Abstract
Background: Poor drug adherence is a major cause of apparent treatment-resistant hypertension. As a consequence, several methods have been developed and attempted implemented in clinical practice to reveal non-adherence and to monitor drug adherence. There are, however, several hitherto unresolved ethical aspects regarding potential methods for drug monitoring in these patients.
Results: The most striking challenge is the balance between patient autonomy and the physician’s desire for the patient to adhere to the prescribed therapy. Also, methods for monitoring must only be implemented in the treatment of well-informed and consenting patients. Major resources are used on non-adherent patients; how long the physician should encourage continuation of treatment is an important question.
Conclusions: We believe that physicians should reflect and discuss these potential challenges, and that patient education, information and a solid patient–physician relationship are essential for achieving drug adherence. Methods for monitoring adherence represent, however, a useful and often necessary supplement.
Introduction
Treatment-resistant hypertension, defined as blood pressure >140/90 mmHg despite the use of at least three antihypertensive drugs from different classes in highest tolerated doses, including a diuretic [Citation1], has gained renewed attention after introduction of invasive treatment methods, e.g. renal sympathetic denervation and baro-reflex stimulation. Still, with proper work-up and adjustment of medication according to guidelines, most patients achieve blood pressure control [Citation2], and are often characterized as having apparent treatment-resistant hypertension. Thus, poor drug adherence has emerged as a major cause of inadequate blood pressure control [Citation3], and there is a continuous on-going development of methods to monitor drug adherence in the treatment of hypertension [Citation4]. Non-adherence is complex in nature and it is hard to obtain evidence for interventions which substantially improve adherence [Citation5]. However, the most promising methods in revealing poor drug adherence in hypertensive patients are drug monitoring in body fluids and directly observed therapy (DOT) with subsequent ambulatory blood pressure measurement [Citation6]. However, with new methods to discover the patient’s behaviour, new ethical challenges arise ( and ). To our knowledge, these challenges have not yet been discussed in detail, at least not for this specific group of patients [Citation7]. Thus, we aimed to review the ethical aspects in the treatment of apparent treatment-resistant hypertension and also the ethical challenges by implementation of new methods to improve patient adherence in clinical practice.
Figure 1. Aspects in treatment of apparent treatment-resistant hypertension. Diagram showing important aspects that should be reflected upon in treatment of patients with apparent treatment-resistant hypertension. aTRH: apparent treatment-resistant hypertension; BP: blood pressure
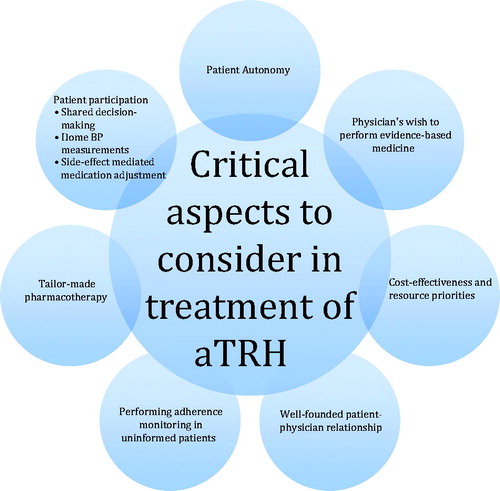
Table 1. Overview of aspects with potential ethical challenges in apparent treatment-resistant hypertension.
New methods for drug monitoring unveil ethical challenges
Drug monitoring in urine or blood samples
Drug monitoring, with quantification of drug metabolites in blood or urine samples, has gained widespread attention as an efficient method for revealing poor drug adherence. There is also a potential blood pressure lowering effect of being monitored [Citation8], especially if combined with subsequent patient education and other approaches to enhance compliance, known as therapeutic drug monitoring [Citation9]. Nonetheless, there are multiple ethical aspects to consider. In many studies using drug monitoring, the patients were unaware of the measurements. In daily patient care, uninformed sampling and measurements are not acceptable, and thorough discussion and informed consent is needed prior to the introduction of drug monitoring. In the setting of a clinical study, a detailed written, informed consent is needed and in clinical practice, the agreement with the patient should be documented by the physician in the patient’s electronic medical record.
It is reasonable to assume that the initial blood pressure lowering effect of drug monitoring and the increase in drug adherence may lose its effect over time. “White coat adherence” is a well-known phenomenon in treatment of hypertension [Citation3,Citation10,Citation11], and drug monitoring will not eliminate the possibility that patients adhere to treatment only during the immediate days prior to an appointment. An approach to overcome extensive white coat adherence and maintain an element of surprise is to not test at each consultation, and also increase the rate of consultations. Still, patients agreeing to this kind of follow-up may of course be adherent in the first place. Another important aspect to be aware of when using drug monitoring is that the method often is interpreted with a dichotomous result: The patient is compliant or the patient is non-compliant. Whether the patient takes all prescribed doses or only every second or third day cannot easily be assessed with this method. Nonetheless, with increasing knowledge on the pharmacokinetics of antihypertensives, patients may be differentiated into compliant, partly compliant or non-compliant. Drug monitoring is presently not included in routine assessment of hypertensive patients and larger intervention studies are needed to prove the effect on drug adherence and blood pressure control [Citation4]. How often drug monitoring should be performed in the follow-up of hypertensive patients is another important question that needs to be answered before implementation in daily clinical work. Low serum concentrations of antihypertensive drugs and their metabolites may also be caused by differences in absorption and drug metabolism, and must not automatically be interpreted as poor adherence by the physician [Citation12].
Directly observed therapy
Directly observed therapy (DOT) is another method to overcome the challenges of poor drug adherence [Citation6]. DOT is regularly and legitimately used in treatment of tuberculosis and severe psychiatric diseases. It is not difficult to justify the use of this method in the treatment of these specific conditions, due to the high risk of serious outcome both for the patients, the patients’ relatives and others. As emphasized below, hypertension is a condition of different character, and forced implementation of DOT would be ethically unacceptable and judicially impossible. In the case of tuberculosis treatment, DOT is limited in time, while antihypertensive treatment on the other hand is usually life-long. With the large number of possible candidates for DOT in mind, this method would be expensive and demand huge resources, making it difficult to implement in daily care of hypertensive patients. Therefore, DOT should be reserved for the assessment of difficult-to-control hypertension, as well as in later adjustment of medications, in well-informed and consenting patients [Citation3].
Another aspect of introducing DOT appears in patients with partial or complete non-adherence, when taking their prescribed medication during DOT: This could potentially lead to severe hypotension, resulting in syncope, acute kidney injury or other adverse complications. It must be considered unethical not to observe the patient after the DOT procedure in order to discover serious side effects.
Patient autonomy
Perhaps the most striking ethical aspect of the treatment of hypertensive patients is the fine balance between the physician’s encouragement to adhere to the prescribed therapy, and the respect for the patient’s autonomy. The patient’s right to participate in decision-making regarding his or her own health is in most countries statutory. And at the end of the day, it will always be the patient’s decision to take his or her medication, as long as the patient is considered to have competence to give informed consent.
Hypertension is a condition usually without signs or symptoms for years in the early phases, and it is therefore not difficult to understand why some patients do not see the need to take blood pressure lowering medication, resulting in poor drug adherence. Thus, the need for the physician to give adequate information on long-term complications is paramount. Information should be given in a manner and amount adjusted to the patients’ abilities to perceive the information. Patient education and information are time consuming and it is often necessary to repeat it regularly during treatment and follow-up. Nevertheless, this is a crucial part of the follow-up of hypertensive patients. It is essential that the patients are aware that relatively small drug interventions can substantially reduce the risk of severe disease in the future.
A major challenge concerning all patient education and thereby patients’ ability to participate in decision-making, is the difficulties of risk communication. What patients consider being high or low risk may be subject to substantial inter-individual differences. Wennberg et al. propose to divide decisions into “effective” and “preference-sensitive” treatment, where “effective” refers to evidence-based and well-founded medical care in which the benefit of treatment outweighs the potential harm, whereas the latter refers to decisions where at least two equally qualified options are available [Citation13]. The two different scenarios require different communication [Citation14]. For patients who are candidates for “effective” treatment, implementation difficulties should be assessed, and motivational interviewing could be used to inform, motivate and overcome barriers to treatment. Information to patients with “preference-sensitive” therapy should be more thorough and less normative. Still, with different perception of risk, the two categories may differ between patients. This also relates to hypertensive patients and will make patient education more difficult.
In recent research, assessment of filled drug prescriptions has been used in order to investigate adherence [Citation15,Citation16]. This method is based upon prescription registries and comparison of estimated use of medication and how often the patients collect their medication [Citation6]. This method will also challenge patient autonomy and confidentiality. The physician cannot assess prescription fill rates without the patient’s approval, and the method is best suited for population studies after approval by Ethics Committees. However, filled prescriptions are no guarantee for actual intake of the drugs prescribed.
Patient–physician relationship in antihypertensive treatment
It is important that the patients have the opportunity to discuss the various aspects of the treatment that they find challenging with their physician. This could be side effects considered unreasonably adverse compared to the expected effect of treatment, or in simpler cases, challenges regarding administration of medications. Clarifying and overcoming these difficulties together may increase drug adherence [Citation9]. Other reasons for poor drug adherence may be lack of trust in conventional medicine, patients wanting to try lifestyle interventions or alternative medicine instead of pills, economic challenges, difficulties concerning oral intake of pills or other reasons. It is the physician’s responsibility to reveal barriers to the treatment and discuss these with the patients. Informing the patient about the benefit, not only for the individual, but also for the society, of treating hypertension, might contribute to the patients understanding of the importance of treatment and potentially lead to increased adherence. However, doing so requires cautiousness so that the patient does not experience any kind of pressure from the physician to comply against his or her wishes.
Physicians are also obliged to adapt treatment in order to facilitate increased adherence for the patients. Most important is choosing medications with (1) tolerable or optimally, no side effects, (2) combination therapy instead of regimens with multiple pills, (3) drugs taken once daily and (4) dosages and medications with synergistic rather than additive effect [Citation17]. Challenges regarding one treatment regimen may be worrisome for some patients and irrelevant for others, and vice versa, and the physician has no foundation for deciding the best treatment without involving the patient [Citation18]. The treatment should therefore be tailored to each patient’s needs, and treatment according to “one size fits all” is not recommendable. Interdisciplinary collaboration with nurses and pharmacists is of uttermost importance.
Monitoring of the patient’s adherence with drug monitoring or DOT may be interpreted by the patient as mistrust from the physician, and will possibly affect the relationship between them. The major challenge in monitoring drug adherence is in fact the underlying suspicion, legitimate or not, that the patient does not follow recommended therapy. Therefore, a well-founded patient–physician relationship, information and cooperation are of pivotal importance if drug monitoring or DOT is to be used. The mandatory information prior to drug monitoring might also represent an opportunity to avoid a sense of mistrust in the patient. It is important that the patient understands the potential benefit from using the method, agrees to use it and thereby taking part in treatment progress. Mascharenas et al. provide a comprehensive review of the trust-distrust topic, with examples from elderly patients with chronic conditions [Citation19]. The authors discuss numerous psychological and behavioural theories trying to explain reasons for distrust and its impact on patient–physician relationship. Based on their hypotheses, several aspects must be addressed to increase trust between patient and physician. The patient needs to sense that the physician have the patients’ best interest as goal, without conflicting interest. One should make clear that increased compliance is not the main target, and instead focus on the potential risk reduction of pharmacotherapy, hence promoting drug adherence. Another way of decreasing distrust is by encouraging patient cooperation. Therefore, treatment that increases the patient’s control and contribution should be used. The use of home blood pressure monitoring with patients’ own measurement devices have improved both adherence and blood pressure control [Citation20]. We believe that this approach is beneficial also in treatment of patients with apparent treatment-resistant hypertension.
It is also worth mentioning that drug monitoring is used in other parts of medicine where the risk of mistrust and an impaired patient–physician relationship is not even a topic. Drug monitoring is for instance used in treatment with ciclosporin, digoxin, aminoglycosides and lithium. Most physicians would agree to the benefit of drug monitoring, due to low therapeutic index. A possible answer to this paradox might be that the physician believes serum concentrations outside the therapeutic window to be due to pharmacokinetic differences out of the patient’s control, in contrast to adherence to antihypertensive drugs. By performing drug monitoring without presenting non-adherence as a reason for testing, but rather as a control of treatment effect, the distrust between patient and physician might be overcome.
Cost-effectiveness and health care priorities
In addition to the ethical aspects regarding monitoring of patients with poor drug adherence, another important issue to discuss is for how long time the physician and other health workers should encourage the patient to take prescribed medication if the patient does not seem to change behaviour. Antihypertensive treatment is in many countries subsidized by governmental support. With the knowledge of the extensive challenge poor drug adherence represents in patients with apparent treatment-resistant hypertension, it may seem that large resources are wasted, not only on untaken medications, but also on consultations at the general practitioner’s office and in specialist health care, radiological diagnostics and hormone analyses. Is it thus an option to cease treatment of patients with poor drug adherence? This cannot be done without utmost caution. If choosing to permanently discontinue pharmacological antihypertensive treatment, it is imperative to ensure complete non-adherence and that the decision is made with the patients’ informed consent, and after all other means to increase adherence and obtain blood pressure control have been attempted including offering the patient professional psychological consulting in order to overcome their resistance.
Drug monitoring seems to increase adherence and reduce blood pressure, but it is uncertain whether the effect is transient or persisting. Most likely, the blood pressure lowering effect is only sustained as long as drug monitoring is performed. Nonetheless, despite scarce research on the topic, drug monitoring seems to be cost-effective, even with only 10 mmHg reduction in blood pressure, or if only half of the patients benefit from the method [Citation21]. This provides another argument in favour of performing drug monitoring in patients with apparent treatment-resistant hypertension.
Non-adherent patients also demand resources when complications to untreated hypertension occur. Examples are acute treatment, rehabilitation and secondary prevention after stroke, heart failure, percutaneous or surgical revascularization of coronary arteries or dialysis or transplantations for chronic kidney disease. One cannot predict a priori which patients who would need to undergo these therapies regardless of their elevated blood pressure, but on a population basis, it is established that proper antihypertensive treatment reduces incidence of the abovementioned conditions at a cost-effective or even cost-saving level [Citation22]. This provides even further evidence defending a proactive approach from the physician’s side. However, this is one of the main challenges of primary prevention aiming for the middle-risk population: a relatively small intervention on population basis may reduce the burden of disease in the population, but the intervention may be regarded as a considerable implication on the patients’ life and felt unreasonably large compared to the expected benefit [Citation23].
Non-adherent patients are not a novel challenge to health care providers, and will continue to remain so in the future. The main questions are how the physician should encourage the patient to take their drugs, for how long the physician should attempt to ensure optimal health care for the patients, and to which extent the patients should take responsibility for their own health. By establishing good patient–physician relationships and focusing on proper patient education and information adapted to the patients’ level of understanding and in a language that the patients are familiar with, if necessary using an interpreter, clinicians may be better prepared when facing the ethical challenges presented above.
In this overview, we have discussed some of the ethical aspects physicians encounter in the treatment of patients with hypertension and particularly in the patients with apparent treatment-resistant hypertension (). Some of these aspects are also relevant in the treatment of other chronic conditions, e.g. diabetes mellitus and dyslipidaemia. Physicians should reflect on these potential challenges and keep them in mind in their clinical work. By doing so, the goal is to provide the best care for the patients.
Acknowledgements
The authors gratefully acknowledge the assistance and expert advice of Ulla Hjørnholm and Vibeke Kjær of the Section of Cardiovascular and Renal Research, and they thank prof. Sverre E. Kjeldsen of the Department of Cardiology, Oslo University Hospital, Ullevaal, for commenting upon this article.
Disclosure statement
FEMFE has received lecture honoraria from Hemo Sapiens, Medtronic and Amgen. AH has received lecture honoraria from Merck, Sharpe & Dome and Amgen. JEM, PAE, SH, ACL and PN declare no conflicts of interest.
References
- Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51:1403–1419.
- Fadl Elmula FE, Hoffmann P, Larstorp AC, et al. Adjusted drug treatment is superior to renal sympathetic denervation in patients with true treatment-resistant hypertension. Hypertension. 2014;63:991–999.
- Heimark S, Eskås PA, Mariampillai JE, et al. Tertiary work-up of apparent treatment-resistant hypertension. Blood Press. 2016;25:312–318.
- Berra E, Azizi M, Capron A, et al. Evaluation of adherence should become an integral part of assessment of patients with apparently treatment-resistant hypertension. Hypertension. 2016;68:297–306.
- McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA. 2002;288:2868–2879.
- Eskås PA, Heimark S, Mariampillai JE, et al. Adherence to medication and drug monitoring in apparent treatment-resistant hypertension. Blood Press. 2016;25:199–205.
- Bernardini J. Ethical issues of compliance/adherence in the treatment of hypertension. Adv Chronic Kidney Dis. 2004;11:222–227.
- Burnier M, Schneider MP, Chiolero A, et al. Electronic compliance monitoring in resistant hypertension: the basis for rational therapeutic decisions. J Hypertens. 2001;19:335–341.
- Brinker S, Pandey A, Ayers C, et al. Therapeutic drug monitoring facilitates blood pressure control in resistant hypertension. J Am Coll Cardiol. 2014;63:834–835.
- Persu A, Jin Y, Baelen M, et al. Eligibility for renal denervation: experience at 11 European expert centers. Hypertension. 2014;63:1319–1325.
- Mancia G, Bombelli M, Brambilla G, et al. Long-term prognostic value of white coat hypertension: an insight from diagnostic use of both ambulatory and home blood pressure measurements. Hypertension. 2013;62:168–174.
- Zisaki A, Miskovic L, Hatzimanikatis V. Antihypertensive drugs metabolism: an update to pharmacokinetic profiles and computational approaches. Curr Pharm Des. 2015;21:806–822.
- Wennberg JE, Fisher ES, Skinner JS. Geography and the debate over Medicare reform. Health Aff (Millwood). 2002;Suppl Web Exclusives:W96–W114. Available from: http://content.healthaffairs.org/content/early/2002/02/13/hlthaff.w2.96.full.pdf [last accessed 18 Nov 2016].
- O’Connor AM, Legare F, Stacey D. Risk communication in practice: the contribution of decision aids. BMJ. 2003;327:736–740.
- Qvarnström M, Kahan T, Kieler H, et al. Persistence to antihypertensive drug treatment in Swedish primary healthcare. Eur J Clin Pharmacol. 2013;69:1955–1964.
- Weitzman D, Chodick G, Shalev V, et al. Prevalence and factors associated with resistant hypertension in a large health maintenance organization in Israel. Hypertension. 2014;64:501–507.
- Burnier M, Wuerzner G, Struijker-Boudier H, et al. Measuring, analyzing, and managing drug adherence in resistant hypertension. Hypertension. 2013;62:218–225.
- Forrow L, Wartman SA, Brock DW. Science, ethics, and the making of clinical decisions. Implications for risk factor intervention. JAMA. 1988;259:3161–3167.
- Mascarenhas OA, Cardozo LJ, Afonso NM, et al. Hypothesized predictors of patient-physician trust and distrust in the elderly: implications for health and disease management. Clin Interv Aging. 2006;1:175–188.
- Parati G, Stergiou GS, Asmar R, et al. European Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens. 2008;26:1505–1526.
- Chung O, Vongpatanasin W, Bonaventura K, et al. Potential cost-effectiveness of therapeutic drug monitoring in patients with resistant hypertension. J Hypertens. 2014;32:2411–2421.
- Cost-effectiveness of hypertension therapy according to 2014 guidelines. N Engl J Med. 2015;372:1677.
- Rose G. Strategy of prevention: lessons from cardiovascular disease. Br Med J (Clin Res Ed). 1981;282:1847–1851.
