Abstract
Objectives
Community-based hospitals in China lack physicians, especially rehabilitation physicians. Recently, several financial resources have been developed to prepare general doctors for community-based hospitals. These doctors seem to be the best choices for assuming the role of a rehabilitation physician. However, their willingness and in-depth information from their perspectives have not been previously investigated.
Materials and methods
We conducted a general investigation of rehabilitation resources in Yunnan, a province located in Southwest China with a population of more than 40 million. Our investigation covered the entire Yunnan Province from December 2020 to May 2022. The questionnaire was administered to 670 general doctors in 112 community hospitals randomly selected in Yunnan Province based on their willingness to assume the role of rehabilitation physicians and obstructive factors to process the rehabilitation services. The reliability and validity of the questionnaire were evaluated, and items regarding their general condition were analyzed.
Results
Cronbach’s alpha and Kaiser–Meyer–Olkin values were 0.748 and 0.729, respectively. The measure comprises four factors: common disease, demand for training to improve skills, subjective/objective factors, and proactivity to recommend rehabilitation therapy. More than 20% of general doctors were unwilling to take on the role of rehabilitation physicians, and their willingness was related to satisfaction with their current job, comprehension of community-based rehabilitation, and comprehension of government support (p < .05).
Conclusions
From the perspective of general doctors, the reimbursement rate for medical insurance, which burdens patients, is the greatest problem in the process of developing community-based hospital rehabilitation services. Offering professional training to increase their capacity and developing common practices to increase doctors’ proactivity to recommend rehabilitation therapy may help increase the future support of medical insurance and increase general doctors’ willingness to take on the role of a rehabilitation physician.
Introduction
General practitioners(GPs) serve a large population in China. GPs include general practitioners (GPs), family doctors, and barefoot doctors in the southwestern area. General practices were introduced to China in the late 1980s [Citation1]. The phenomenon of barefoot doctors represents a distinctive feature of Chinese history. GPs and barefoot doctors alike offer primary healthcare services, with GPs catering to both urban and rural areas, while barefoot doctors primarily serve rural regions and need fewer qualifications to fulfill their roles effectively [Citation2]. A large cohort of GPs have been developed over the last two decades with the support of the government. However, the quantity and quality of GPs in China has been questioned over the years and the number of qualified GPs is still lacking [Citation3,Citation4].
Their lower cultural and service levels have been criticized in several studies, and some researchers believe that GPs should have various skills to provide better services to community residents [Citation5].
Some studies have suggested that job transfer training for creating GPs can be detrimental to hierarchical diagnosis and treatment [Citation3]. The working conditions and the attractiveness of becoming a GP have improved in recent years, and the government has facilitated several policies to increase the population of GP and has achieved some results. However, the quality and allocation of GPs are unbalanced and large regional differences exist in China [Citation6].
A preliminary survey showed that 107 community health service centers in Shanghai City have 325 licensed physicians, 37 of whom are rehabilitation physicians (11.38%) [Citation7]. However, in Yunnan Province, of 90 randomly selected community health service hospitals, only 42 were licensed physicians, and only 2.51 (5.97%) were licensed rehabilitation physicians. Both physicians and rehabilitation physicians are lacking in Southwest China; however, supplementing this population by training a large number of doctors is impossible in China.
The outbreak of the coronavirus disease (COVID-19) pandemic from 2019 to 2023 has brought both opportunities and unprecedented job burnout to physicians in China. In particular, GPs provide first-line healthcare services. A previous study, conducted in 2021, reported that the careers of Chinese GP trainees improved after the COVID pandemic. With prolonged anti-pandemic working durations, behavioral abnormalities, especially job burnout, are common among medical staff. However, with the declaration of an anti-pandemic victory, the focus of public opinion was again on the GP population, which was referred to as the guardian of health.
A previous study reported that more than 19% of the elderly population in China had asymptomatic lacunar infarction, which may cause dementia and require increased home- or community-based medical rehabilitation care services. The exclusion of patients clearly diagnosed is concerning, and has already created a significant burden on national medical insurance whether service providers were prepared to provide health services for these potential cognitively impaired populations or not [Citation8].
It has been proposed that based on population distribution, health resources should increase the number of services providers in the Eastern region, but more attention should be paid to improving the uptake rate in the sparsely populated Western regions of China [Citation9]. In other words, GPs in the southwestern region should assume more roles as specialty physicians.
Considering economic and realistic factors, training the GP population to take on the role of rehabilitation physicians in community-based hospitals seem to be the simplest and quickest way to reduce training input.
However, to the best of our knowledge, no study has investigated whether GPs, at least GPs in Southwest China, are willing to take on the role of community rehabilitation physicians. In summary, no study has attempted to investigate what factors hinder the process of community rehabilitation services from a GPs perspective. Therefore, this study aimed to investigate GPs working in a community-based hospital in Yunnan Province. We also investigated problems in the process of community rehabilitation services.
Material and methods
This cross-sectional study was derived from a subtopic of the study guided by a local government agency. This study was approved by the Institutional Review Board of this study ((PJ-2020-67(1)). As a local people’s wellbeing related study, this study also received support from a non-profit, the Norway Cooperation Association organization.
Sample and data collection
Data were collected and analyzed from December 2020 to May 2022 in Yunnan Province, Southwest China. A total of 112 institutions were randomly selected from among all institutions under the management of the Yunnan Healthcare Commission, including community health services and health centers. 710 GPs affiliated with these institutions received an advanced information e-mail or call, which included the aims, benefits, and agency of the questionnaire. We also emphasized that participation was voluntary, that participants were randomly selected, and that they could withdraw from the study without a reason. 670 GPs provided consent to participate in the questionnaire survey. 10 volunteers completed pre-questionnaire training and visited 11 cities, 51 towns, and 11 districts to complete 670 face-to-face surveys. The data pertaining to the experience of GPs in delivering community-based rehabilitation services were acquired via our questionnaire and subsequently collected and organized using Microsoft Excel software.
Questionnaire design
A pilot study was conducted at 12 community hospitals to assess the comprehensiveness, feasibility, and scientific basis of the questionnaires. Experts’ opinions on the interview guide and questionnaire were processed before and after the pilot study to improve the quality of the questionnaire. After modification based on previous testing, the questionnaire included 13 general items related to factors hindering the process of community-based rehabilitation services, and 13 items related to other conditions.
Measurements
Data were collected through a face-to-face survey by volunteers trained in the Yunnan Sanitation and Health Commission (SHC) project. Following data collection, 10% of the questionnaires were randomly chosen to assess the test-retest reliability.
Statistical analysis
IBM SPSS software version 26.0 and AMOS software version 26.0 were employed for validity and reliability analyses. Confirmatory factor analysis was used to examine validity and Cronbach’s alpha was used to examine internal consistency reliability. Questionnaire items were deleted if they did not meet al.pha coefficient < 0.70, Kaiser-Meyer-Olkin (KMO) value < 0.60, or Bartlett’s value < 0.05. Chi squared, degrees of freedom, the goodness of fit index, root mean square error of approximation, root mean square residual, comparative fit index, normed fit index, and Tucker-Lewis index were used to confirm the structural model. The different between GPs willing to take on or did not want to take on the role of rehabilitation physician were used Pearson Chi-squared, Fisher’s exact test, or linear by linear test and the value of p < .05 was considered statistically significant.
Results
Demographic and clinical characteristics
73 target cities, towns, and districts included 112 community-based hospitals and 670 doctors. All institutions registered at least one doctor, and the mean number of registered doctors was 5.98 (with a minimum of one and a maximum of 26 doctors). Each doctor treat more than 500 patients per month. The mean age was 38.65 ± 8.09 and their educational degree concentrated on college school levels. Most doctors’ practice ranges were GPs; however, others were dispersed across several other ranges.
All questionnaires were completed and returned (valid return rate: 100%). The demographic characteristics of the doctors are presented in . The mean age of the GPs in our study was 38 years old, and most of them had college diplomas. Rehabilitation accounted for only 0.9% of their practice.
Table 1. Demographic characteristics of the general doctors in community-based hospital.
Reliability and validity
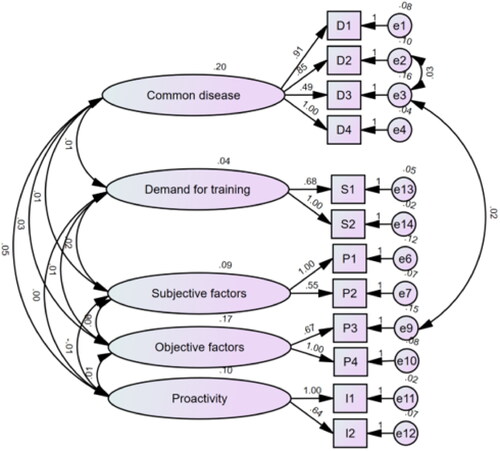
Cronbach’s alpha coefficient for the total questionnaire was 0.748. The Kaiser-Meyer Olkin value was 0.729, indicating that the data were suitable for factor analyses. Bartlett’s test of sphericity value was 2693.445 (p < .000), indicating that the extraction of common factors could explain most of the statistical information represented by the questionnaire items. Four common factors with eigenvalues >1 were extracted by principal components analysis, which explained 63.071% of the variance. Using the orthogonal rotation method, the factor loadings of each item on its dimensions ranged from 0.541 to 0.877. The factor and item factor loadings are listed in . These factors were named common diseases, ‘subjective/objective factors,’ ‘proactivity’, and ‘demand for training’. According to the factors extracted from the comprehensive results, the prevailing diseases identified by GPs in community medical care settings included sequelae of brain damage, cerebral palsy, dysplastic disease, chronic pain, and trauma. Furthermore, our study reveals that these GPs perceive challenges in delivering community-based rehabilitation services primarily due to factors such as a low rate of medical insurance reimbursement, financial constraints faced by patients, limited opportunities for professional development, and low wages. The proactivity of referral rehabilitation service was categorized into rehabilitation therapy and referral to other rehabilitation hospital options. In our study, the GPs requested training that enhances their knowledge of new advancements, as well as medical and surgical expertise.
Table 2. Factor loading matrix after rotation in the general doctor’s questionnaire.
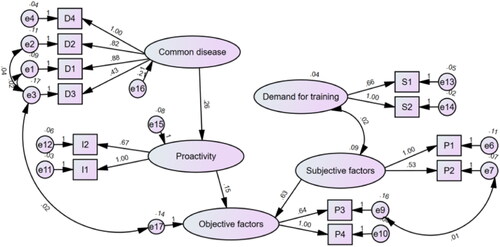
SEM path analysis
Convergent validity in the initial structural model was not ideal; therefore, the model was modified according to government policy, convergent validity, and modification indices. Considering the covariance, correlation estimate, and p-value, the common disease 5 factor was removed, and the subjective and objective factors were separated. After this modification, the fit indices of the final model were within acceptable ranges. See for the fit indices before and after modification, and we found the fitting indexes to be more acceptable after modification than before.
Table 3. Fitting indexes before and after the model modification.
The results of the path analysis were structural models before modification, as shown in . Although the regression weight in most factors was more than 0.5, models were modified by modification indices and theory, as is shown in , and after modification, the regression weight in most factors was suitable. The demand for training and subjective factors were associated with each other. Objective factors seem to be directly affected by subjective factors and proactivity but are indirectly affected by common diseases and demand for training.
Other important results based on the questionnaire responses
Among the 670 general doctors, more than 20% (140) were unwilling to assume the role of a rehabilitation physician. Among them, the doctors willing to take on the role seemed more satisfied with their current job and better understood the concept of community rehabilitation. Contrastingly, the doctors who did not want to take on the role did not seem to have understood the support policy for community-based hospitals (p < .05) ().
Table 4. The different between willing to take on or did not want to take on the role of rehabilitation physician.
Discussion
Chinese healthcare service faces an unprecedented strain as the population ages [Citation10]. The community-based healthcare model explicitly matches the Chinese local environment, which is at the forefront of primary healthcare and played an important role during the COVID-19 pandemic [Citation11]. In recent years, large financial resource investments and infrastructure building projects have been undertaken to improve medical community healthcare services. The primary form of facilitation was the cultivation of many GPs, who may be the most suitable choice to assume the role of community-based rehabilitation physician.
In China, the basic medical and health care system comprises four major systems: the health security system, with the majority of medical insurance; the primary medical and health care system with the majority of community-based health care services; the public health system with the majority of disease prevention; and the drug-regulatory system. We found that, aside from the last term, all three major systems were related to the scope of primary healthcare providers. This means that the launch of medical reform, which is the main form of building the primary healthcare system, could not be separated from GPs, who are the main component of community-based services. Some existing research [Citation12] also targeted primary healthcare providers and recommended that comprehensively improving the skills of GPs could address most problems existing in health inequalities and population aging.
Research on the work stability of family doctors in Shanghai showed that, as gatekeepers of residents’ health, their work competency and stability depends on job satisfaction [Citation13]. This is consistent with our research finding that the willingness to assume the role of rehabilitation physicians in Yunnan Province was related to job satisfaction.
However, during the COVID-19 pandemic, GPs experienced unprecedented job burnout as a result of their role as frontline doctors The scope of general doctors covers several domains, including universal vaccination, prevention and management of chronic diseases, mental health care, and planning of health promotion services in the community. The professional training of GPs themselves is poor; they need several training sessions related to community-based knowledge annually, which might explain why some were not willing to take on an additional role. Moreover, most GPs reported no job satisfaction. Additionally, every general doctor must treat more than 500 patients per month. Most of their practice ranges were not general but working in general posts. Rehabilitation is a major aspect of professionalism requiring additional training and clinical practice. However, this study demonstrated that the average age of community general doctors is high, and they seem unable or unwilling to understand community-based rehabilitation or government support policy and, moreover, to take on the role of rehabilitation physicians.
Researchers have encouraged Chinese medical students to become GPs [Citation14]. This is very risky because as most GPs working in an non-local professional major might feel more dissatisfied with their job, face twofold challenges in tedious work, and miss more time in clinical practice.
Case-based payments and the capitation of alternative payment sources decrease the length of stay, which decreases total medical expenditure, especially the risk of catastrophic medical expenditure [Citation15,Citation16]. However, the reformed medical insurance that resulted in rehabilitation therapy in China is reimbursed only for the first 90 days, regardless of the type of disease. After the first 90 d, most therapeutic projects need to be out-of-pocket, particularly physical therapy, occupational therapy, and speech therapy, which require highly professional technology. This means that patients tend to stay in the rehabilitation centers of tertiary hospitals to receive high-quality rehabilitation services. This also indirectly increases the total cost of continued rehabilitation therapy indirectly, such as in community-based hospitals. Most GPs in our study established a lower rate of medical insurance reimbursement as the main factor affecting the development of community-based rehabilitation therapy. Although the first 90 d is indeed an important time for most diseases, it is important to understand that rehabilitation therapy appeals may be necessary and helpful in future healthcare system reforms. Moreover, it may help to reduce patient aggregation and increase the proactivity of GPs.
In a previous study, we found that a few types of modern rehabilitation therapy processes in community-based conditions were key problems in Yunnan Province. The same problems emerged from this study: only half of the outpatients proactively required rehabilitation therapy, which may indicate a lack of rehabilitation awareness among community residents. Considering the results of our study, half of the GPs did not understand the support policies for community-based hospitals. Government advertising is necessary for both residents and community physicians to increase their awareness of disabilities in community rehabilitation. However, we also need to emphasize that rehabilitation medicine requires strong professionalism, deep professional training, and expert mentoring to improve self-confidence.
Nonetheless, we should recognize that, in addition to essential knowledge, GPs also require other skills and attitudes to face aging population challenges [Citation5]. This is an unfair burden for healthcare providers, as our study showed that they were already bearing heavy pressure from outpatients and other professional training. We cannot neglect these challenges: being a GP in this large setting, and the stress of the increased aging population. Although an important method for managing chronic diseases, rehabilitation services need to be better understood by both local residents and GPs. Moreover, we need to respect the willingness of GPs to assume the role of rehabilitation physicians, even if they are the most suitable population for the extent of this service.
Authors contributions
All authors have made substantial contributions to this work and have approved the final version of the manuscript. Concept and design: LHJ, YQH; Acquisition of data: LHJ, YQH, JCD; Statistical analysis: YML, JCD; Data interpretation: YML, LQY; Authorship of the original draft, LHJ, YQH; Review and editing, YML, LQY; Funding, LQY.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The datasets used and/or analyzed for the development of this manuscript are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Ren W, Liu Y, Qiu Y, et al. Development of general practice education and training in China. Chin Med J. 2014;127:1–7.
- Mathers N, Huang YC. The future of general practice in China: from ‘barefoot doctors’ to GPs? Br J Gen Pract. 2014;64(623):270–271. doi: 10.3399/bjgp14X679933.
- Fu Y, Wang J, Sun J, et al. Equity in the allocation of general practitioner resources in mainland China from 2012 to 2019. Healthcare. 2023;11(3):398. doi: 10.3390/healthcare11030398.
- Wu D, Lam TP. Underuse of primary care in China: the scale, causes, and solutions. J Am Board Fam Med. 2016;29(2):240–247. doi: 10.3122/jabfm.2016.02.150159.
- Shi L, Fan L, Xiao H, et al. Constructing a general competency model for Chinese public health physicians: a qualitative and quantitative study. Eur J Public Health. 2019;29(6):1184–1191. doi: 10.1093/eurpub/ckz048.
- Zhang Y, Wang Q, Jiang T, et al. Equity and efficiency of primary health care resource allocation in mainland China. Int J Equity Health. 2018;17(1):140. doi: 10.1186/s12939-018-0851-8.
- Xiaohong Cao YF, Zhou Y, Yang P, et al. Investigation and countermeasures of the current situation of community rehabilitation medicine in shanghai. J Chin Rehabil Med. 2016;31:908–910.
- Wang W, Jiang B, Sun H, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation. 2017;135(8):759–771. doi: 10.1161/CIRCULATIONAHA.116.025250.
- Yuan S, Wei F, Liu W, et al. Methodology discussion of health resource allocation equity evaluation based on agglomeration degree. Chin Hosp Manag. 2015;35:3–5.
- Zhou Y, Zhou L, Fu C, et al. Socio-economic factors related with the subjective well-being of the rural elderly people living independently in China. Int J Equity Health. 2015;14(1):5. doi: 10.1186/s12939-015-0136-4.
- Li X, Krumholz HM, Yip W, et al. Quality of primary health care in China: challenges and recommendations. Lancet. 2020;395(10239):1802–1812. doi: 10.1016/S0140-6736(20)30122-7.
- Yip W, Fu H, Chen AT, et al. 10 Years of health-care reform in China: progress and gaps in universal health coverage. Lancet. 2019;394(10204):1192–1204. doi: 10.1016/S0140-6736(19)32136-1.
- Liu S, Wang L, Zhang T, et al. Factors affecting the work competency and stability of family doctors in shanghai: a tracking study. BMC Fam Pract. 2019;20(1):95. doi: 10.1186/s12875-019-0988-6.
- Xiao Y, Wu X-H, Li C-Y, et al. It is time to encourage Chinese medical students to become general practitioners. Fam Pract. 2022;39(4):778–780. doi: 10.1093/fampra/cmab100.
- He R, Miao Y, Ye T, et al. The effects of global budget on cost control and readmission in rural China: a difference-in-difference analysis. J Med Econ. 2017;20(9):903–910. doi: 10.1080/13696998.2017.1336448.
- Peng J, Zhang M, Yu P, et al. Can single disease payment system based on clinical pathway reduce hospitalization costs in rural area? A case study of uterine leiomyoma in Anhui, China. BMC Health Serv Res. 2018;18(1):990. doi: 10.1186/s12913-018-3807-1.