Abstract
Objective
Chronic pain is a significant source of suffering in the United States, and many individuals increasingly turn towards yoga for pain relief. However, little is known regarding how yoga improves pain. Herein we seek to examine the scope of the literature linking mind-body practices, pain and interoception; an emerging mechanism by which yoga may improve chronic pain.
Methods
This scoping review followed the five-stage methodological framework proposed by Arksey and O’Malley to examine behavioral and neural correlates of interoception in mind-body practices and pain. A broad search of the Pubmed, CINAHL, SportDiscus, Scopus, PsychInfo, and SocIndex databases was conducted, utilizing three clusters of search terms: (1) interoceptive terms, (2) mind-body terms, and (3) pain terms.
Results
A combined total of 690 articles were screened, and 24 findings included for analysis. Sixteen studies examined interoceptive outcomes in response to mind-body practices for chronic pain, and 8 studies examined interoceptive outcomes in response to evoked-pain tasks in experienced mind-body practitioners. Only three studies linked yoga, interoception and pain.
Conclusion
This review relied on the broader mind-body literature to inform our analyses as the literature examining yoga, pain and interoception remains limited. Interoceptive techniques including attending to and acceptance of bodily sensations, appear to be key therapeutic mechanisms in mind-body practices for chronic pain. Future yoga-based interventions would benefit examining interoceptive outcomes and integrating interoceptive strategies to facilitate the pain-modulating benefits of yoga.
Introduction
Background
Chronic pain is a significant source of suffering and disability in the United States, affecting approximately 20% of U.S. adults [Citation1]. As a complex condition with deficits in cognitive appraisal, emotion regulation and physical function, current clinical practice guidelines recommend a multimodal rehabilitation approach to chronic pain [Citation2], where practices requiring patients to be active in the rehabilitation process, such as exercise and mind-body practices, may be particularly beneficial [Citation3]. Yoga is a multimodal approach uniquely positioned to address the physical, cognitive, and emotional components of chronic pain, through the use of physical postures (asana), breathing techniques (pranayama), and meditation (dhyana), three of the most commonly practiced eight limbs of yoga. Indeed, yoga-based practices are increasingly popular for pain management, and previous findings indicate that yoga is beneficial for chronic pain [Citation4–7]. However, the mechanisms by which yoga improves chronic pain remain to be understood.
Interoception is emerging as a mechanism by which yoga may improve pain and psychological health [Citation8] yet little direct evidence exists in support of this hypothesis, or the effects of yoga on interoception in other populations [Citation9]. While definitions vary [Citation10], interoception is generally defined as the sense of internal bodily signals [Citation11,Citation12] but more broadly conceptualized as a multidimensional construct requiring both the perception of internal sensations as well as the cognitive appraisal and emotional evaluation of those bodily signals [Citation11]. Yoga has previously been conceptualized to facilitate the integration of bottom-up interoceptive input with top-down cognitive and emotional regulatory processes (See Citation8 for an excellent theoretical framework linking philosophical foundations to modern findings), well-suited to addressing the multidimensional cognitive, emotional and physical symptoms common in chronic pain.
A limitation to the yoga and pain literature is the implicit focus on yoga as an exercise modality, often compared to other forms of physical activity or exercise [Citation4,Citation6,Citation7], and the emphasis on asana practice as the active ingredient of yoga-based practices. However, in the Yoga Sutras of Patanjali, an ancient text describing the eight limbs of yoga and providing guidelines for living a meaningful and purposeful life [Citation13], only three of the 196 sutras are dedicated to describing asana practice (sutras 2.46–2.48), while the remaining describe primarily contemplative and cognitive techniques. Furthermore, B.K.S. Iyengar highlights the role of asana as a means to gain awareness of our innermost states by directing attention towards bodily sensations, thoughts, and emotions that arise during asana [Citation14], an undeniably interoceptive process. However, even the most detailed yoga protocols rarely specify the cuing that occurs during asana, and rather list the postures used in sequence, along with specific breathing and meditation practices. It is therefore possible that cuing in yoga-based interventions could vary widely, such that a greater emphasis might be placed on proprioceptive cueing (e.g. physical alignment) rather than interoceptive cuing (e.g. noticing sensations). We hypothesize that in addition to regular pranayama and dhyana practices, the benefits of asana practice are not limited to the physiological, but also the interoceptive work that occurs while performing physical postures.
Identifying the research question
As there is limited evidence to support the benefits of yoga on interoception in chronic pain, this scoping review sought to explore the current literature linking mind-body practices to interoceptive processing and pain. The intention was to identify hypothesis-generating patterns within the mind-body literature to inform the selection of interoceptive techniques (e.g. mindful movement, breath awareness, body scans), common in many mind-body practices, to integrate into targeted yoga-based interventions for chronic pain. Consequently, the mind-body practices included in this review were selected due to their origins in or similarity with yoga, including those contemplative traditions conceptualizing a subtle energetic body [Citation11], regardless of their being movement or meditation-based practices.
The choice of interoceptive outcomes included in this review is intentionally broad, to account for the heterogeneity within the literature regarding terminology and assessment [Citation11,Citation12]. In selecting interoceptive outcomes, we follow the four dimensions of interoceptive processing described by Pollatos & Herbert [Citation12], including: interoceptive accuracy (IAc) – the ability to detect bodily signals, such as a heartbeat; interoceptive sensibility (IS) – the subjective report on bodily states, such as muscle tension; interoceptive awareness (IAw) – both the awareness of and confidence in the accuracy of one’s perception of internal states; and emotional evaluation of interoceptive signals (IE) – the interpretation of and attention paid to bodily signals [Citation12].
Additionally, we examine neural correlates of interoceptive processing with the conceptualization that interoception is a multidimensional construct including the sensory perception of internal states along with the cognitive appraisal and emotional evaluation of those bodily signals [Citation11]. As such, we selected neural correlates relevant to this review to be those representing an interoceptive network of regions identified by Critchley et al. [Citation15]. The somatosensory and insular cortices are proposed to play a central role in receiving raw interoceptive signals and generating subjective feeling states [Citation15,Citation16] and ‘second-order’ regions including the anterior cingulate cortex (ACC), ventromedial and dorsolateral prefrontal cortices (vmPFC, dlPFC) [Citation15] assist in the cognitive regulation and emotional evaluation of internal feeling states [Citation12,Citation15]. We select these regions acknowledging the limitation of assuming the accuracy of these regions as key interoceptive substrates, as the field remains relatively nascent. Therefore, we rely on the authors expertise on the neural regions of interest with the purpose of identifying patterns within the literature that link mind-body practices to behavioral and neural correlates of multidimensional interoceptive processing, including the perception, cognitive appraisal, and emotional evaluation of pain.
Methods
This scoping review was conducted following the 5-stage methodological framework for conducting rigorous, transparent scoping reviews as suggested by Arksey and O’Malley [Citation17] and updated by Levac and colleagues [Citation18]. We outlined the first stage ‘identifying the research question’ in our introduction. Herein, we report on the next four stages and summarize and report the findings in the results section of this review. A detailed protocol can be made available upon request to the corresponding author.
Identifying relevant studies
This scoping review used a broad search strategy seeking to link three bodies of literature: interoception, mind-body practices and pain. As such, search terms were constructed in three clusters: (1) interoceptive terms, (2) mind-body terms and (3) pain terms (a detailed search string is included in the Supplementary Material with this manuscript). The cluster of interoception terms was intentionally broad to account for the vast heterogeneity of terminology within the literature. Emotion regulation terms and neural regions were included within this cluster to account for the emotional evaluation dimension of interoception [Citation12] and regions hypothesized to reflect the interoceptive neural network [Citation15]. Mind-body terms initially focused on yoga, mindfulness, and meditation, but tai chi and qigong were later included due to the evolving nature of the scoping review. Arksey and O’Malley suggest that search criteria in scoping reviews be amendable to allow for additional criteria to be added once greater familiarity with the field is reached [Citation17].
The primary search was conducted in June 2022 of the following databases: Pubmed, CINAHL, SportDiscus, Scopus, PsychInfo, and SocIndex. We placed limits and filters for English and Human subjects research, with the remaining exclusion criteria applied during screening and review. We identified duplicates with the de-duplication tool in Mendeley desktop. Two additional searches were conducted in July 2023 to: (1) identify new findings published within the past year, and (2) include the search terms tai chi and qigong as mind-body terms. In addition to the database searches, we scanned the reference lists of included articles.
Study selection
As the reviewer most familiar with the breadth of the topic, the database searches and abstract/title screening were conducted by the primary author. Data extraction was then conducted by two independent reviewers (first and second authors). The final assessment of inclusion/exclusion criteria was determined by consensus between the primary and senior author.
Inclusion and exclusion criteria
We included any peer-reviewed, empirical study written in English that examined interoception outcomes in response to either (1) mind-body practices (MBP) for individuals with chronic pain; or (2) pain-evoked tasks in experienced mind-body practitioners. Studies were excluded if they did not meet the inclusion criteria as defined in . Interoception outcomes were defined as standardized behavioral measures examining changes in self-reported awareness of bodily sensations or changes in at least one of the neural correlates identified by Critchley et al. [Citation15] and listed in . Mind-body practices were defined as any style of yoga, mindfulness, meditation, tai chi, or qigong.
Table 1. Inclusion and exclusion criteria.
Depending on the study population (chronic pain or mind-body practitioners) we defined the following additional criteria. Chronic pain population met by diagnostic criteria (e.g. fibromyalgia, chronic low back pain (cLBP)) or a minimum pain duration of 3 months. Experienced mind-body practitioners are defined by the original authors’ criteria for including individuals with expertise or experience in a mind-body practice deemed sufficient for comparison to a matched novice or naïve control group.
Following the initial abstract/title screening, the primary and senior author revised the inclusion/exclusion criteria (indicated in ) prior to data extraction to include the following additional criteria to narrow the scope of the review for a more meaningful analysis. This revision of criteria was conducted in accordance with Arksey and O’Malley’s suggestion that scoping review criteria be amendable once greater familiarity with the field is reached [Citation17]. Studies included only for neural correlates of interoception were required to include at least one pain outcome as neural correlates of interoception may also activate in response to non-pain related tasks (e.g. working memory). Mind-body practices were further refined to include tai chi and qigong, and excluded any interventions in which a MBP was combined with another intervention (e.g. transcranial direct current stimulation) that could confound the findings. In studies that did not report duration of chronic pain, studies were included if the population’s diagnostic criteria included a minimum duration of at least 3 months of pain (e.g. fibromyalgia, cLBP) but excluded if the pain population included a mix of acute and chronic pain or met diagnostic criteria that did not specify a minimum pain duration of 3 months (e.g. some findings in knee osteoarthritis). We excluded studies examining the relationship between mind-body practices and pain in healthy, practice-naïve individuals assigned to an intervention [Citation19,Citation20] to reflect findings that neural changes in mind-body practitioners may be due to years of regular practice [Citation21,Citation22], and evidence that chronic pain is associated with neuroplastic changes distinct from typical pain processing in healthy individuals [Citation23].
Charting the data
The following data was extracted from each of the articles reviewed, utilizing Microsoft excel to organize the data in two separate sheets for studies examining interoception outcomes in response to either (1) MBP for individuals with chronic pain; or (2) pain-evoked tasks in experienced mind-body practitioners.
The following data was extracted from all studies: author(s), publication year, sample size, mean age, female to male ratio, type of MBP, control group (if applicable), study design, interoceptive outcomes matching inclusion criteria, remaining outcome measures, and key findings as interpreted by the original authors. Additional data extracted from studies examining individuals with chronic pain included: pain population, minimum pain duration and MBP intervention duration. Additional data extracted from studies in experienced practitioners included: length of experience and type of evoked pain stimulus. Key findings were further separated into behavioral and neural correlates. As the focus of this review was on interoception and pain, we charted significant and nonsignificant results for all interoception and pain-related outcomes. All remaining outcomes examined (e.g. depression, physical function) were charted if significant to provide relevant contextual findings.
Collating, summarizing and reporting the data
To collate and summarize the findings reported in the results below, the data was organized into two sections: (1) MBP for individuals with chronic pain; or (2) pain-evoked tasks in experienced mind-body practitioners. Within each section, the data was further summarized by (a) behavioral interoception outcomes and (b) neural correlates of interoception. Behavioral outcomes were further subdivided by assessment type and neural correlates were subdivided into task-evoked findings (e.g. neural activity during pain or meditation) and structural/resting state connectivity findings. Based on the patterns that emerged from the literature, we discuss the neural findings within two broad categories: (1) neural processing in regions involved in the perception and awareness of internal bodily signals, and (2) neural processing in regions associated with the cognitive and emotional evaluation of internal states.
Results
Articles retrieved
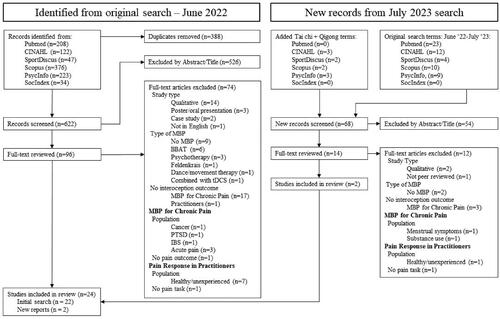
A combined total of 690 articles were screened and 24 articles included for analysis. A PRISMA flow diagram of the search procedure is presented in . The initial search yielded 1010 hits, with 622 titles remaining after duplicates were removed. All titles and abstracts were examined for relevance and after removing 526 irrelevant hits, 96 titles were reviewed in their entirety and screened for inclusion or exclusion. Seventy-four articles were excluded for reasons listed in the PRISMA flow diagram () and the initial search yielded 22 articles included in this scoping review. The reference lists of these articles were scanned but did not yield any new findings. The additional searches in July 2023 yielded a combined total of 68 new hits, of which 54 were irrelevant. Fourteen were reviewed in their entirety, 12 excluded for the reasons listed in , and two additional studies (two tai chi studies from 2016/17) were included for a combined total of 24.
Effects of MBP on interoception in chronic pain
Sixteen studies examined interoceptive outcomes in response to MBP in chronic pain; study characteristics are detailed in . Intervention lengths ranged from 2 to 16 weeks and types of chronic pain included: chronic low back (cLBP) [Citation28–30], heterogeneous pain populations [Citation5,Citation31], opioid-treated chronic pain [Citation32,Citation33], fibromyalgia [Citation34,Citation35], chronic neck pain [Citation24,Citation36], knee osteoarthritis [Citation37], chronic musculoskeletal pain [Citation38], migraine [Citation39], and breast cancer survivors with chronic neuropathic pain [Citation40] or persistent post-surgical pain [Citation41]. Types of MBP included: tai chi [Citation24,Citation34,Citation36,Citation37], yoga [Citation5,Citation30], qigong [Citation41], and the following mindfulness-based interventions: brief self-compassion training [Citation28], mindfulness-based stress reduction (MBSR) [Citation29,Citation35,Citation39,Citation40], mindfulness-oriented recovery enhancement (MORE) [Citation32,Citation33], mindfulness-based cognitive therapy (MBCT) [Citation31], and a mindfulness-based pain management program (MBPM) [Citation38]. Key findings for all studies are detailed in and summarized below.
Table 2. Study characteristics of Mind-Body practices (MBP) for chronic pain.
Table 3. Effects of Mind-Body Practices (MBP) on interoceptive outcomes in chronic pain.
Behavioral outcomes
Eight studies reported behavioral interoception outcomes, of which six used the Multidimensional Assessment of Interoceptive Awareness (MAIA) [Citation24,Citation28,Citation31,Citation33,Citation36,Citation41], one used the Body Responsiveness Questionnaire (BRQ) [Citation5] and one used a subset of questions combined from the BRQ and Body Awareness Questionnaire (BAQ) to examine body awareness [Citation30]. No studies used a heartbeat detection/tracking task to assess interoceptive accuracy.
Multidimensional assessment of interoceptive awareness (MAIA)
Four studies identified improvements in interoceptive sensibility assessed with the MAIA in response to MBP in chronic pain, including MBCT [Citation31], qigong [Citation41], MORE [Citation33], and brief self-compassion training [Citation28]. Two reports (from the same trial) found a mean increases in MAIA scores in response to tai chi [Citation24], and reported that interoceptive sensibility was not a predictor of reduced pain [Citation36].
Differences in which MAIA subscales responded to MBP in chronic pain were also reported. Not-distracting and Self-regulation scales improved in response to MBCT, where Not-distracting partially mediated reductions in depression, and changes in Noticing and Attention Regulation were not significant [Citation31]. Total MAIA and Self-regulation improved in response to MORE, and Self-regulation was a significant mediator of cognitive reappraisal, which facilitated reductions in emotional distress [Citation33]. Qigong improved all MAIA domains except Noticing and Not-distracting [Citation41]. Self-compassion training improved total MAIA along with Self-regulation, Body Listening and Attention Regulation, with a trend towards improving Emotional Awareness, Trusting and Not Worrying [Citation28].
Body awareness and body responsiveness questionnaires (BAQ, BRQ)
The only two yoga interventions included in this analysis used the BAQ and BRQ [Citation5,Citation30]. Body responsiveness improved in response to Hatha yoga [Citation5] whereas body awareness was not a significant independent mediator of improved back function in response to Viniyoga [Citation30].
Neural correlates
Nine studies examined changes in neural correlates of interoception in response to MBP for chronic pain [Citation28,Citation29,Citation32,Citation34,Citation35,Citation37–40]. Behavioral findings and original author interpretations of neural correlates are detailed in . For brevity, only neural correlates and pain outcomes are summarized below.
Task-evoked changes: fMRI and EEG
Six studies examined task-evoked neural activity, of which four used functional magnetic resonance imaging (fMRI) [Citation28,Citation29,Citation39,Citation40] and two used electroencephalography (EEG) [Citation32,Citation38], to examine pain-, emotion-, and attention-evoked activity. The emotion-evoked studies were included as they reported emotion-regulation findings consistent with second-order neural representations of interoceptive processing [Citation15] and the emotional evaluation component of interoception [Citation12].
Pain-evoked neural activity
Two studies examined pain-evoked neural activity in response to self-compassion training [Citation28] and MBPM [Citation38]. In both studies, there were no post-training differences in pain-evoked visual analog scale (VAS) intensity or unpleasantness ratings despite improvements in functional pain outcomes. During pain stimulation, self-compassion training produced reductions in right temporo-parietal junction (rTPJ) activity, correlating with reductions in pain intensity [Citation28], and MBPM produced mild, but non-significant, reductions in amygdala and anterior insula (aINS) activity [Citation38]. During pain anticipation, self-compassion training produced increased right dlPFC and ventral posterior cingulate cortex (vPCC) activity correlating with lower self-compassion and greater Body Listening, respectively [Citation28]; and MBPM produced greater dlPFC and somatosensory (S2) deactivation (i.e. increased activity) correlating with improved mental health and pain controllability [Citation38].
Emotion-evoked neural activity
Two studies examined emotion-evoked neural activity in response to abbreviated MBSR [Citation29] and MBSR [Citation40]. Both studies found improvements in functional pain outcomes but no change in pain intensity [Citation40] or the sensory/affective aspects of pain [Citation29]. On a sadness-induction task, abbreviated MBSR produced increased subgenual anterior cingulate cortex (sgACC) activity, correlating with emotional valence/intensity ratings, and increased vlPFC and dmPFC activity [Citation29]. On an emotional Stroop task with pain-related sensory and affective words, MBSR produced reductions in S1, precuneus and dlPFC activity [Citation40].
Attention-evoked neural activity
Two studies examined attention-evoked neural activity in response to MORE during mindfulness [Citation32] and enhanced MBSR (MBSR+) during a cognitive task [Citation39]. Pain outcomes included reduced opioid usage [Citation32] and reduced headache-related disability with no change in intensity [Citation39]. During meditation, MORE increased frontal alpha and theta power where increased theta power mediated reductions in opioid dosing. MORE also increased frontal-midline-theta (FMT) coherence, reflecting increased prefrontal to limbic structure connectivity [Citation32]. During a cognitive task, MBSR + reduced activity in the cuneus and parietal operculum, a region including the posterior insula [Citation39].
Structural and connectivity differences
Four studies examined differences in brain volume or structural and/or functional connectivity. Three examined resting state functional connectivity [Citation34,Citation37,Citation39], one used structural MRI [Citation39], and one used Arterial Spin Labelling [Citation35].
Structural MRI
One study examined structural brain changes as part of a multimodal neuroimaging study in response to MBSR + in which there were no significant differences between groups, but both MBSR + and controls demonstrated reductions in anterior midcingulate cortex (aMCC) volume [Citation39].
Resting state functional connectivity (rsFC)
Three studies examined changes in rsFC in response to tai chi [Citation34,Citation37] and MBSR+ [Citation39]. In addition to the clinical improvements after MBSR + reported above [Citation39], tai chi improved fibromyalgia [Citation34], and knee pain [Citation37] symptoms. One study noted altered rsFC prior to intervention, where individuals with fibromyalgia had greater dlPFC to rostral anterior cingulate cortex/medial prefrontal cortex (rACC/mPFC) connectivity compared to healthy controls [Citation34]. Tai chi further enhanced this altered connectivity, correlating with fibromyalgia symptom improvements, and reduced rACC/mPFC connectivity to the periaqueductal gray and hippocampus and increased rACC/mPFC connectivity to regions linked to the cognitive, emotional and sensory aspects of pain [Citation34]. In knee osteoarthritis, tai chi produced a non-significant increase in mPFC-amygdala connectivity, correlating with improved physical function [Citation37]. MBSR + demonstrated greater reductions in aINS connectivity to specific regions of the cognitive task network, including the posterior parietal cortex and cuneus [Citation39].
Brain perfusion
One study used Arterial Spin Labelling, an fMRI method to generate regional cerebral blood flow (rCBF) maps of subtle blood perfusion differences in response to MBSR [Citation35]. Prior to intervention, greater rCBF to ACC and aINS were associated with greater pain intensity ratings, and greater rCBF to the amygdala correlated with greater anxiety and pain catastrophizing. After training, MBSR did not demonstrate any unique differences in pain outcomes or neural activity, but rCBF to emotional processing regions was no longer associated with pain intensity after MBSR or active the active control intervention (psychoeducation) [Citation35].
Interoceptive processing of pain in experienced mind-body practitioners
Eight studies examined interoceptive differences in response to evoked-pain in experienced mind-body practitioners; study characteristics are detailed in . Types of practitioners included: practitioners of the Nyingma and Kagyu traditions of Tibetan Buddhism, similar to mindfulness [Citation42,Citation43], Zen meditation [Citation44,Citation45], Vipassana meditation, a form of mindfulness [Citation46], Transcendental meditation [Citation47], any type of formal meditation practice [Citation48], and any type of yoga practice integrating postures, meditation and breathing [Citation49]. Key findings are detailed in and summarized below.
Table 4. Study characteristics of interoception outcomes in experienced mind-body practitioners.
Table 5. Pain-related interoception outcomes in experienced mind-body practitioners.
Behavioral outcomes
Only one study in practitioners use a behavioral interoception measure in which Buddhist practitioners reported lower unpleasantness ratings than controls, despite similar intensity ratings on a pain-evoked task [Citation43]. While interoceptive sensibility (MAIA) was not the focus of this analysis, it was higher in practitioners and negatively correlated with pain catastrophizing across both groups. The primary findings of this study reported that cognitive defusion (the psychological distancing from thoughts and feelings), was the most specific predictor of pain unpleasantness, surviving an adjustment for pain catastrophizing, also strongly associated with unpleasantness ratings [Citation43].
Neural correlates
Seven studies examined neural correlates in response to pain-evoked tasks in practitioners to matched novice (no experience) or practice-naïve (minimal training) controls. Behavioral findings along with the original author interpretations of neural correlates are detailed in . For brevity, only neural correlates and pain outcomes are summarized below.
Pain-evoked activity: fMRI and EEG
Five studies examined pain-evoked neural activity: four used fMRI [Citation42,Citation45–47], and one used EEG [Citation48].
Pain-evoked activity in a mindful/meditative state
Two studies examined pain-evoked neural activity while in a mindful or meditative state in mindfulness practitioners of the Vipassana [Citation46] and Buddhist [Citation42] traditions. In both studies, practitioners demonstrated lower unpleasantness but similar intensity ratings to controls. During pain, Vipassana practitioners demonstrated greater pINS/S2 activation associated with lower unpleasantness ratings [Citation46] whereas Buddhists demonstrated greater aINS and aMCC activity but no differences in pINS/S2 activation [Citation42]. During pain anticipation, Vipassana practitioners demonstrated lower lPFC and greater rACC/vmPFC activity [Citation46] and Buddhists demonstrated lower aINS, aMCC and amygdala activity [Citation42].
Pain-evoked activity outside a mindful/meditative state
Two studies instructed practitioners to not meditate/engage in mindfulness during pain in Zen [Citation45] and transcendental meditation (TM) [Citation47] practitioners. Zen practitioners demonstrated lower pain sensitivity (i.e. required higher stimulus intensity) to match similar subjective pain intensities as controls [Citation45] and TM practitioners demonstrated no difference in pain intensity ratings [Citation47]. Zen practitioners demonstrated greater activation in sensory pain regions including the insula, thalamus and dACC, despite controlling for greater stimulus intensity in practitioners, whereas controls demonstrated greater activation in prefrontal and emotion-processing regions in the bilateral dlPFC, amygdala, left middle frontal gyrus, right hippocampus and mPFC/orbitofrontal cortex [Citation45]. Furthermore, greater meditation experience was associated with greater de-activation in prefrontal regions, and meditators with the lowest pain sensitivity had the weakest functional connectivity between the dACC and dlPFC [Citation45]. TM practitioners demonstrated lower pain-related response in the thalamus and whole brain but no other regions of interest examined, including the ACC and PFC [Citation47]. After novices learned and practiced TM for 5 months, there were no longer any significant differences between groups.
One study instructed participants to focus only on the unpleasantness of pain in meditation practitioners of any discipline [Citation48]. Differences in pain unpleasantness ratings only differed when the sample was reduced to practitioners with a minimum of 6 years of experience, after which lower unpleasantness correlated with greater experience. During pain, practitioners demonstrated lower INS/S2 activity, but this effect did not survive correction for anticipatory activity prior to stimulation. During pain anticipation, practitioners demonstrated lower MCC activity, an effect predicted by greater meditation experience and associated with decreased unpleasantness. Controls demonstrated greater mPFC/pACC activity during pain anticipation, correlating with greater unpleasantness ratings, an effect that was reversed in practitioners and mediated by lower anticipatory MCC activity [Citation48].
Structural differences
Two studies used MRI to compare structural differences to performance on pain tasks in Zen [Citation44] and yoga [Citation49] practitioners. Zen practitioners demonstrated greater dACC and S2 cortical thickness, and years of experience correlated with greater ACC thickness. Across participants, lower pain sensitivity was associated with greater cortical thickness in the right dACC, S2 and insular cortices with no differences between groups, despite practitioners demonstrating lower pain sensitivity overall [Citation44]. Yoga practitioners demonstrated greater pain tolerance and greater gray matter volume in multiple cortical regions, including the S2/insular cortices, cingulate/SMA/S1 and left dorsal mPFC [Citation49]. However, only insula volume correlated with increased pain tolerance in practitioners and left insular volume correlated with years of experience [Citation49].
Discussion
The purpose of this scoping review was to examine the scope of the literature on mind-body practices and pain with a focus on interoceptive outcomes, to inform yoga-based interventions for chronic pain. Patterns of findings are discussed below, with the intention of forming hypotheses for future research on yoga, interoception and pain. Prior to a further discussion of the findings, we note that of the 24 studies included in this analysis, only two were large randomized controlled trials including a behavioral or neural correlate of interoception [Citation24,Citation39]. Interoception was not the primary outcome in either of these trials, and therefore they may not have been sufficiently powered to reliability detect change. Of these two trials, changes in interoception were reported on an exploratory basis in one [Citation24], and analyses of secondary outcomes were not adjusted for multiple comparisons in the other [Citation39], wherein multiple comparisons of secondary outcomes can increase the probability of a false significant result. Furthermore, the remaining intervention trials were secondary analyses, subsets of larger trials or pilot studies designed to evaluate preliminary feasibility, but for which efficacy analyses would require a full randomized controlled trial. Lastly, all the studies on experienced mind-body practitioners were cross-sectional and therefore must also be interpreted with caution. Cross-sectional designs cannot evaluate causation, and are limited to potential bias or selection effects (e.g. individuals with greater pain tolerance or interoceptive awareness may be more likely to choose a MBP) that may influence results. As such, we suggest that these findings must all be interpreted with caution but viewed as informative for future research on yoga, interoception and pain.
Yoga, interoception and pain
As hypothesized, the current literature linking the three areas of interest for this review – yoga, interoception and pain – is sparse, with only two yoga-based interventions [Citation5,Citation30] and one study of yoga practitioners [Citation49] identified. These findings must also be interpreted with caution as they are either cross-sectional [Citation49], preliminary pilot findings results [Citation5], and/or use body awareness measures [Citation5,Citation30], previously noted to be inadequate for evaluating interoceptive sensibility [Citation51], but included as they provide useful insight into the relationship between yoga, body awareness, and chronic pain.
Findings from the two yoga interventions conflict, where body responsivity improved in one account [Citation5] but was not a significant mediator of improved back function in the other [Citation30]. These could reflect differences in pain population, where Schmid et al. [Citation5] reported a complex, heterogeneous pain population with high opioid use and activity limitations, whereas Sherman et al. [Citation30] only included individuals with cLBP receiving no concurrent pain care and without complex causes of pain. Or, they could reflect the use of the full standardized questionnaire in one finding [Citation5] whereas Sherman et al. [Citation30] acknowledged the limitations of these measures [Citation51] and used a subset of questions from the BRQ and BAQ combined, selecting items most likely to respond to yoga [Citation30]. However, improved interoceptive sensibility in response to yoga in other populations, including healthy sedentary individuals [Citation52], adults with neurodisability [Citation53], and PTSD [Citation54], suggests that it would be an important outcome to examine in future trials of yoga for chronic pain.
The only study to report interoceptive differences in yoga practitioners [Citation49] presents intriguing results as the insular cortex, a primary region in interoceptive processing [Citation15,Citation16] was the only cortical region to mediate improved pain tolerance in practitioners. Additionally, despite no instructions on specific strategy use, practitioners reported using interoceptive strategies during pain, including focused breathing, non-reactive observing of sensations, and acceptance of pain in contrast to distraction and avoidance techniques by controls. Authors suggest that regular yoga practice may promote a more adaptive interoceptive response to pain, contributing to structural differences in the insula [Citation49].
MBP and self-reported interoceptive sensibility
Patterns of the effects of MBP on interoceptive sensibility in chronic pain began to emerge in the six interventional studies that used the MAIA [Citation24,Citation28,Citation31,Citation33,Citation36,Citation41]. All three of the mindfulness-based interventions improved interoceptive sensibility, of which two demonstrated improvements in comparison to active treatment controls [Citation31,Citation33], and one after longitudinal intervention [Citation28]. In contrast, of the three studies using movement-based MBPs, only qigong improved interoceptive sensibility [Citation41] whereas two reports (from the same trial) did not report significant differences after tai chi [Citation24,Citation36], of which one analyzed the MAIA only on an exploratory basis [Citation24]. However, tai chi did yield a mean increase on all of the MAIA subscales [Citation24] and postural awareness was a significant predictor of reduced pain after tai chi [Citation36]. Within postural awareness, it was specifically the effortless awareness and connectedness score that predicted improved pain, suggested to reflect a more effortless awareness between one’s posture, wellbeing and habitual movement patterns to facilitate pain relief [Citation36]. The discrepancy in these findings could reflect differences in MBP delivery. As described by the authors, the mindfulness-based and qigong interventions all included an emphasis on cognitive appraisal skills [Citation28,Citation31,Citation33,Citation41] in addition to breath and body awareness, whereas the tai chi interventions described a greater emphasis on breath, body and movement awareness but not cognitive skills [Citation24,Citation36]. In accordance with the conceptualization of interoception as a multidimensional construct, we suggest that interoceptive strategies that facilitate not only awareness of, but also appraisal and evaluation of internal signals are essential components of MBP for chronic pain.
Subscale analyses reveal further insight into the benefits of distinct interoceptive techniques. While all of the MAIA subscales were not included in all reports, only Self-regulation [Citation28,Citation31,Citation33,Citation41] and Body Listening [Citation28,Citation33,Citation41] consistently showed improvements in the studies in which they were included. Interoceptive Self-regulation specifically measures the ability to regulate distress by attending to bodily sensations [Citation55] suggesting that training in the ability to use breathing techniques and body awareness to self-regulate distress may be a particularly important therapeutic mechanism of MBP for chronic pain [Citation33]. Improved Body Listening after self-compassion training was also the only scale to correlate with changes in neurological processing during pain anticipation, particularly in the vPCC [Citation28]. Authors interpret this finding to suggest the self-compassion produced a greater awareness of and ability to focus on bodily sensations while anticipating pain, lending support to the above findings that breath and body awareness may be key self-regulatory mechanisms for chronic pain. Finally, one study noted that improvements in Not-distracting mediated reductions in depression symptoms, and was the only subscale to not correlate with any other MAIA scales [Citation31]. These findings could reflect the study’s population (chronic pain with comorbid depression) or, authors suggest that Not-distracting, defined as the tendency to not ignore or distract oneself from sensations of pain or discomfort [Citation55], may represent a coping style distinct from other components of interoceptive sensibility in chronic pain [Citation31]. As we discuss in more detail in regard to neural correlates below, attending to rather than ignoring or distracting oneself from unpleasant sensations appears to be a key technique for regulating the pain experience, as previously noted in mechanistic findings [Citation56,Citation57].
Neural correlates of interoceptive processing
Herein we briefly summarize the findings on neural correlates of interoceptive processing, relying on the author’s expertise for their interpretation of neural activity. We broadly categorize these findings in two sections: (1) neural processing in regions primarily involved in the perception and awareness of internal bodily signals, including the somatosensory and insular cortices [Citation15,Citation16], and (2) neural processing in regions associated with the cognitive and emotional evaluation of internal signals [Citation12,Citation15], including the anterior cingulate (ACC), ventromedial and dorsolateral prefrontal cortices (vmPFC and dlPFC).
Detecting internal states
Experienced practitioners showed some, albeit inconsistent, differences in primary interoceptive processing regions. During pain, increased pINS/S2 activity was associated with reduced pain unpleasantness while in a mindful state [Citation46], but another report found no change in pINS/S2 activity while in engaged in Open Presence (OP) meditation [Citation42]. Rather, OP produced greater aINS/aMCC activity increased during pain and decreased aINS/aMCC activity during pain anticipation [Citation42]. Authors indicate that the aINS/aMCC are key regions of the salience network [Citation42], important for assigning emotional weight to homeostatically-relevant stimuli [Citation50]. As the aINS is proposed to be essential for the subjective awareness of internal sensations [Citation15] whereas the pINS is more involved in perceiving pain intensity [Citation23], these subtle differences could reflect different meditation styles. In mindfulness, attention is directed towards the present moment, including towards the pain experience, along with an attitude of nonjudgmental acceptance [Citation46]. In contrast, OP meditation places greater emphasis on cultivating a state of effortless openness and acceptance [Citation42]. While overlapping, the attention to and acceptance of bodily sensations are distinct interoceptive strategies, both of which may be essential in modulating the pain experience and important to examine into yoga-based interventions for chronic pain.
A few findings noted structural differences in the insula and somatosensory cortices among experienced practitioners, linked to experience and reduced pain sensitivity [Citation44,Citation49], but there were no unique structural differences in response to MBP for chronic pain. Rather, neural correlates in response to MBP in chronic pain occurred primarily in prefrontal and emotion processing regions. These could reflect differences in pain processing in individuals with chronic pain in contrast to healthy individuals [Citation23] or the vast differences in experience, where experienced practitioners had multiple years of regular practice in contrast to 2–3-month intervention periods (). It has been previously suggested that it may take longer to develop more automatic, bottom-up processing of sensory and interoceptive input, but that the integration of bottom-up interoceptive processing with top-down cognitive and emotion-regulation processing may be an essential benefit of yoga-based practices [Citation8]. A few findings begin to lend support to this hypothesis. MBSR + reduced aINS connectivity to regions of the cognitive task network, suggested to reflect improved cognitive efficiency, and less depletion of cognitive and emotional resources during pain [Citation39]. Similarly, MORE increased frontal-midline-theta coherence, interpreted to reflect increased PFC to ACC connectivity, or greater plasticity between top-down and bottom-up self-regulation structures [Citation32].
Cognitive and emotional evaluation of pain
As noted above, neural correlates in response to MBP in chronic pain occurred primarily in prefrontal and emotion processing regions, with similarities to correlates in long-term practitioners. MBPM reduced dlPFC and S2 deactivation during pain anticipation, correlating with pain controllability, suggested to reflect a greater ability to maintain cognitive control and focus on bodily sensations [Citation38]. MBSR increased sgACC and prefrontal activity during a sadness-induction task, interpreted as greater access to and attentional awareness of one’s emotional state [Citation29]. MORE produced greater frontal alpha and theta power, interpreted to reflect greater prefrontal activation and improved self-regulation, corresponding with improved self-referential processing [Citation32]. Furthermore, tai chi further enhanced altered connectivity between the dlPFC and rACC/mPFC, associated with clinical improvements, suggested to reflect greater self-regulatory processes to cope with repeated pain [Citation34]. Additionally, tai chi reduced rACC/mPFC connectivity to the periaqueductal gray and hippocampus, important regions in the conceptualization of chronic pain as a form of long term learning [Citation23].
Similar interpretations appear in the findings of experienced practitioners. During pain anticipation, practitioners demonstrated greater mPFC/pACC [Citation48] and rACC/vmPFC [Citation46] activity, predicting reduced unpleasantness in one finding [Citation48], and interpreted to reflect greater attention regulation prior to pain. Similarly, reduced dACC to dlPFC connectivity predicted reduced pain sensitivity, suggested to reflect a functional decoupling to allow painful stimuli to be interpreted with more acceptance/cognitive disengagement than threat [Citation45]. As a whole, the use of cognitive and emotion regulatory interoceptive strategies such as maintaining attention to and acceptance of unpleasant sensations, appear common in mind-body practitioners and may present an important initial therapeutic target for MBP in chronic pain.
MBP and the pain experience
One of the most interesting patterns that emerged is that MBPs largely have a greater impact on functional pain outcomes, reflecting the ability to effectively manage pain symptoms, despite limited or no improvements in pain intensity. In MBP studies that included both pain intensity and functional pain outcomes, individuals with chronic pain demonstrated no difference in evoked pain intensity and unpleasantness ratings despite improvements on functional pain outcomes [Citation28,Citation38], reductions in pain interference despite no change in intensity ratings [Citation5,Citation40], and reduced migraine frequency and functional impact despite no change in intensity [Citation39]. Additionally, seven of the eight studies examining evoked pain in experienced practitioners reported lower unpleasantness despite similar intensity ratings [Citation42,Citation43,Citation46,Citation48], or higher pain thresholds in practitioners matched to similar subjective intensities [Citation44,Citation45,Citation49]. While the exact neural regions involved continue to be explored, authors do largely concur that regular mind-body practitioners are able to decouple the sensory and cognitive/affective pain experience [Citation45,Citation46], such that greater pain intensity does not always imply a greater negative emotional experience of pain. We suggest that this pattern matches the conceptualization of interoception as a multidimensional construct including sensory perception of internal states along with the cognitive appraisal and emotional evaluation of those bodily signals [Citation11]. MBPs appear to improve the relationship between oneself and unpleasant bodily sensations, such that they are experienced with acceptance rather than avoidance. The ability to maintain focused attention on the breath, sensations and non-judgmental acceptance of the sensory experience emerged as common techniques amongst MBP contributing to an improved pain experience.
Limitations
This review presents several limitations. First and foremost is the nature of the scoping review, such that the purpose is to examine the scope of the current literature on a nascent body of research, rather than to critically evaluate the findings or draw conclusions [Citation17]. While our primary purpose was to examine the link between yoga, interoception and pain, the yoga-based literature is sparse, and we relied on findings from the wider mind-body literature to inform our review. Within the mind-body literature included, the findings disproportionately examined mindfulness and meditation-based practices. While the MBSR curriculum is rooted in yogic and Buddhist practices [Citation58] and includes yoga postures, many of the other practices included in this review are primarily seated cognitive-based practices (e.g. MBCT, MORE, Zen, TM), and may not confer similar effects as movement-based practices such as yoga, tai chi and qigong. Additionally, most of the findings included in this review must be interpreted with caution due to either small sample sizes or study design, including primarily longitudinal, cross-sectional, and pilot studies, as well as secondary analyses/subsamples of larger RCTs ( and ). Only two large RCTs were identified for this review [Citation24,Citation39], where self-reported interoceptive sensibility was a secondary outcome in only one [Citation24]. Furthermore, we did not a priori specify length of experience in mind-body practitioners required to be included in this review. As such, we included studies with practitioners who’s experience ranged from as little as 39 weeks [Citation48] or 1000 h [Citation45] to some with over 30 years of experience [Citation47].
Another limitation is the interoceptive outcomes chosen for this review. Only seven studies utilized the MAIA [Citation24,Citation28,Citation31,Citation33,Citation36,Citation41,Citation43], currently the most commonly used measure of self-reported interoceptive sensibility [Citation10] and two utilized either the BAQ or BRQ, with previously noted limitations [Citation51]. Additionally, we identified no findings using interoceptive accuracy or a heartbeat detection task as an interoceptive outcome matching our remaining criteria. The effects of MBP on interoceptive accuracy in chronic pain remain to be further examined, with conflicting findings regarding whether interoceptive accuracy is [Citation59] or is not [Citation60,Citation61] altered in individuals with chronic pain. We a priori selected the above measures as interoceptive outcomes for this review, but acknowledge that other measures were identified, including a sensation manikin to assess the ratio of pleasant to unpleasant sensations [Citation62] and a dynamic interoceptive signature scale [Citation63]. Additionally, we selected only those mind-body practices with similar contemplative traditions and overlapping practices to yoga. However, other mind-body practices such as Feldenkrais and Basic Body Awareness Therapy and psychotherapeutic techniques like Cognitive Behavioral Therapy,with potentially distinct or overlapping mechanisms, did appear in our search and would be worth examining in future studies.
Perhaps the most significant limitation is the assumption of an interoceptive neural network. While these regions have previously been linked to interoceptive processing [Citation15] and aligns with interoception as a multidimensional construct linking sensory, affective and cognitive processing of internal sensations [Citation11], this body of literature is still new and much remains to be determined. Additionally, pain appears to be processed differently in individuals with chronic pain [Citation23], such that pain-evoked neural activity in experienced mind-body practitioners may not accurately inform neural processing in response to an MBP intervention in chronic pain. This limitation may further be influenced by the demographic differences between studies in mind-body practitioners in comparison to MBP for chronic pain. Most notably, interventions in chronic pain included predominantly middle-aged to older adult (40–60 years old) female participants, whereas studies in experienced practitioners are predominantly in young to middle aged (30–40 years old) male participants. While women are disproportionately more likely to experience chronic pain and be less physically active [Citation64], they are also more likely to practice yoga [Citation65], suggesting that yoga is a particularly useful modality for chronic pain management. However, in examining the current literature, we acknowledge that pain processing in primarily male practitioners may not accurately inform the female experience of chronic pain in response to MBP.
Future directions
In its current state, the mind-body literature on interoception and pain exists primarily in seated mindfulness and meditation-based practices. Of the 16 trials examining MBP for chronic pain, only two utilized yoga [Citation5,Citation30], one qigong [Citation41] and two tai chi [Citation24,Citation36] and only one study examined neural correlates of interoception in response to pain in yoga practitioners [Citation49]. Both seated and movement-based MBPs appear to target interoceptive processes and have overlapping techniques, particularly regarding breath awareness, breath regulation and noticing internal sensations, but we hypothesize that movement-based practices such as yoga have the potential to train individuals to adaptively apply interoceptive strategies to a more diverse range of sensory experiences that may be highly relevant to individuals with chronic pain navigating the challenges of their daily routine. The findings by Villemure et al. [Citation49] lend support to this hypothesis, in which experienced yoga practitioners were not instructed on any particular strategy to use during a cold pain tolerance task, yet they still reported the application of interoceptive strategies during pain without being instructed to do so [Citation49]. By challenging practitioners to notice sensations, regulate breathing and adaptively respond to their internal experience from one posture to the next, each yoga posture may provide a new and unique interoceptive experience.
We believe the current state of the literature is too limited to draw conclusions regarding the conferred benefits of seated or movement-based practices on interoception in chronic pain. In our summary of MBP on self-reported interoceptive sensibility above, mindfulness-based practices [Citation28,Citation31,Citation33] appeared to have a greater impact on interoceptive sensibility than movement-based MBPs [Citation24,Citation36,Citation41]. However, we note that Lauche et al. [Citation24] was also the only RCT in this group, and only reported a mean increase in MAIA after tai chi on an exploratory basis, and as such did not conduct significance tests. The remaining trials were either secondary analyses, pilot, or longitudinal trials. We do hypothesize that mindfulness-based cognitive reappraisal skills may be an important component of any MBP for chronic pain, and that future yoga-based interventions for chronic pain would benefit from the explicit inclusion of such techniques such as acceptance and non-judgmental awareness of sensations, that may confer benefits beyond simply noticing sensations or proprioceptive awareness of physical alignment. Indeed, these techniques fall within the yamas and niyamas, the first and second limbs of Patanjali’s eight limb path of yoga, and include observances such as aparigraha (non-attachment) and ahimsa (non-violence or kindness) that may be an important component of interoceptive self-regulation.
Future studies examining yoga-based interventions for chronic pain would benefit from exploring manipulations to the intervention that would further explore the role of interoception. For example: instructor cuing can be manipulated to only include proprioceptive alignment cueing (i.e. align the knee over the heel) vs. also adding interoceptive cuing (i.e. noticing changes in the breath while in a posture or where sensation arises); participants can be instructed to link movements to their breath vs. noticing and practicing acceptance of sensations during sustained physical postures; or the intervention environment can be manipulated such that practicing without mirrors may challenge individuals to direct attention towards internal sensations rather than noticing how they appear in the mirror. It would also be beneficial to compare interoceptive outcomes in response to interventions that compare yoga to a seated MBP and/or other movement-based practices (e.g. stretching). Additionally, the MBP literature would benefit from evaluating both interoceptive sensibility and interoceptive accuracy measures, such as heartbeat tracking tasks, as changes in interoceptive sensitivity to internal sensations may be distinct from the subjective interpretation of those sensations [Citation66].
Conclusion
The literature linking yoga, interoception and pain remains limited and warrants further research. Findings from the broader mind-body literature indicate interoceptive techniques including attending to and acceptance of bodily sensations, including pain, may be key therapeutic mechanisms for chronic pain. Within this review, we identified no studies that linked interoceptive accuracy, pain and MBP, a topic that remains to be explored. Future yoga-based interventions would benefit examining both self-reported and interoceptive accuracy outcomes and from exploring the role of interoceptive techniques practiced during asana, in addition to structured pranayama and dhyana practices, to evaluate the role of interoception as a pain-modulating benefit of yoga.
Authors contributions
Stephanie Voss: Conception/Design; Data collection; Data analysis and interpretation; Drafting; Critical revision; Final approval of the published version.
Daniel A. Boachie: Data collection; Table/Figure drafting; Final approval of published version.
Norberto Nieves Jr.: Data collection; Table/Figure drafting; Final approval of published version.
Neha P. Gothe: Conception/Design; Data analysis and interpretation; Drafting; Critical revision; Final approval of published version.
Supplemental Material
Download MS Word (13.4 KB)Acknowledgements
The authors would like to acknowledge the contribution of Dr. JJ Pionke for his assistance and guidance in generating our search strategy.
Disclosure statement
Stephanie Voss, Daniel A. Boachie and Norberto Nieves Jr. and Neha P. Gothe have no conflicts of interest to report.
Data availability statement
The detailed study protocol is available upon request.
Additional information
Funding
References
- Yong RJ, Mullins PM, Bhattacharyya N. Prevalence of chronic pain among adults in the United States. PAIN. 2022;163(2):1–22. doi: 10.1097/j.pain.0000000000002291.
- Dowell D, Ragan K, Jones C, et al. CDC clinical practice guideline for prescribing opioids for Pain-United States, 2022. MMWR Recomm Rep. 2022;71(3):1–95. doi: 10.15585/mmwr.rr7103a1.
- Skelly AC, Chou R, Dettori JR, et al. Noninvasive nonpharmacological treatment for chronic pain: a systematic review update. Vol. 227. Rockville: Agency for Healthcare Research and Quality; 2020. p. 20–90. doi: 10.23970/AHRQEPCCER227
- Saper RB, Lemaster C, Delitto A, et al. Yoga, physical therapy, or education for chronic low back pain: a randomized noninferiority trial. Ann Intern Med. 2017;167(2):85–94. doi: 10.7326/M16-2579.
- Schmid AA, Fruhauf CA, Sharp JL, et al. Yoga for people with chronic pain in a community-based setting: a feasibility and pilot RCT. J Evid Based Integr Med. 2019;24:1–11. doi: 10.1177/2515690X19863763.
- Sherman KJ, Cherkin DC, Erro J, et al. Comparing yoga, exercise and a self-care book for chronic low back pain: a randomized, controlled trial. Ann Intern Med. 2005;143(12):849–856. doi: 10.7326/0003-4819-143-12-200512200-00003.
- Sherman KJ, Cherkin DC, Wellman RD, et al. A randomized trial comparing yoga, stretching, and a self-care book for chronic low back pain. Arch Intern Med. 2011;171(22):2019–2026. doi: 10.1001/archinternmed.2011.524.
- Gard T, Noggle JJ, Park CL, et al. Potential self-regulatory mechanisms of yoga for psychological health. Front Hum Neurosci. 2014;8:770. doi: 10.3389/fnhum.2014.00770.
- Pascoe MC, de Manincor MJ, Hallgren M, et al. Psychobiological mechanisms underlying the mental health benefits of yoga-based interventions: a narrative review. Mindfulness. 2021;12(12):2877–2889. doi: 10.1007/s12671-021-01736-z.
- Mehling WE, Acree M, Stewart A, et al. The multidimensional assessment of interoceptive awareness, version 2 (MAIA-2). PLOS One. 2018;13(12):e0208034. doi: 10.1371/journal.pone.0208034.
- Farb N, Daubenmier J, Price CJ, et al. Interoception, contemplative practice, and health. Front Psychol. 2015;6:763. doi: 10.3389/fpsyg.2015.00763.
- Pollatos O, Herbert BM. 2018). Interoception: definitions, dimensions and neural substrates. In G. Hauke & A. Kritikos (Eds.), Embodiment in psychotherapy: a practitioner’s guide. Cham: Springer International Publishing.
- Bryant EF. The yoga sutras of Patanjali: a new edition, translation, and commentary. New York: North Point Press; 2015.
- Iyengar BKS. Light on life: the yoga journey to wholeness, inner peace and ultimate freedom. Pennsylvania: Rodale Books; 2006.
- Critchley HD, Wiens S, Rotshtein P, et al. Neural systems supporting interoceptive awareness. Nat Neurosci. 2004;7(2):189–195. doi: 10.1038/nn1176.
- Craig ADB. Significance of the insula for the evolution of human awareness of feelings from the body. Ann N Y Acad Sci. 2011;1225(1):72–82. doi: 10.1111/j.1749-6632.2011.05990.x.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. doi: 10.1186/1748-5908-5-69.
- Zeidan F, Emerson NM, Farris SR, et al. Mindfulness meditation-based pain relief employs different neural mechanisms than placebo and sham mindfulness meditation-induced analgesia. J Neurosci. 2015;35(46):15307–15325. doi: 10.1523/JNEUROSCI.2542-15.2015.
- Zeidan F, Martucci KT, Kraft RA, et al. Brain mechanisms supporting the modulation of pain by mindfulness meditation. J Neurosci. 2011;31(14):5540–5548. doi: 10.1523/JNEUROSCI.5791-10.2011.
- Lazar SW, Kerr CE, Wasserman RH, et al. Meditation experience is associated with increased cortical thickness. NeuroReport. 2005;16(17):1893–1897. doi: 10.1097/01.wnr.0000186598.66243.19.
- Villemure C, Čeko M, Cotton VA, et al. Neuroprotective effects of yoga practice: age-, experience-, and frequency-dependent plasticity. Front Hum Neurosci. 2015;9:281. doi: 10.3389/fnhum.2015.00281.
- Apkarian AV, Hashmi JA, Baliki MN. Pain and the brain: specificity and plasticity of the brain in clinical chronic pain. Pain. 2011;152(Suppl 3):S49–S64. doi: 10.1016/j.pain.2010.11.010.
- Lauche R, Stumpe C, Fehr J, et al. The effects of tai chi and neck exercises in the treatment of chronic nonspecific neck pain: a randomized controlled trial. J Pain. 2016;17(9):1013–1027. doi: 10.1016/j.jpain.2016.06.004.
- Garland EL, Hanley AW, Riquino MR, et al. Mindfulness-Oriented recovery enhancement reduces opioid misuse via analgesic and positive psychological mechanisms: a randomized controlled trial. J Consult Clin Psychol. 2019;87(10):927–940. doi: 10.1037/ccp0000390.
- Shergill Y, Rice DB, Khoo EL, et al. Mindfulness-Based stress reduction in breast cancer survivors with chronic neuropathic pain: a randomized controlled trial. Pain Res Manag. 2022;2022:4020550–4020514. doi: 10.1155/2022/4020550.
- Feliu-Soler A, Borràs X, Peñarrubia-María MT, et al. Cost-utility and biological underpinnings of Mindfulness-Based stress reduction (MBSR) versus a psychoeducational programme (FibroQoL) for fibromyalgia: a 12-month randomised controlled trial (EUDAIMON study). BMC Complement Altern Med. 2016;16(1):81. doi: 10.1186/s12906-016-1068-2.
- Berry MP, Lutz J, Schuman-Olivier Z, et al. Brief self-compassion training alters neural responses to evoked pain for chronic low back pain: a pilot study. Pain Med. 2020;21(10):2172–2185. doi: 10.1093/pm/pnaa178.
- Braden BB, Pipe TB, Smith R, et al. Brain and behavior changes associated with an abbreviated 4-week mindfulness-based stress reduction course in back pain patients. Brain Behav. 2016;6(3):e00443. doi: 10.1002/brb3.443.
- Sherman KJ, Wellman RD, Cook AJ, et al. Mediators of yoga and stretching for chronic low back pain. Evid Based Complement Alternat Med. 2013;2013:130818–130811. doi: 10.1155/2013/130818.
- de Jong M, Lazar SW, Hug K, et al. Effects of mindfulness-based cognitive therapy on body awareness in patients with chronic pain and comorbid depression. Front Psychol. 2016;7:967. doi: 10.3389/fpsyg.2016.00967.
- Hudak J, Hanley AW, Marchand WR, et al. Endogenous theta stimulation during meditation predicts reduced opioid dosing following treatment with mindfulness oriented recovery enhancement. Neuropsychopharmacology. 2021;46(4):836–843. doi: 10.1038/s41386-020-00831-4.
- Roberts RL, Ledermann K, Garland EL. Mindfulness-oriented recovery enhancement improves negative emotion regulation among opioid-treated chronic pain patients by increasing interoceptive awareness. J Psychosom Res. 2021;152:110677. doi: 10.1016/j.jpsychores.2021.110677.
- Kong J, Wolcott E, Wang Z, et al. Altered resting state functional connectivity of the cognitive control network in fibromyalgia and the modulation effect of mind-body intervention. Brain Imaging Behav. 2019;13(2):482–492. doi: 10.1007/s11682-018-9875-3.
- Medina S, O’Daly OG, Howard MA, et al. Differential brain perfusion changes following two mind–body interventions for fibromyalgia patients: an arterial spin labelling fmri study. Mindfulness (N Y). 2022;13(2):449–461. doi: 10.1007/s12671-021-01806-2.
- Lauche R, Wayne PM, Fehr J, et al. Does postural awareness contribute to Exercise-Induced improvements in neck pain intensity? A secondary analysis of a randomized controlled trial evaluating tai chi and neck exercises. Spine. 2017;42(16):1195–1200. doi: 10.1097/BRS.0000000000002078.
- Shen C-L, Watkins BA, Kahathuduwa C, et al. Tai chi improves brain functional connectivity and plasma lysophosphatidylcholines in postmenopausal women with knee osteoarthritis: an exploratory pilot study. Front Med. 2021;8:775344. doi: 10.3389/fmed.2021.775344.
- Brown CA, Jones AKP. Psychobiological correlates of improved mental health in patients with musculoskeletal pain after a mindfulness-based pain management program. Clin J Pain. 2013;29(3):233–244. doi: 10.1097/AJP.0b013e31824c5d9f.
- Seminowicz DA, Burrowes SAB, Kearson A, et al. Enhanced mindfulness-based stress reduction in episodic migraine: a randomized clinical trial with magnetic resonance imaging outcomes. Pain. 2020;161(8):1837–1846. doi: 10.1097/j.pain.0000000000001860.
- Hatchard T, Mioduszewski O, Khoo E-L, et al. Reduced emotional reactivity in breast cancer survivors with chronic neuropathic pain following mindfulness-based stress reduction (MBSR): an fMRI pilot investigation. Mindfulness. 2021;12(3):751–762. doi: 10.1007/s12671-020-01546-9.
- Osypiuk K, Ligibel J, Giobbie-Hurder A, et al. Qigong mind-body exercise as a biopsychosocial therapy for persistent post-surgical pain in breast cancer: a pilot study. Integr Cancer Ther. 2020;19:1–12. doi: 10.1177/1534735419893766.
- Lutz A, McFarlin DR, Perlman DM, et al. Altered anterior insula activation during anticipation and experience of painful stimuli in expert meditators. Neuroimage. 2013;64(1):538–546. doi: 10.1016/j.neuroimage.2012.09.030.
- Zorn J, Abdoun O, Sonié S, et al. Cognitive defusion is a core cognitive mechanism for the sensory-affective uncoupling of pain during mindfulness meditation. Psychosom Med. 2021;83(6):566–578. doi: 10.1097/PSY.0000000000000938.
- Grant JA, Courtemanche J, Duerden EG, et al. Cortical thickness and pain sensitivity in zen meditators. Emotion. 2010;10(1):43–53. doi: 10.1037/a0018334.
- Grant JA, Courtemanche J, Rainville P. A non-elaborative mental stance and decoupling of executive and pain-related cortices predicts low pain sensitivity in zen meditators. Pain. 2011;152(1):150–156. doi: 10.1016/j.pain.2010.10.006.
- Gard T, Hölzel BK, Sack AT, et al. Pain attenuation through mindfulness is associated with decreased cognitive control and increased sensory processing in the brain. Cereb Cortex. 2012;22(11):2692–2702. doi: 10.1093/cercor/bhr352.
- Orme-Johnson DW, Schneider RH, Son YD, et al. Neuroimaging of meditation’s effect on brain reactivity to pain. NeuroReport. 2006;17(12):1359–1363. doi: 10.1097/01.wnr.0000233094.67289.a8.
- Brown CA, Jones AKP. Meditation experience predicts less negative appraisal of pain: electrophysiological evidence for the involvement of anticipatory neural responses. Pain. 2010;150(3):428–438. doi: 10.1016/j.pain.2010.04.017.
- Villemure C, Čeko M, Cotton VA, et al. Insular cortex mediates increased pain tolerance in yoga practitioners. Cereb Cortex. 2014;24(10):2732–2740. doi: 10.1093/cercor/bht124.
- Seeley WW. The salience network: a neural system for perceiving and responding to homeostatic demands. J Neurosci. 2019;39(50):9878–9882. doi: 10.1523/JNEUROSCI.1138-17.2019.
- Mehling WE, Gopisetty V, Daubenmier J, et al. Body awareness: construct and self-report measures. PLOS One. 2009;4(5):e5614. doi: 10.1371/journal.pone.0005614.
- van Aalst J, Jennen L, Demyttenaere K, et al. Twelve-Week yoga vs. Aerobic cycling initiation in sedentary healthy subjects: a behavioral and multiparametric interventional PET/MR study. Front Psychiatry. 2021;12:739356. doi: 10.3389/fpsyt.2021.739356.
- Suárez-Iglesias D, García-Porro M, Clardy A, et al. Feasibility and effects of a chair-based yoga program for adults with neurodisability. Disabil Rehabil. 2022;44(18):5220–5230. doi: 10.1080/09638288.2021.1933617.
- Neukirch N, Reid S, Shires A. Yoga for PTSD and the role of interoceptive awareness: a preliminary mixed-methods case series study. Eur J Trauma Dissociation. 2019;3(1):7–15. doi: 10.1016/j.ejtd.2018.10.003.
- Mehling WE, Price CJ, Daubenmier J, et al. The multidimensional assessment of interoceptive awareness (MAIA). PLOS One. 2012;7(11):e48230. doi: 10.1371/journal.pone.0048230.
- Kim D, Woo C-W, Kim S-G. Neural mechanisms of pain relief through paying attention to painful stimuli. Pain. 2022;163(6):1130–1138. doi: 10.1097/j.pain.0000000000002464.
- Zorn J, Abdoun O, Bouet R, et al. Mindfulness meditation is related to sensory-affective uncoupling of pain in trained novice and expert practitioners. Eur J Pain. 2020;24(7):1301–1313. doi: 10.1002/ejp.1576.
- Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. 1985;8(2):163–190. doi: 10.1007/BF00845519.
- Di Lernia D, Lacerenza M, Ainley V, et al. Altered interoceptive perception and the effects of interoceptive analgesia in musculoskeletal, primary, and neuropathic chronic pain conditions. J Pers Med. 2020;10(4):201. doi: 10.3390/jpm10040201.
- Ribera d’Alcalà C, Webster DG, Esteves JE. Interoception, body awareness and chronic pain: results from a case–control study. Int J Osteopath Med. 2015;18(1):22–32. doi: 10.1016/j.ijosm.2014.08.003.
- Valenzuela-Moguillansky C, Reyes-Reyes A, Gaete MI. Exteroceptive and interoceptive body-self awareness in fibromyalgia patients. Front Hum Neurosci. 2017;11:117. doi: 10.3389/fnhum.2017.00117.
- Hanley AW, Garland EL. Mapping the affective dimension of embodiment with the sensation manikin: validation among chronic pain patients and modification by Mindfulness-Oriented recovery enhancement. Psychosom Med. 2019;81(7):612–621. doi: 10.1097/PSY.0000000000000725.
- Cayoun B, Simmons A, Shires A. Immediate and lasting chronic pain reduction following a brief self-implemented mindfulness-based interoceptive exposure task: a pilot study. Mindfulness. 2020;11(1):112–124. doi: 10.1007/s12671-017-0823-x.
- Umeda M, Kim Y. Gender differences in the prevalence of chronic pain and leisure time physical activity among US adults: a NHANES study. Int J Environ Res Public Health. 2019;16(6):988. doi: 10.3390/ijerph16060988.
- Cramer H, Ward L, Steel A, et al. Prevalence, patterns, and predictors of yoga use: results of a U.S. Nationally representative survey. Am J Prev Med. 2016;50(2):230–235. doi: 10.1016/j.amepre.2015.07.037.
- Garfinkel SN, Seth AK, Barrett AB, et al. Knowing your own heart: distinguishing interoceptive accuracy from interoceptive awareness. Biol Psychol. 2015;104:65–74. doi: 10.1016/j.biopsycho.2014.11.004.