatrist [Citation10]; one study provided telephone-based cognitive-behavioral treatment (T-CBT), which comprised telephone-based coaching in how to support and encourage the use of new CBT coping skills between therapy sessions [Citation28]; one study provided remote collaborative depression care (RCDC), which consisted of a 3-month treatment that included continuous remote supervision by psychiatrists through shared electronic health records (SEHR) and phone patient monitoring [Citation29]; one study provided online spirituality informed e-mental health intervention, which was an eight-week online program consisted of eight module to guide participants through an exploration of spiritually informed principles [Citation21]; one study provided nurse telehealth care, which consisted of emotional support and focused behavioral interventions in ten 6-minute calls during 4 months by primary care nurses [Citation22]; one study provided telepsychiatry-based culturally sensitive collaborative treatment (T-CSCT), which included the teleconferencing technology and added a cultural component to the collaborative care model [Citation11]; and one study provided a 6-month usual care plus the mobile monitoring system intervention, which asked participants to downloaded the mobile monitoring application to their smartphones [Citation25]. The length of interventions and follow-up duration ranged from three weeks to 12 months.
The outcome measurements were varied across the seventeen studies. Depressive symptoms were examined in most studies (n = 16/17) and measured using Patient Health Questionnaire–9 [PHQ-9] (n = 7) [Citation10,Citation12,Citation13,Citation24,Citation26,Citation27,Citation31], Beck Depression Inventory [BDI]/[BDI-II] (n = 8) [Citation12,Citation22–24,Citation28–30,Citation32], Hamilton Depression Rating Scale [HAM-D] (n = 5) [Citation11,Citation21,Citation22,Citation28,Citation31], Children’s Depression Rating Scale Revised [CDRS-R] (n = 1) [Citation21], Neurological Disorders Depression Inventory for Epilepsy [NDDIE] (n = 1) [Citation13], Depression Anxiety Stress Scales–21 [DASS-21] (n = 1) [Citation13], Geriatric Depression Scale [GDS] [Citation32], and MADRS, Montgomery-Asberg Depression Rating Scale [MADRS] (n = 1) [Citation10].
Fifty-eight percent of included studies (n = 10/17) measured self-reported quality of life. Five studies assessed health-related quality of life and functioning using the Short-Form Health Survey [SF-12/SF-36] [Citation22,Citation26–28,Citation33]. Two studies also assessed quality of life using the Quality of Life Enjoyment and Satisfaction Questionnaire [Q-LES-Q] [Citation10,Citation11]. One study evaluated health-related quality of life in people with epilepsy using the Quality of Life in Epilepsy–10 items [QOLIE-10] [Citation13]. One study assessed health-related quality of life in adolescents using the KIDSCREEN-27 [Citation29]. Two studies measured quality of life using the EuroQol-5 Dimension [EQ-5D] [Citation30] and EuroQol-Visual Analogue Scale [EQ-VAS] [Citation26], respectively. Only one of the seventeen studies assessed work and social function outcome, and this was undertaken using the Work and Social Adjustment Scale [WSAS] [Citation13], which was designed to measure patients’ perceived functional impairment resulting from a health problem.
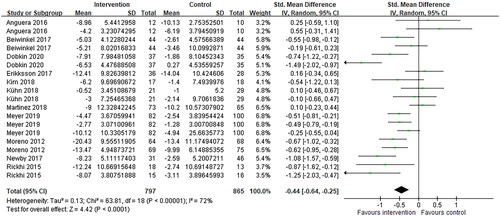
Study results are shown in . Meta-analysis of the depressive symptoms outcomes after treatment via telemedicine intervention showed a significant improvement in depression scores after intervention compared to control. There was a trend towards improved depressive symptoms (standardized mean difference = −0.44; 95% CI= −0.64 to −0.25; p < .001). Statistical heterogeneity was present in the comparison between telemedicine and control groups (I2 = 72%; p < .001) ().
Table 2. Summary of results on outcome measures in reviewed studies.
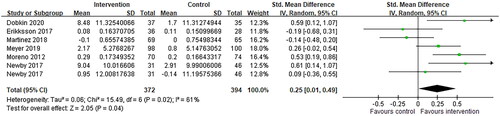
shows a Forest plot for included studies reporting the effect size estimate for treatment via telemedicine interventions on quality of life. Pooling results across studies showed a significant trend toward improved quality of life compared to controls. The standardized mean difference was 0.25 (95% CI −0.01 to 0.49, p = .04). There was an evidence of statistical heterogeneity (I2 = 61%; p = .02) ().
Insufficient data were provided for meta-analysis of work and social functioning. Only study conducted by Meyer et al. included work and social functioning as one of its outcome measures; thus, this outcome was not included in the meta-analysis [Citation13]. Meyer et al. showed that the intervention group produced clinically significant effects on improvements in social‐occupational impairment, which exceeded improvements observed among control group [Citation13].
Discussions
This study included seventeen articles from six databases regarding the outcome effects of treatment via telemedicine intervention on individuals with depression, and data from eleven articles were extracted for meta-analysis. The forest plot revealed that depressive symptoms improved and quality of life was elevated after the intervention. One of the eligible articles showed evidence that telemedicine improves patients’ social-occupational impairment. Our meta-analysis demonstrated that telemedicine was beneficial in improving depressive symptoms and quality of life in patients with depression. The outcomes of this study support the advantages of telemedicine application in individuals with depression and the concept of clinical practice, establishing a well-organized telepsychiatry system.
The possible reasons for positive outcomes of treatment via telemedicine for patients with depression include the following. First, telehealth increases patients’ access to professional help for depression [Citation34]. Common barriers to getting professional help include lack of time, transportation, or the availability of providers in a patient’s local area. Second, treating depression virtually appears to be just as effective as in-person visits [Citation35]. Healthcare providers can easily monitor patients’ clinical conditions by adjusting medication, addressing non-adherence, or providing additional psychotherapy to enhance the quality of patient care [Citation36]. Third, virtual visits were more comfortable. Patients may feel more at ease during an online psychiatrist appointment than during an in-person interview, especially those with severe depression [Citation14].
Telemedicine has advantages and disadvantages for healthcare. Telemedicine benefits patients who live far from healthcare facilities. It also brings benefits to healthcare professionals, who can provide prompt service during patients’ acute conditions and manage patients’ long-term chronic diseases. On the other hand, home-based telemedicine may increase the burden on family caregivers. Family members and patients take more responsibility, and there is greater risk of error in a do-it-yourself homecare scenario. This burden may compel patients and caregivers to seek alternative options for medical services. In addition, telemedicine breaks the boundary between a patient’s public and private life, which affects the significance of the home [Citation37]. Telemedicine lacks the quality of face-to-face human contact. The position of the camera affects the angle of view, unlike face-to-face consultation, which involves facing each other and affects the patient-physician relationship and healthcare quality.
Modern technologies must fill the gaps and limitations in current practice. The future generation of psychiatrists must recognize that the fundamental practice of psychiatry remains based on the patient-physician connection and be aware of the ethical issues and quality of treatment. Physicians must consider an individualized treatment process according to the patient’s characteristics. Therefore, developing a guideline and assessment tool for the quality of care, going beyond the clinical benefit and health outcomes, is needed [Citation38–40].
This study has several limitations. First, the articles excluded patients with suicidal ideation or severe depression. Therefore, the outcome of telemedicine is limited to individuals with mild and moderate depression. Second, we included articles only in English and excluded theses and conference papers, which may have caused language and publication bias. Third, the heterogeneity in the intervention and control groups, regarding program content and duration of the telemedicine components, and statistical heterogeneity in the meta-analyses may limit the interpretation of the results. Fourth, due to the lack of outcome measure data in the RCTs, meta-analysis was limited to eleven studies, which may have affected the strength of the conclusions drawn. This review is further limited by the moderate risk of bias, as most included studies suffer inevitable limitations of blinding patients and assessors to the treatment conditions.
Conclusion
Treatment via telemedicine intervention improved the quality of life and ameliorated the depressive symptoms in patient with mild to moderate depression. Future studies should incorporate with consistent use of telemedicine program and duration of the telemedicine components, given the robust evidence to support the treatment effect via telemedicine intervention in this population.
Ethical approval
This is a review study, and no ethical approval is required.
Author contributions
Yin-Hwa Shih: Methodology, Data curation, Writing- Original draft preparation, Writing- Reviewing and Editing. Jiun-Yi Wang: Conceptualization, Investigation, Methodology, Software, Writing- Original draft preparation. Po-Han Chou: Methodology, Data curation, Writing- Original draft preparation, Writing- Reviewing and Editing. Kuan-Han Lin: Methodology, Supervision, Software, Validation, Writing- Original draft preparation, Writing- Reviewing and Editing. All authors read and approved the final manuscript.
Supplemental Material
Download MS Word (56 KB)Supplemental Material
Download MS Word (30.5 KB)Acknowledgments
The authors have no acknowledgments to report.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data are available to investigators after request.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Bashshur R, Shannon G, Krupinski E, et al. The taxonomy of telemedicine. Telemed J E Health. 2011;17(6):484–494.
- Sood S, Mbarika V, Jugoo S, et al. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed J E Health. 2007;13(5):573–590.
- Santomauro DF, Mantilla Herrera AM, Shadid J, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–1712.
- Brenes GA. Anxiety, depression, and quality of life in primary care patients. Prim Care Companion J Clin Psychiatry. 2007;9(6):437–443.
- Cho Y, Lee JK, Kim D-H, et al. Factors associated with quality of life in patients with depression: a nationwide population-based study. PLoS One. 2019;14(7):e0219455.
- Bosc M. Assessment of social functioning in depression. Compr Psychiatry. 2000;41(1):63–69.
- Kupferberg A, Bicks L, Hasler G. Social functioning in major depressive disorder. Neurosci Biobehav Rev. 2016;69:313–332.
- Boxer RJ, Ellimoottil C. Advantages and utilization of telemedicine. Mhealth. 2019;5:12.
- Echelard JF. Use of telemedicine in depression care by physicians: scoping review. JMIR Form Res. 2021;5(7):e29159.
- Moreno FA, Chong J, Dumbauld J, et al. Use of standard webcam and internet equipment for telepsychiatry treatment of depression among underserved hispanics. Psychiatr Serv. 2012;63(12):1213–1217.
- Yeung A, Martinson MA, Baer L, et al. The effectiveness of telepsychiatry-based culturally sensitive collaborative treatment for depressed chinese American immigrants: a randomized controlled trial. J Clin Psychiatry. 2016;77(08):e996–e1002.
- Kühn S, Berna F, Lüdtke T, et al. Fighting depression: action video game play may reduce rumination and increase subjective and objective cognition in depressed patients. Front Psychol. 2018;9:129.
- Meyer B, Weiss M, Holtkamp M, et al. Effects of an epilepsy‐specific internet intervention (emyna) on depression: results of the ENCODE randomized controlled trial. Epilepsia. 2019;60(4):656–668.
- Guaiana G, Mastrangelo J, Hendrikx S, et al. A systematic review of the use of telepsychiatry in depression. Community Ment Health J. 2021;57(1):93–100.
- Giovanetti AK, et al. Teletherapy versus in-Person psychotherapy for depression: a Meta-Analysis of randomized controlled trials. Telemed J E Health. 2022;28(8):1077–1089.
- Page MJ, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
- Telematics W. A health telematics policy in support of WHO'S Health-For-All strategy for global development: report of the WHO group consultation on health telematics 11-16 december, Geneva. 1998.
- Higgins J. Cochrane handbook for systematic reviews of interventions. Version 5.1. 0 The Cochrane Collaboration. 2011. www.cochrane-handbook.org
- The Joanna Briggs Institute. Critical Appraisal Tools. 2021. https://jbi.global/critical-appraisal-tools
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174.
- Rickhi B, Kania-Richmond A, Moritz S, et al. Evaluation of a spirituality informed e-mental health tool as an intervention for major depressive disorder in adolescents and young adults–a randomized controlled pilot trial. BMC Complement Altern Med. 2015;15(1):1–14.
- Hunkeler EM, Meresman JF, Hargreaves WA, et al. Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. Arch Fam Med. 2000;9(8):700–708.
- Kim SM, Kim H-J, Hwang HC, et al. The effects of a serious game on depressive symptoms and anxiety in breast cancer patients with depression: a pilot study using functional magnetic resonance imaging. Games Health J. 2018;7(6):409–417.
- Beiwinkel T, Eißing T, Telle N-T, et al. Effectiveness of a web-based intervention in reducing depression and sickness absence: randomized controlled trial. J Med Internet Res. 2017;19(6):e6546.
- Place S, Blanch-Hartigan D, Smith V, et al. Effect of a mobile monitoring system vs usual care on depression symptoms and psychological health: a randomized clinical trial. JAMA Netw Open. 2020;3(1):e1919403.
- Gili M, Castro A, García-Palacios A, et al. Efficacy of three low-intensity, internet-based psychological interventions for the treatment of depression in primary care: randomized controlled trial. J Med Internet Res. 2020;22(6):e15845.
- Newby J, Robins L, Wilhelm K, et al. Web-based cognitive behavior therapy for depression in people with diabetes mellitus: a randomized controlled trial. J Med Internet Res. 2017;19(5):e157.
- Dobkin RD, Mann SL, Gara MA, et al. Telephone-based cognitive behavioral therapy for depression in parkinson disease: a randomized controlled trial. Neurology. 2020;94(16):e1764–e1773.
- Martínez V, Rojas G, Martínez P, et al. Remote collaborative depression care program for adolescents in araucanía region, Chile: randomized controlled trial. J Med Internet Res. 2018;20(1):e38.
- Eriksson MCM, Kivi M, Hange D, et al. Long-term effects of internet-delivered cognitive behavioral therapy for depression in primary care–the PRIM-NET controlled trial. Scand J Prim Health Care. 2017;35(2):126–136.
- Anguera JA, Gunning FM, Areán PA. Improving late life depression and cognitive control through the use of therapeutic video game technology: a proof‐of‐concept randomized trial. Depress Anxiety. 2017;34(6):508–517.
- Egede LE, Acierno R, Knapp RG, et al. Psychotherapy for depression in older veterans via telemedicine: a randomised, open-label, non-inferiority trial. Lancet Psychiatry. 2015;2(8):693–701.
- Egede LE, Acierno R, Knapp RG, et al. Psychotherapy for depression in older veterans via telemedicine: effect on quality of life, satisfaction, treatment credibility, and service delivery perception. J Clin Psychiatry. 2016;77(12):1704–1711.
- Rafiq A, Merrell RC. Telemedicine for access to quality care on medical practice and continuing medical education in a global arena. J Contin Educ Health Prof. 2005;25(1):34–42.
- Osenbach JE, O'Brien KM, Mishkind M, et al. Synchronous telehealth technologies in psychotherapy for depression: a meta-analysis. Depress Anxiety. 2013;30(11):1058–1067.
- Salisbury C, O'Cathain A, Edwards L, et al. Effectiveness of an integrated telehealth service for patients with depression: a pragmatic randomised controlled trial of a complex intervention. Lancet Psychiatry. 2016;3(6):515–525.
- Bauer KA. Home-based telemedicine: a survey of ethical issues. Camb Q Healthc Ethics. 2001;10(2):137–146.
- Kidholm K, Clemensen J, Caffery LJ, et al. The model for assessment of telemedicine (MAST): a scoping review of empirical studies. J Telemed Telecare. 2017;23(9):803–813.
- Cowan KE, McKean AJ, Gentry MT, et al. Barriers to use of telepsychiatry: clinicians as gatekeepers. Mayo Clin Proc. 2019;94(12):2510–2523.
- Jha AK, Sawka E, Tiwari B, et al. Telemedicine and community health projects in asia. Dermatol Clin. 2021;39(1):23–32.