Abstract
Objective. To estimate the repeatability of radial pulse wave analysis (PWA) in measuring central systolic and diastolic blood pressures (cSBP/cDBP), pulse pressure (cPP), augmentation pressure (cAP) and pulse pressure amplification (PPA). Methods. After 15 min supine rest, 20 ambulant patients (aged 27–82 years; four female) underwent four SphygmoCor PWA measurements on a single occasion. Two nurses independently undertook two measurements in alternate order, blind to their colleague's measurements. Analysis was by Bland–Altman limits of agreement (LOA). Results. Heart rate and brachial blood pressure (BP) were stable during assessment. Based on the average of two PWA measurements between‐observer differences (LOA, mean difference±2SD) were small (cSBP 1.5±10.9 mmHg; cDBP 0.4±5.2 mmHg; cAP 0.5±4.5 mmHg; cPP 1.1±10.5 mmHg; PPA −0.5%±5.6%). Between‐observer differences were much greater for single/initial PWA measurement (cSBP 3.6±15.9 mmHg; cDBP 2.8±8.8 mmHg; cAP 0.7±5.8 mmHg; cPP 0.8±13.6 mmHg; PPA −1.2±9.4%). Within‐observer LOA were very similar for both nurse A (cSBP −4.2±14.1 mmHg; cDBP −4.6±13.1 mmHg; cAP −0.4±4.4 mmHg; cPP 0.5±11.0 mmHg; PPA 0.7%±9.0%) and nurse B (cSBP 0.0±12.1 mmHg; cDBP 0.2±8.5 mmHg; cAP −0.1±4.4 mmHg; cPP −0.2±11.9 mmHg; PPA −0.7%±10.6%). Conclusion. Non‐invasive assessment of central aortic pressures using PWA on a single occasion is highly repeatable in ambulant patients even when used by relatively inexperienced staff.
Introduction
Despite being subject to considerable measurement error the assessment of brachial blood pressure (BP) is a well‐established part of routine clinical practice Citation[1]. Brachial BP provides important prognostic information and is a central element of cardiovascular (CV) risk prediction, although which BP measurement (either alone or in combination) is the best predictor of future CV events is an area of active scientific debate Citation[2–4].
The traditional measurement of brachial BP can be viewed as a convenient surrogate for central aortic BP Citation[1], Citation[5]. Central aortic pressures may be of greater pathophysiological and clinical importance than brachial pressures, since left ventricular load depends upon central systolic pressure and coronary artery perfusion upon central diastolic pressure Citation[1], Citation[5]. Brachial BP may also be a poor indicator of central BP Citation[1]. The recent CAFE (Conduit Artery Function Evaluation) study has demonstrated that different anti‐hypertensive drugs can have very different effects on central BP, despite having a relatively similar effects on reducing brachial BP Citation[6]. The CAFE study assessed central BP using the SphygmoCor system, which employs pulse wave analysis (PWA) as non‐invasive method for measuring central aortic pressures without the need for cardiac catheterization Citation[1], Citation[6]. The SphygmoCor device has been widely used for research purposes and is commercially available for use in routine clinical practice Citation[1], Citation[6].
Clinical innovations do not always translate into the anticipated clinical benefits for patients seen in routine clinical practice Citation[7]. It is important that clinical innovations such as PWA are carefully evaluated in the settings in which they will be applied. The repeatability of measurements made using the SphygmoCor system are prone to two major sources of error. Firstly, it requires the skilled and consistent “applanation” (applied so as to flatten the side, but not occlude the artery) of a small hand‐held tonometer to the radial artery Citation[1]. Secondly, it is calibrated against the traditional brachial cuff measurement of BP, a technique known to be prone to high levels of measurement error Citation[1]. For PWA to be clinically useful, it needs to be demonstrated that it is a reproducible technique in the hands of healthcare staff using it in routine assessment.
The recent introduction of PWA into the clinical CV assessment of patients at Aberdeen Royal Infirmary (a 1000‐bed university teaching hospital) provided the opportunity to assess the repeatability of PWA when undertaken by nursing staff with limited previous experience of the technique. The aim of this study is to estimate the within‐observer and between‐observer repeatability on a single occasion of the measurement of central aortic BP using radial applanation tonometry and peripheral PWA.
Materials and methods
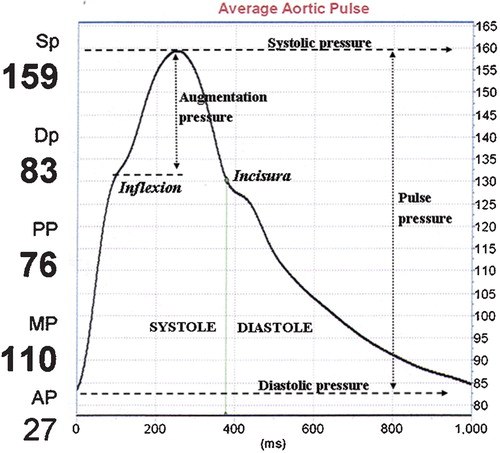
PWA using radial applanation tonometry is a non‐invasive method for measuring central aortic BP without the need for cardiac catheterization. A high‐fidelity tonometer is used to capture the shape of the radial pulse wave, which is calibrated against the brachial systolic/diastolic pressure (measured with a cuff). SphygmoCor employs a convolutional algorithm (a generalized transfer function) to derive the central aortic waveform and pressures Citation[1], Citation[8], Citation[9]. A typical aortic pulse wave (obtained from an older patient in this study) is shown in Figure . SphygmoCor identifies the first systolic shoulder resulting from the returning reflected wave (inflexion) and derives the central augmentation pressure (cAP). It also identifies the peak systolic pressure (cSBP) and the nadir of diastolic pressure (cDBP). The incisura indicates closure of the aortic valve.
Figure 1 Annotated central aortic pulse wave derived from pulse wave analysis(PWA) using the SphygmoCor system.
A consecutive series of 20 ambulant patients in sinus rhythm underwent PWA. Brachial BP and radial PWA were each measured a total of four times at a single visit to hospital. Two nurses independently undertook all BP/PWA measurements (BP left brachial artery; PWA right radial artery). Patients rested supine for 15 min, before each nurse (A and B) measured BP/PWA twice (each nurse measured brachial BP immediately prior to PWA) in alternate order (ABAB or BABA). Both nurses were registered general nurses with backgrounds in intensive care nursing and more than 20 years of clinical experience each. Prior to the start of this study, they attended a 2‐day theoretical/practical PWA course (6 months previously) and had practised PWA on a small number of work colleagues (approximately 35 PWA assessments before the start of this study).
BP was measured using a standard adult cuff at the left brachial artery (a large adult cuff was used if upper arm circumference was greater than 32 cm). Supine brachial BP was measured four times (two nurses alternating twice) using the Omron M5‐I IntelliSense BP monitor (HEM‐757 Omron Healthcare Inc.). This is an automated oscillometric BP monitor that has been independently validated against international criteria Citation[10]. A hand‐held tonometer (Millar, Texas, USA) was “applanated” to the right radial artery. The peripheral pulse wave was captured electronically on a laptop computer (10‐s recording period) using the SphygmoCor system (SCOR v 7.01, AtCor, Sydney, Australia). The quality of the captured pulse waves were assessed by the nurses visually on the computer screen and also numerically using the device's default in‐built quality index, QI% (based on pulse height, pulse height variation and diastolic variation; maximum QI score 100%). The nurses were trained to accept only high‐quality pulse wave traces: uninterrupted steep upstroke; second systolic shoulder before a sharp incursa; smooth diastolic exponential decline; and a QI% ⩾85% (based on pulse height ⩾100 units, pulse height variation ⩽5% and diastolic variation ⩽5%).
The nurses undertook all their measurements alone in a clinical side‐room at the hospital, ensuring that any marks left at the right wrist had disappeared before alternating. Each nurse was aware of their own BP/PWA measurements, but blind to their colleague's measurements. Other than current use of anti‐hypertensive medication, the nurses were unaware of a patient's previous medical history. All assessments were undertaken in a quiet temperature‐controlled side‐room at Aberdeen Royal Infirmary (22 July to 30 September 2004, between the hours of 08:30 and 15:30 h). Patients had not been asked to refrain from eating, drinking or smoking prior to assessment. They were not permitted to speak or sleep during the assessment.
Statistical approach
The unit of analysis is the individual patient. Data was double‐entered into SPSS (version 14) for analysis. No patients or outlying values were excluded. The Bland–Altman 95% limits of agreement (LOA) approach (mean difference±2SD) was used to assess within‐observer and between‐observer differences in paired measurements made on the same patient Citation[11], Citation[12]. This approach uses the standard deviation (SD) of the difference between means as an index of measurement error (twice the standard deviation, 2SD, is sometimes referred to as the coefficient of repeatability). It assumes that the best estimate of the true underlying value is the average of all four measurements and that observer differences are normally distributed over the range of measurements. The true mean difference between any measurements would only be zero if such measurements were perfectly repeatable Citation[11], Citation[12]. Standard methods (based on 19 degrees of freedom) were used to calculate 95% confidence intervals around mean differences Citation[13].
Results
The mean age of the 20 study participants (four female) was 56 years (range 27–82 years). Mean brachial BP was 136/79 mmHg with a pulse rate of 64 beats/min (Table ). Ten patients were on prescribed medication for essential hypertension (four mono‐therapy, four dual‐therapy and two triple‐therapy). All patients were in sinus rhythm. Excluding the initial 15‐min supine rest, PWA assessment took a mean (±SD) of 30±11.8 min (range 12–54 min) per patient with each patient undergoing four sequential measurements. For 12 patients, nurse assessment followed the sequence ABAB (eight patients BABA). Based on the average of two BP/PWA measurements, each nurse independently recorded very similar mean values for the study group (Table ). The quality of PWA recording was high with a mean quality index (QI%) of 97% (range 90–100%) that was similar for both nurses (96.9% and 97.3%).
Table I. Brachial oscillometric blood pressures, central aortic blood pressures and heart rate measurements obtained during pulse wave analysis study using radial applanation tonometry (n = 20).
The relative stability of brachial BP, pulse rate and quality index over time are shown in Figure . Between the first and fourth measurements made, brachial systolic/diastolic pressures declined by 4/3 mmHg. Heart rate (derived from the SphygmoCor machine) also declined by 2 beats/min between the third and fourth measurements. The quality of pulse wave recording (QI%) remained consistently high (Figure ). Brachial and aortic BPs, based on the average of all four measurements, are shown in Table . The mean central systolic/diastolic pressure (cSBP/cDBP) was 124/80 mmHg. The cAP was 12 mmHg and the central pulse pressure (cPP) 44 mmHg. Amplification of the cSBP (from 124 to 136 mmHg) and cPP (from 44 to 57 mmHg) at the brachial artery is apparent (Table ). Between‐ and within‐observer repeatability in the measurement of central pressures (and pulse pressure amplification, PPA) are shown in Table (a and b). Measurements with a wider range of values (Table ) consistently had wider LOA. For every 10‐point increase in the range of values, the LOA widened by an average of 1.3 mmHg.
Figure 2 Mean values of brachial oscillometric blood pressure, heart rate and pulse wave quality index during assessment.
Table II. Repeatability of central blood pressures and pulse pressure amplification derived from pulse wave analysis (PWA) using radial applanation tonometry (n = 20): (a) between‐observer repeatability (b) within‐observer repeatability.
Between‐observer differences are shown in Table . Taking the average of two PWA measurements, rather than relying on an initial PWA measurement, substantially reduced the SD of differences between observers. Central pressures derived from a single measurement generally showed larger differences than those derived from the average of two readings. When based on the average of two measurements, the absolute mean differences were small (⩽1.5 mmHg). The widest LOA was for cSBP based on a single measurement (−12 to +19 mmHg). This was reduced when cSBP was based on the average of two measurements (−9 to +12 mmHg). LOA for cDBP were considerably narrower than those for cSBP (Table ). Only the measurement of cAP showed little difference between observers, irrespective of whether it was based on a single measurement or the average of two measurements (LOA −5 to +7 mmHg vs −4 to +5 mmHg) (Table ).
Within‐observer differences, based on the two measurements made by each nurse on each patient, are shown in Table . Both nurses had similar LOA for cAP (approximately−4 to +4 mmHg) and cPP (−12 to +12 mmHg). Nurse B demonstrated the smallest within‐observer differences for cSBP and cDBP (mean differences of ⩽0.2 mmHg, with a lower SD for both). Nurse A had wider LOA for cSBP and cDBP than nurse B (cSBP −18 to +10 mmHg vs −12 to +12 mmHg; cDBP −18 to +10 mmHg vs −8 to +9 mmHg) (Table ).
Bland–Altman plots for PPA are shown in Figure . There was no increase in the variability of differences between measurements as the magnitude of PPA (or any other indices such as cSBP, cDBP, cPP, cAP) increased. The apparently wider LOA for within‐observer repeatability of PPA (as compared with between‐observer LOA) is related to taking the average of two measurements (as opposed to a single/initial measurement). All within‐observer and between‐observer mean differences were small (⩽1.2%) (Table ). Between‐observer LOA for PPA was −6% to +5% for the average of two measurements (single/initial measurement LOA was −11% to +8%). Within‐observer mean differences were similar both nurses (LOA of around −11% to +10%) (Table ).
Figure 3 Between‐observer and within‐observer differences in the measurement of pulse pressure amplification (PPA): limits of agreement (Bland–Altman) plots.
LOA were calculated for oscillometric brachial pressures recorded at the upper arm with the Omron M5‐I. A comparison of the central aortic LOA with the equivalent brachial LOA is shown in Figure . Between‐observer and within‐observer repeatability for central and brachial pressures (SBP, DBP, PP) had very similar LOA. Only the data for nurse A is shown (Figure ), but nurse B also demonstrated the same pattern (data not shown).
Discussion
Both within‐observer and between‐observer differences in the non‐invasive measurement of central pressures were small with no group mean differences exceeding 4.6 mmHg. The measurement of central pressures using radial applanation tonometry and PWA demonstrated levels of repeatability comparable to those for oscillometric brachial BP measurement using an internationally validated machine. The relatively new index of PPA also demonstrated similarly high levels of repeatability. Using the average of two PWA measurements, rather than relying on an initial PWA measurement, substantially reduced the SD of differences between observers.
We adopted a rigorous approach to our evaluation and took account of consensus guidelines concerning the performance of PWA Citation[14]. We ensured a stable haemodynamic state (and reduced variability) by initially resting all of the participants supine for 15 min in a quiet room. Two nurses using the same equipment, but blind to their colleague's measurements, independently undertook BP/PWA measurements. Other than drug therapy for hypertension, the nurses were also blind to the patient's past medical history. Brachial BP was recorded using a validated automatic oscillometric machine Citation[10], and PWA measurement was undertaken to a consistently very high standard. We intentionally collected only limited patient demographic data, since our principle interest was the repeatability of PWA, not the ability of PWA to distinguish between patients with or without specific medical conditions.
A limitation of our study is that the sequence of nurse assessment was alternate rather than random. The order of assessment depended upon which nurse was most readily available to undertake the first BP/PWA measurement. This is unlikely to have seriously biased our results. Patients initially assessed by nurse A were comparable with those initially assessed by nurse B (mean age 57 vs 56 years; BP 133/78 vs 140/79 mmHg; pulse rate 66 vs 61 beats/min). A second limitation is that we did not confirm that BP was the same in both arms. Radial PWA and brachial BP were measured on opposite arms simply because it was more convenient to place the Omron BP machine and SphygmoCor device on opposite sides of the patient. This will not have influenced our assessment of repeatability, since both nurses followed the same procedure for all patients. But for patients with a significant difference in BP between each arm, the miscalibration of the SphygmoCor device will have distorted the central aortic pressures obtained from the true value. Finally, since we assessed our patients at a single session, we have not accounted for within‐patient variability that would operate when assessing the same patient on more than one occasion, for example in monitoring changes in central pressures over time. It was also not feasible to avoid each nurse being aware of their own initial BP/PWA measurements when undertaking their second measurement and any resulting bias will tend to reduce within‐observer variability.
The high levels of repeatability achieved may relate to our nurses' previous experience of intensive care and a greater appreciation of the importance of careful clinical measurement.
Awareness that their performance was being scrutinized may also have influenced the nurses to be particularly diligent in their assessments. It is difficult to avoid such influences when undertaking a formal repeatability study, which requires a sequence of measurements being made in an identical manner. Levels of repeatability in less controlled circumstances are likely to be somewhat wider. The wider application of our findings is also limited by the fact that women made up only 20% of our study participants.
LOA is the most useful approach to the clinical assessment of repeatability Citation[11], Citation[12]. The number of patients we recruited is comparable with other published repeatability studies and provided a wide range of central BP values over which to assess repeatability (Table ). Our systematic search of the literature (Medline, Embase and Science Citation Index; last updated 30 March 2007) identified three published studies that have assessed the repeatability of central BP measurement using peripheral PWA Citation[5], Citation[15], Citation[16].
In a study involving two observers and 88 healthy hospital staff, the between‐observer repeatability (based on the average of two measurements) of cSBP (mean±2SD) was 3.3±18 mmHg (LOA −15 to +21 mmHg) Citation[15]. This is somewhat wider than our equivalent repeatability of 1.5±11 mmHg (LOA −9 to +12 mmHg). A second study measured central BP in 25 healthy volunteers on three separate occasions (a total of 75 measurements), but the pooled analysis takes no account of the paired nature of the data Citation[5]. The third study provides insufficient data to assess repeatability Citation[16]. Observer repeatability in the CAFÉ study (among technicians, physicians and nurses at five centres across the UK and Ireland) has not been reported Citation[6].
Research into the prognostic importance of the non‐invasive measurement of central BP using peripheral PWA is still at an early stage of development. It is not yet clear what additional information central BP measurement provides over and above that already available from traditional brachial BP measurement. Nor is it clear which are the most important central BP indices (including newer indices such as PPA) for predicting CV events. The recent CAFE study found similar levels of increased risk associated with central pulse pressure, cAP and peripheral pulse pressure (a relative risk increase of between 12% to 18% for every 10 mmHg increase in pressure) for a composite of CV outcome measures. The level of CV risk associated with these measures was similar for both men and women Citation[6], although a sub‐study of older hypertensive women in the second Australian National BP Study found brachial pulse pressure to be a much stronger predictor of CV events than central pulse pressure Citation[17].
In conclusion, PWA using radial artery applanation tonometry demonstrates an acceptable level of within‐observer and between‐observer repeatability for measuring central aortic pressures, even when used by nurses with limited previous experience of the technique. The level of repeatability of PWA is comparable with the oscillometric measurement of peripheral brachial BP. It is a technique that can be easily acquired for use in clinical practice, which adds supports to suggestions that PWA has the potential to be included in the routine assessment of ambulant patients.
References
- Nichols W. W., O'Rourke M. F. McDonald's blood flow in arteries: Theoretical, experimental and clinical principles. Hodder Arnold, London 2005, 5th ed
- Lewington S., Clarke R., Qizilbash N., Peto R., Collins R. Age‐specific relevance of usual blood pressure to vascular mortality: A meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903–1913
- Gasowski J., Fagard R. H., Staessen J. A., Grodzicki T., Pocock S., Boutitie F., et al. Pulsatile blood pressure component as predictor of mortality in hypertension: A meta‐analysis of clinical trial control groups. J Hypertens 2002; 20: 145–151
- Poulter N. R., Wedel H., Dahlof B., Sever P. S., Beevers D. G., Caulfield M., et al. Role of blood pressure and other variables in the differential cardiovascular event rates noted in the Anglo‐Scandinavian Cardiac Outcomes Trial‐Blood Pressure Lowering Arm (ASCOT‐BPLA). Lancet 2005; 366: 907–913
- Siebenhofer A., Kemp C., Sutton A., Williams B. The reproducibility of central aortic blood pressure measurements in healthy subjects using applanation tonometry and sphygmocardiography. J Hum Hypertens 1999; 13: 625–629
- Williams B., Lacy P. S., Thom S. M., Cruickshank K., Stanton A., Collier D., et al. Differential impact of blood pressure‐lowering drugs on central aortic pressure and clinical outcomes: Principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation 2006; 113: 1213–1225
- McKinlay J. B. From “promising report” to “standard procedure”: Seven stages in the career of a medical innovation. Milbank Mem Fund Q Health Soc 1981; 59: 374–411
- Pauca A. L., O'Rourke M. F., Kon N. D. Prospective evaluation of a method for estimating ascending aortic pressure from the radial artery pressure waveform. Hypertension 2001; 38: 932–937
- Gallagher D., Adji A., O'Rourke M. F. Validation of the transfer function technique for generating central from peripheral upper limb pressure waveform. Am J Hypertens 2004; 17((11 Pt 1))1059–1067
- El Assaad M. A., Topouchian J. A., Asmar R. G. Evaluation of two devices for self‐measurement of blood pressure according to the international protocol: The Omron M5‐I and the Omron 705IT. Blood Press Monit 2003; 8: 127–133
- Bland J. M., Altman D. G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1: 307–310
- Bland J. M., Altman D. G. Applying the right statistics: Analyses of measurement studies. Ultrasound Obstet Gynecol 2003; 22: 85–93
- Altman D. G., Machin D., Bryant T. N., Gardner M. J. Statistics with confidence: Confidence intervals and statistical guidelines. BMJ Books, London 2000, 2nd ed
- Van Bortel L. M., Duprez D., Starmans‐Kool M. J., Safar M. E., Giannattasio C., Cockcroft J., et al. Clinical applications of arterial stiffness, Task Force III: Recommendations for user procedures. Am J Hypertens 2002; 15: 445–452
- Filipovsky J., Svobodova V., Pecen L. Reproducibility of radial pulse wave analysis in healthy subjects. J Hypertens 2000; 18: 1033–1040
- Woodman R. J., Kingwell B. A., Beilin L. J., Hamilton S. E., Dart A. M., Watts G. F. Assessment of central and peripheral arterial stiffness: Studies indicating the need to use a combination of techniques. Am J Hypertens 2005; 18((2 Pt 1))249–260
- Dart A. M., Gatzka C. D., Kingwell B. A., Willson K., Cameron J. D., Liang Y. L., et al. Brachial blood pressure but not carotid arterial waveforms predict cardiovascular events in elderly female hypertensives. Hypertension 2006; 47: 785–790