Abstract
Objectives: Suboptimal medication adherence is common among patients with hypertension. Measurements of plasma or urinary levels of antihypertensive drugs are useful, but not widely available. The aim of our study was to investigate the relation of patients’ heart rates to their serum beta-blocker levels.
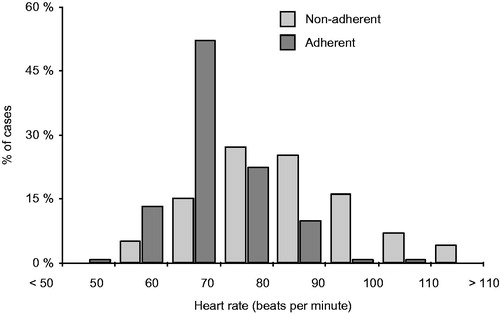
Methods: We correlated 220 measurements of serum beta-blocker levels in 106 patients with apparently resistant hypertension to their corresponding office heart rate. A significant proportion, 44.6% of patients, were non-adherent to beta-blocker treatment according to serum level measurement. Non-adherent patients had significantly higher heart rates (80.9 vs. 66.6 bpm, p < .001), systolic (157.4 vs. 147.0 mm Hg, p = .002) and diastolic blood pressure (91.1 vs. 87.2 mm Hg, p = .041) in comparison to adherent patients.
Results: Heart rate above 75.5 beats per minute predicted non-adherence to beta-blocker treatment with a sensitivity of 62.5%, specificity 86.8% and AUC ROC 0.802 (p < .001). Higher heart rate cutoff might be applicable for nebivolol but was not determined due to the low number of patients treated with nebivolol.
Conclusions: We concluded that heart rate was shown to be a good predictor of non-adherence to beta-blocker treatment, and might become a quick and easy measure to determine patient adherence in hypertensive patients.
Introduction
Arterial hypertension is the world’s leading preventable cause of cardiovascular disease morbidity and mortality [Citation1]. Lowering blood pressure (BP) with antihypertensive drug therapy has been shown to significantly lower the risk of coronary heart disease, stroke and also all-cause mortality [Citation2].
A crucial factor in the treatment of hypertension is patient compliance or adherence to treatment. Suboptimal medication adherence is common among hypertension patients, with studies reporting non-adherence rates in patients of 25–53% [Citation3–8], leading to worse blood pressure control and higher occurrence of cardiovascular events [Citation9,Citation10].
Diagnosis of non-adherence is not easy [Citation11]. Counting pills is more reliable in clinical studies than in real life. Electronic containers for medicines, which record each time a box is opened by the patient [Citation12], are also not commonly available. A useful option in clinical practice is directly observed therapy with subsequent office or ambulatory monitoring of blood pressure immediately after the controlled administration of morning medication [Citation5,Citation13]. Measurements of plasma or urinary levels of antihypertensive drugs are very accurate and are therefore becoming a golden standard [Citation4,Citation8,Citation14]. However, these measurements are only available in a limited number of hospitals and laboratories and their costs are not negligible.
High heart rate in patients taking beta blockers is assumed to be an indirect marker of non-adherence. To the best of our knowledge, no particular heart rate cut-off has been defined in the literature to identify non-adherence. The aim of our study was to evaluate the ratio of the non-adherent patients in our hypertension center according to plasma levels of beta blockers and to study the relation of the plasma levels to patients’ office heart rate.
Methods
We performed a retrospective analysis of consecutive patients with apparently resistant arterial hypertension who had had beta-blocker levels measured to assess adherence to the recommended medical therapy. All patients were referred to and followed-up at our outpatient Hypertension Unit (European Society of Hypertension Excellence Center) at the Department of Internal Medicine I – Cardiology, University Hospital Olomouc.
Arterial hypertension was defined as resistant according to the American Heart Association (AHA) if a patient failed to achieve target blood pressure (BP) despite regime measures and adequate doses of at least three different classes of antihypertensive drugs, one of which was a diuretic, or the target BP was reached with a combination of four or more different antihypertensives [Citation15].
All patients underwent a clinical investigation during an outpatient visit, including a detailed patient history analysis and physical examination. Sitting blood pressure was measured three times by a calibrated mercury sphygmomanometer and the value was recorded as the average of the 2nd and 3rd measurements [Citation16]. Sitting heart rate was measured using stop watch and recorded by one minute pulse palpation on the radial artery after the third measurement of BP. Heart rate was measured on the same day as betablocker dosage.
We included only patients who confirmed regular intake of antihypertensive medication including the beta blocker and also stated its use at least 2 hours before blood sampling in the morning. We asked every patient to state regular intake of antihypertension drugs. Answers were recorded in patients medical report. Patients with atrial fibrillation, other arrhythmias or stimulated rhythm were excluded.
Blood samples for serum levels of beta blockers were taken during an outpatient visit from seated patients together with samples for other routine analyses. Patients were not informed before the clinical visit and blood sampling that analysis of used antihypertensive drugs will be performed. All patients stated their agreement with use of blood test results for science purpose during first outpatient visit in our hospital. Written consent with this procedure was collected. No additional consent with plasma drug level measurements was requested by local Ethic committee.
The blood samples (serum) were prepared by liquid-liquid extraction (LLE). All analyses were carried out using a UHPLC UltiMate 3000 RSLC System (Dionex, Sunnyvale, CA, USA) connected with a UHR-TOF Maxis Impact HD (Bruker Daltonics, Billerica, MA, USA). Chromatographic separations were performed at 40 °C on a reverse phase analytical column Acclaim RS 120 (Thermo Fisher Scientific, Waltham, MA, USA). The chromatographic conditions were: injection volume 5 μL; flow rate 0.5 mL/min; gradient elution; total runtime 6 min. UHR-TOF Maxis Impact HD equipped with an electrospray-ionisation source (ESI) operated in the positive MS mode.
Serum levels of beta blockers were measured repeatedly in the majority of patients, the minimal time difference between the two measurements in a single patient was three months. Therapeutic levels were defined by the laboratory according to the literature and the method used (please see ) [Citation17].
Table 1. Therapeutic and toxic serum ranges of different beta blockers.
A patient was classified as adherent at the particular measurement if the serum level was within therapeutic range. A patient was classified as non-adherent if the serum level was below the therapeutic range or undetectable. The detected serum level of beta blocker was compared with heart rate.
Median with 5th and 95th percentile values and mean with standard deviation were used for the description of continuous variables; the statistical significance of differences between groups of patients was tested using Mann-Whitney U test. ROC analysis was adopted for the analysis of the predictive power of heart rate for the identification of patients not using beta blockers and the definition of optimal heart rate cutoffs and their description using sensitivity and specificity. Statistical analysis was computed using SPSS 23.0.0.1 (IBM Corporation, New York, U.S.A.).
Results
Between January 2011 and December 2014 we performed 220 measurements of serum beta-blocker levels in 106 patients. Mean patient age was 56.8 years and 56% were men. Mean office systolic blood pressure was 151.7 mm Hg and diastolic blood pressure 89.0 mm Hg. Mean office heart rate was 73.0 beats per minute. Patients were using a mean of 5.5 antihypertensive drugs.
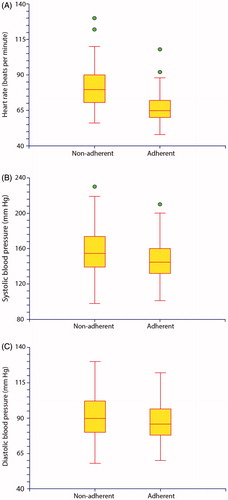
Only 55.4% of betablocker serum level measurements were within the therapeutic range, thus we classified these patients as adherent and the remaining 44.6% as non-adherent. There was a statistically significant difference in heart rate detected between the group of non-adherent patients (80.9 bpm) and adherent patients (66.6 bpm), p < .001 (please see and ).
Figure 1. Box-Whisker plots showing distribution of heart rate (A), systolic blood pressure (B) and diastolic blood pressure (C) in adherent and non-adherent patients.
There was no significant difference in heart rate between the group of patients whose beta-blocker levels were below the therapeutic range (79.8 bpm) and the group with undetectable levels (81.1 bpm), p = .179. Therefore, these two groups were merged for further analyses.
Systolic blood pressure in non-adherent patients was significantly higher than in adherent patients (157.4 vs. 147.0 mm Hg, p < .002) and diastolic pressure was also higher (91.1 vs. 87.2 mm Hg, p = .041) (, ). We found no significant difference between non-adherence in men and woman. ()
Table 2. Comparison of clinical characteristics of adherent and non-adherent patients.
Table 3. Comparison of non-adherence in men and women.
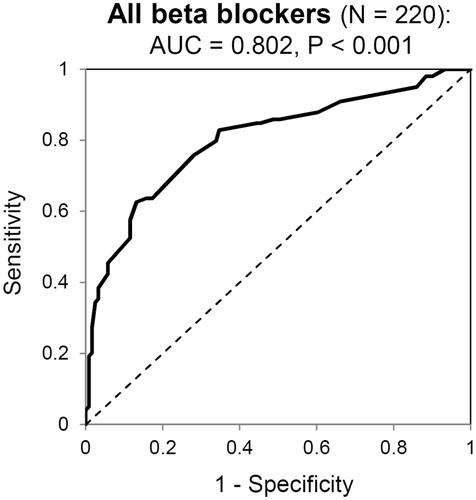
The receiver operator characteristics (ROC) analysis identified that a heart rate above 75.5 beats per minute predicted non-adherence with 62.5% sensitivity and 86.8% specificity, the area under the curve (AUC ROC) was 0.802 (p < .001) (please see ).
Figure 2. ROC analysis of the predictive power of heart rate to diagnose non-adherence in patients taking beta blockers. (AUC: area under the curve)
A separate ROC analysis was then performed for different beta blockers (, ). We found different heart rate cut-offs identifying non-adherence to different beta blockers. The lowest heart rate cut-off was found for bisoprolol (≥68.5 bpm, p < .001), the highest for nebivolol (≥81.5 bpm, p = .185). Mean dosage of beta blockers used in study with range and % of optimal dose is summarized in .
Figure 3. ROC analyses of the predictive power of heart rate to diagnose non-adherence in patients taking different types of beta blockers. (AUC: area under the curve).
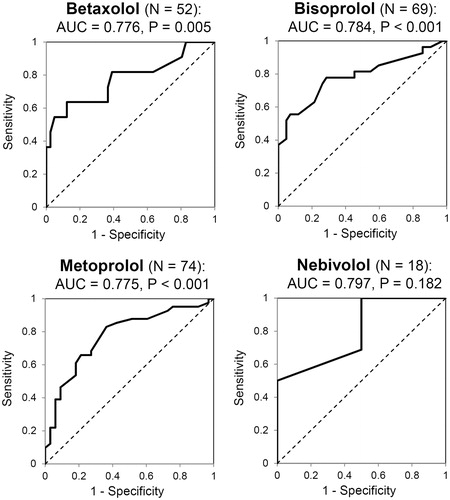
Table 4. Predictive power of heart rate for identification of patients not using beta blockers.
Table 5. Mean dosage of beta blockers used in study with range and % of optimal dose.
There was 24-hour ambulatory blood pressure monitoring (ABPM) available in 123 cases. We did the analysis of predicting non-adherence with heart rate derived from ABPM. (). The receiver operator characteristics (ROC) analysis identified that 24 hour average heart rate above 71,5 beats per minute predicted non-adherence with 63,3% sensitivity and 68.8% specificity (p < .001) and day time average heart rate above 77.5 beats per minute predicted non-adherence with 46,9% sensitivity and 87,5% specificity. The area under the curve (AUC ROC) was 0.700 (p < .001) for both ABPM derived cut-offs.
Table 6 Comparison of predictive power of office heart rate, 24 ABPM derived average heart rate and Day time ABPM average heart rate.
a. Relationship between not using medication and office heart rate.
b. Relationship between not using medication and heart rate derived from 24-hour ambulatory blood pressure measurements - 24 hour heart rate average.
c. Relationship between not using medication and heart rate derived from 24-hour ambulatory blood pressure measurements - Day time heart rate average.
We evaluated changes in long term adherence in patients with repeated testing. The minimum time difference between single measurements in one patient was 3 month. In 39 patients (56% of men) we performed total of 146 measurements of serum beta-blocker level with average of 3.74 (+− 1.56) measurements per each patient. The change in adherence status was revealed in 180 patients (46%). The majority of the patients with at least once confirmed nonadherence (56%) varied in compliance unpredictably and their status changed from adherent to nonadherent or vice versa during the follow up. The remaining 44% of nonadherent patients never had the serum level of beta-blocker in the therapeutic range, and thus were classified as nonadherent during the whole follow up. We compared portion of nonadherence in first and last visit and we found decreasing nonadherence by 17%. (56% in first and 38% in last visit).
Discussion
This study found that heart rate was a good predictor of non-adherence to beta-blocker treatment in patients with resistant hypertension. A heart rate of more than 75.5 beats per minute was highly predictive of non-adherence to most beta blockers with a high specificity of 86.8%. For nebivolol, the cutoff heart rate for non-adherence seemed to be somewhat higher at 81.5 bpm. ABPM related values of 24 hour average and day time average were also derived, but the results are inferior to office heart rate measurement. Smaller number of patients with available ABPM in our study is a handicap, but cutting of the stress elevation of heart rate in patients taking beta blocker is another potential explanation for better identification of non-adherence with office heart rate.
To the best of our knowledge, this is the first study to assess office heart rate in relation to serum levels of beta blockers. Since heart rate can be measured in all patients encountered in clinical settings, this might become a quick, cheap and easy measure to determine adherence in hypertensive patients treated with beta blockers. Even if heart rate measurement is not direct proof of non-adherence, defining the cutoff could reveal a subgroup of patients deserving closer attention and more detailed testing.
Measurement of serum or urinary levels of antihypertensive drugs may provide a more exact assessment of adherence [Citation4,Citation8,Citation14], but this method has significant costs and is not widely available to clinicians. Despite the cost of the analysis, a recent study showed that therapeutic drug monitoring presented a potential cost-effective healthcare intervention in patients diagnosed with resistant hypertension, independent of sex and age [Citation18].
The number of patients shown to be non-adherent to beta-blocker treatment by laboratory measurement of plasma levels in our study (44.6%) is similar to other published studies [Citation4–6,Citation14]. This number is high and alarming, as is the lack of widely-available precise methods for the assessment of adherence. With many effective antihypertensive drugs currently available, in the near future both researchers and physicians should focus more on the evaluation and improvement of medication adherence, which in turn may lead to improved hypertension control and patient prognosis [Citation19,Citation20].
Office systolic and diastolic BP values were also significantly higher in non-adherent patients by a mean of 10.4/3.9 mmHg. Non-adherence to another prescribed medication is likely, although it was not studied in this work. Unfortunately, since BP depends on many clinical factors and variables and the overlap of both groups was high (), it is very difficult to identify a BP cut-off usable to assess patient adherence in clinical practice. In our practice, however, we noted that in patients presenting with high office BP (e.g. >170/105 mm Hg) despite a combination of five or six antihypertensive drugs in adequate doses, non-adherence to one or more drugs proven by subsequent laboratory evaluation is very common.
Adherence to treatment depends on many factors, such as actual patient priorities, their financial situation or any kind of new information of positive or negative educational quality. Therefore, non-adherence has to be seen as a dynamic phenomenon which changes with time. In a secondary analysis of our study, we found a change of adherence status in 46% of patients during repeated testing. Improved adherence was closely related to improved hypertension control and vice versa. This phenomenon surely deserves further research, since data on medication adherence variability, its changes over time and methods for improvement is very limited, if not completely absent.
Patient – physician relationship is an important issue in long term adherence reaching. Our six year experience shows, that even in patients directly confronted with zero level of antihypertensives we can achieve a fair relationship, if we don´t judge but try to solve particular reason for not adhering to medication. A big portion of those patients appreciate our effort to help. Some of them accept psychological advice which is routinely offered in our hospital, some of them agree with change of medication if adverse effects are the problem, some of them need only proper education and explanation of the disease complications and drug effects. If repeated samples in one patient were taken, adherence increased. This endorses our hypothesis that repeated testing, education, solving problems and building closer relationship between the patient and the physician improves adherence.
The limitation of our study is retrospective design and a relatively small number of patients and laboratory measurements. Studies of more patients using nebivolol are particularly necessary to determine a more exact heart rate cut-off to predict non-adherence to this drug.
Secondly, patients with resistant hypertension were enrolled, in whom non-adherence to treatment may be more common than in general hypertensive patients. A systematic review identified that when electronic monitoring of antihypertensive medication was used, the adherence was relatively high, over 80% [Citation21]. Further studies are necessary to assess adherence in general hypertensive patients by serum or urinary measurements of administered drugs.
Perspectives
We conducted the first ever study to correlate office heart rate with serum levels of beta blockers in 106 patients with seemingly resistant hypertension. A heart rate of more than 75.5 beats per minute was shown to be a good predictor of non-adherence to beta-blocker treatment and might become a quick and easy measure to determine patient adherence in hypertensive patients. Our study also confirmed a high degree of non-adherence to treatment in these patients, present in 44.6%, which was associated with significantly higher BP values and worse BP control. Further methods to assess treatment adherence and especially interventions to improve patient adherence to medication are needed.
Disclosure statement
None declared.
References
- Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260.
- Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–967.
- Burnier M, Schneider MP, Chioléro A, et al. Electronic compliance monitoring in resistant hypertension: the basis for rational therapeutic decisions. J Hypertens. 2001;19:335–341.
- Jung O, Gechter JL, Wunder C, et al.. Resistant hypertension? Assessment of adherence by toxicological urine analysis. J Hypertens. 2013;31:766–774.
- Fadl Elmula FEM, Hoffmann P, Larstorp AC, et al. Adjusted drug treatment is superior to renal sympathetic denervation in patients with true treatment-resistant hypertension. Hypertension. 2014;63:991–999.
- Moise N, Schwartz J, Bring R, et al. Antihypertensive drug class and adherence: an electronic monitoring study. Am J Hypertens. 2015;28:717–721.
- Tomaszewski M, White C, Patel P, et al. High rates of non-adherence to antihypertensive treatment revealed by high-performance liquid chromatography-tandem mass spectrometry (HP LC-MS/MS) urine analysis. Heart. 2014;100:855–861.
- Strauch B, Petrák O, Zelinka T, et al. Precise assessment of noncompliance with the antihypertensive therapy in patients with resistant hypertension using toxicological serum analysis. J Hypertens. 2013;31:2455–2461.
- Mazzaglia G, Ambrosioni E, Alacqua M, et al. Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation. 2009;120:1598–1605.
- Yiannakopoulou EC, Papadopulos JS, Cokkinos DV, et al. Adherence to antihypertensive treatment: a critical factor for blood pressure control. Eur J Cardiovasc Prev Rehabil. 2005;12:243–249.
- Burnier M, Wuerzner G, Struijker-Boudier H, et al. Measuring, analyzing, and managing drug adherence in resistant hypertension. Hypertension. 2013;62:218–225.
- Waeber B, Feihl F. Assessment of drug compliance in patients with high blood pressure resistant to antihypertensive therapy. Euro Intervent. 2013;9(Suppl R):29–34.
- Hameed MA, Tebbit L, Jacques N, et al. Non-adherence to antihypertensive medication is very common among resistant hypertensives: results of a directly observed therapy clinic. J Hum Hypertens. 2016;30:83–89.
- Ceral J, Habrdova V, Vorisek V, et al. Difficult-to-control arterial hypertension or uncooperative patients? The assessment of serum antihypertensive drug levels to differentiate non-responsiveness from non-adherence to recommended therapy. Hypertens Res. 2011;34:87–90.
- Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation. 2008;117:e510–e526.
- Mancia G, De Backer G, Dominiczak A, et al. 2007 guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25:1105–1187.
- Schulz M, Iwersen-Bergmann S, Andresen H, et al. Therapeutic and toxic blood concentrations of nearly 1000 drugs and other xenobiotics. Crit Care. 2012;16:R136.
- Chung O, Vongpatanasin W, Bonaventura K, et al. Potential cost-effectiveness of therapeutic drug monitoring in patients with resistant hypertension. J Hypertens. 2014;32:2411–2421.
- Fung V, Huang J, Brand R, et al. Hypertension treatment in a medicare population: adherence and systolic blood pressure control. Clin Ther. 2007;29:972–984.
- Morris AB, Li J, Kroenke K, et al. Factors associated with drug adherence and blood pressure control in patients with hypertension. Pharmacotherapy. 2006;26:483–492.
- Christensen A, Osterberg LG, Hansen EH. Electronic monitoring of patient adherence to oral antihypertensive medical treatment: a systematic review. J Hypertens. 2009;27:1540–1551.