Abstract
Background: Management of resistant hypertension (RHTN) is challenging and often implies the use of complex polypharmacy and interventional therapies. The main objectives of this study were (i) to describe the characteristics of patients with RHTN referred to two expert centres; (ii) to identify predictors of blood pressure (BP) control after intensive management.
Methods: We reviewed electronic medical files of all patients referred for RHTN to the Brussels and Torino centres, and extracted detailed clinical data, informations on drug adherence and psychological profile. All patients with confirmed diagnosis of RHTN, according to office and ambulatory BP monitoring (ABPM) measurements, were considered eligible.
Results: 313 patients (51% men; age: 56 ± 12 years; office BP 177/98 mmHg; 24-hour ABPM 153/90 mmHg) were included. At the end of follow-up (median: 2 years [1–4]), only 26% of patients (n = 81) reached BP control. When compared to patients remaining resistant, patients eventually controlled had lower pulse pressure (71 vs. 82 mmHg, p < 0.001), less often myocardial infarction (6% vs. 20%, p < 0.005) and showed a higher recourse to cognitive reappraisal as far as emotion regulation is concerned (4.8 ± 1.1 vs. 3.9 ± 1.2, p = 0.009; ERQ Questionnaire). In a multivariate analysis looking for predictors of controlled BP, only the psychological characteristic of cognitive reappraisal (i.e., changing one’s thoughts about a potentially emotion-eliciting event) remained significant (OR 2.06 [1.10; 3.84], p = 0.02).
Conclusions: Even in expert centres, only a minority of patients with RHTN reached BP control, irrespective of the centre involved or the interventions applied. Patients who eventually responded to therapy had lower arterial stiffness and less cardiac organ damage. Furthermore, besides vascular damage, the single predictor of BP control was the ability to modify the emotional impact of stressful situations.
Introduction
Resistant hypertension (RHTN) is defined as office blood pressure (BP) values ≥140 and/or 90 mmHg despite 3 or more antihypertensive drugs at optimal or best-tolerated dosage, including a diuretic [Citation1–2]. According to the US definition, patients who require ≥4 antihypertensive drugs to reach BP control should also be considered resistant to treatment [Citation3].
The prevalence of RHTN ranges from 5 to 30% across different studies, according to the interpretations of the definition of RHTN used, and recent data suggested it has been increasing in the last years [Citation4]. However, prevalence of RHTN significantly decreases to 2.2% when only patients satisfying the strictest definition of RHTN (indicated above) are classified as resistant [Citation5–6].
Patients with RHTN have been shown to be at higher risk of hypertension-related organ damage, chronic kidney disease (CKD) and cardiovascular (CV) events [Citation7–8].
The diagnosis of RHTN requires confirmation of persistently high BP levels by out-of-office measurements, exclusion of causes of pseudoresistance (such as poor adherence to prescribed medications and clinician inertia) and screening for secondary causes of hypertension, which may benefit from specific treatment [Citation1].
Finally, management of RHTN is often challenging and implies identification and improvement of reversible lifestyle factors, discontinuation of interfering substances, maximization and optimization of antihypertensive therapy as well as treatment of comorbidities [Citation3].
During the last years, several interventional therapies, such as renal denervation (RDN) and baroreflex activation therapy (BAT), have been proposed to treat the most refractory cases with variable results [Citation9].
The aim of this retrospective study is to carefully depict the characteristics of a multicentre cohort of patients with a diagnosis of uncontrolled RHTN according to the definition of the ESH/ESC guidelines [Citation1] and to compare these characteristics across different subgroups (men vs. women, patients <60 years old vs. >60 years old, patients with RHTN who underwent RDN vs. patients who did not undergo RDN) in two expert centres of Northern and Southern Europe. Furthermore, we looked for baseline differences between patients who were eventually controlled vs. patients who remained refractory to therapy at the end of the follow-up and predictors of eventual BP control.
Methods
Inclusion criteria
Electronic medical files of all hypertensive outpatients referred to the Hypertension Clinique of the Cardiology Department of the Cliniques Universitaires Saint-Luc (Brussels, Belgium) and to the Hypertension Unit of the Division of Internal Medicine of the A.O.U. Città della Salute e della Scienza (Torino, Italy) were reviewed from 2010 to October 2018. Both Cliniques Universitaires Saint-Luc and A.O.U. Città della Salute e della Scienza are Excellence Centres of the European Society of Hypertension (ESH). The single inclusion criteria was essential uncontrolled RHTN; i.e. patients with office BP values ≥140 and/or 90 mmHg, and 24-hour ambulatory BP monitoring (ABPM) values ≥130 and/or 80 mmHg, despite the use of at least three antihypertensive drugs including a diuretic after careful exclusion of secondary causes of HTN. For patients with several visits, only the first one, according to which the patient met the criteria of resistant HTN, was considered for data analysis.
Details on clinical data extraction, methods of BP measurement and statistic tests may be found in the Online Data Supplement.
Adherence to drug therapy was assessed at baseline in a subsets of patients using a liquid chromatography system coupled with a tandem mass spectrometer as detector (LC-MS/MS) [Citation10–12]. Along adherence evaluation, four validated psychological questionnaires (The Toronto Alexithymia Scale – TAS-20 [Citation13], The Emotion Regulation Questionnaire – ERQ [Citation14], The Post Traumatic Diagnostic Scale – PTDS [Citation15], and The Brief Symptom Inventory – BSI [Citation16]) were administered in a subgroup of patients [Citation17], also at baseline. Further details on assessment of adherence and psychological tests are available in the Online Data Supplement.
Results
During the inclusion period, 313 patients out of 25 938 met the definition of RHTN (1.2%). The mean age at diagnosis was 56 ± 12 years, 51% were men and 89.1% Caucasians. Overall, subjects had an increased body max index (BMI 31 ± 6.7 kg/m2), 72 patients (23%) were current smokers at the moment of the first visit and 149 (48%) had a positive history for smoking.
Mean seated office systolic and diastolic BP values were 177 ± 26 mmHg and 98 ± 19 mmHg respectively, with a pulse pressure (PP) of 79 ± 24 mmHg. Standing office SBP and DBP were 176 ± 26 mmHg and 100 ± 20 mmHg, respectively. Twenty-four -hour ambulatory SBP was 153 ± 22 mmHg and 24-h ambulatory DBP was 90 ± 19 mmHg, with a PP of 64 ± 18 mmHg. Mean daytime ambulatory SBP and DBP were 158 ± 19 mmHg and 94 ± 16 mmHg, respectively, with a PP of 64 ± 16 mmHg and mean night-time ambulatory SBP and DBP were 144 ± 24 mmHg and 82 ± 19 mmHg, with a PP of 61 ± 15 mmHg. According to ABPM readings, 126 patients (40%) were non- or reverse dippers.
Approximately 63% patients were dyslipidaemic, 32% had type 2 diabetes and 23% had CKD. Fifty-one patients (16%) had a positive history of acute myocardial infarction, 14 (5%) suffered from heart failure, 17 (5%) from valvular disease and 130 patients (42%) had left ventricular hypertrophy (LVH). Among all comorbidities, Obstructive Sleep Apnoea Syndrome (OSAS) was the most frequent, affecting 85 (27%) patients, of whom 52 (17%) required continuous positive airway pressure (CPAP) therapy. All clinical and biochemical characteristics are shown in .
Table 1. Characteristics of patients with resistant hypertension at baseline.
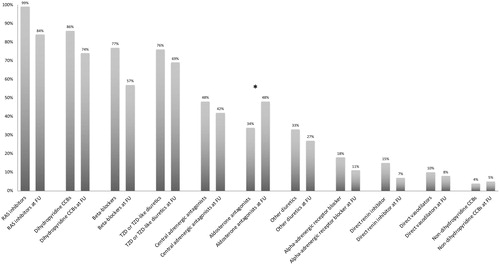
The median number of antihypertensive drug classes used at the diagnosis was 5 [4–6]. The proportion of patients on different antihypertensive drug classes at baseline is shown in . Notably, at the time of diagnosis, only 107 patients (34%) were under treatment with aldosterone antagonists.
Figure 1. Changes in antihypertensive drugs prescription from baseline to follow-up in the overall cohort of resistant hypertensive patients. *p-Value <0.001. RAS: Renin-Angiotensin-System; FU: Follow-up; CCBs: Calcium Channel Blockers; TZD: Thiazide diuretics.
Among non-antihypertensive medications, according to comorbidities, statins and other lipid lowering agents were prescribed in 43% and 10% respectively, oral antidiabetic agents and insulin in 23% and 10% respectively, and low dose acetylsalicylic acid in 40%. 69 patients (22%) were on antidepressant drugs and 73 subjects (21) underwent renal denervation.
Follow-up
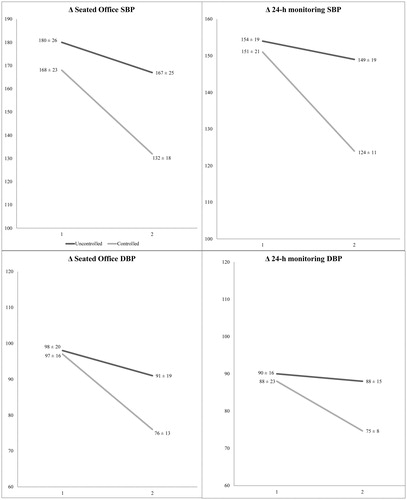
At the end of the follow-up (median 2 year [1–4]), seated Office SBP and DBP values decreased by −19 ± 29 mmHg and by −11 ± 17 mmHg, respectively (ΔPP −8 ± 21 mmHg). Twenty-four hour ambulatory SBP and DBP values decreased by −9 ± 23 mmHg and −6 ±14 mmHg (ΔPP −2 ± 16 mmHg), daytime ambulatory SBP and DBP reduced by −11 ± 24 mmHg and by −6 ± 14 mmHg (ΔPP −4 ± 14 mmHg), and nigh-time ambulatory SBP and DBP values decreased by −10 ± 24 mmHg and by −7 ± 15 (ΔPP −3 ± 13 mmHg), respectively.
Among patients who were still in follow-up (n = 127, 41%), the median number of antihypertensive drugs was 5 [4–6]. RAS inhibitors, dihydropyridine CCBs, thiazide or thiazide like diuretics and BB remained the most frequent antihypertensive classes prescribed (84%, 74%, 69%, 57%), while a pivotal increase in prescription of aldosterone antagonists was observed (48% vs. 34% at baseline, p < 0.001) ().
Patients with persistent RHTN vs. controlled RHTN at follow-up
At the end of the follow-up, 26% (81) were eventually controlled and 74% remained resistant to treatment. BP control was defined as OBP <140/90 mmHg and daytime ambulatory BP <135/85 mmHg.
Both median numbers of antihypertensive agents at diagnosis and at follow-up were lower in patients who reached BP control (5 [3–5] vs. 5 [4–6], p-value = 0.001 and 5 [4–6] vs. 5 [4–6], p-value = 0.02, respectively), while no significant differences in terms of prescribed antihypertensive drug classes were found (Table S1).
No differences in terms of age, sex, BMI, or comorbidities were found when patients with persistent RHTN (n = 232) at follow-up were compared with those who reached BP control (n = 81); only coronary artery disease was significantly more frequent in subjects with persistent RHTN at follow-up (acute myocardial infarction: 20% vs. 6%, p-value = 0.005). Both seated and standing Office SBP at diagnosis were significantly higher in patients with persistent RHTN (seated Office SBP: 180 vs. 168 mmHg, p-value = 0.001; standing Office SBP: 178 vs. 168 mmHg, p-value = 0.003, respectively), while no differences were detected either in terms of Office diastolic or ambulatory BP values (Table S1).
Analysis of PP values at baseline showed higher baseline PP values at Office and daytime ambulatory readings in patients who were still uncontrolled at the end of the follow-up when compared to patients who reached BP control (Seated Office PP: 82 vs. 71 mmHg, p-value = 0.001 – Standing Office PP 79 vs. 68 mmHg, p-value = 0.001 – Daytime ambulatory PP: 65 vs. 60 mmHg, p-value = 0.04). When comparing differences in terms of BP values from baseline to follow-up between the two subgroups, Office BP decreased two or three times more in patients who reached BP control (Δ Seated Office SBP/DBP: −36/−21 vs. −13/−7 mmHg, p-value <0.001/<0.001 – Δ Standing Office SBP/DBP: −39/−22 vs. −10/−6 mmHg, p-value <0.001/<0.001) and this difference was even more pronounced when considering ambulatory BP measurements (Δ Daytime ambulatory SBP/DBP: −31/−18 vs. −5/−3 mmHg, p-value <0.001/<0.001 – Δ Night-time ambulatory SBP/DBP: −29/−19 vs. −4/−3, p-value <0.001/<0.001 – Δ 24-h ambulatory SBP/DBP: −31/−18 vs. −4/−3 mmHg, p-value <0.001/<0.001) () (Table S1).
Figure 2. Office and ambulatory BP changes between baseline and follow-up in persistent resistant and controlled hypertensive at follow-up. SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure.
In univariate analysis, the single variables associated with controlled hypertension at follow-up were: Seated Office SBP at baseline (OR 0.98; IC 95% [0.97; 0.99], p-value = 0.009), Seated Office PP at baseline (OR 0.98; IC 95% [0.97; 0.99], p-value = 0.004), number of antihypertensive drugs at baseline (OR 0.74; IC 95% [0.62; 0.88], p-value = 0.001), history of myocardial infarction (OR 0.27; IC 95% [0.10; 0.73], p-value = 0.009), and “cognitive reappraisal” (known as the ability to change the way one thinks about a potentially emotion-eliciting event in order to modify its emotional impact) at the Emotion Regulation Questionnaire (ERQ) questionnaire (OR 1.95; IC 95% [1.11; 3.40], p-value = 0.019).
In multivariate analysis, the single independent predictor of eventual BP control after intensive management in the expert centre was psychological characteristic “cognitive reappraisal” (OR 2.06; IC 95% [1.10; 3.84], p-value = 0.02) ().
Table 2. Predictors of eventual blood pressure control at last follow-up in the expert centre.
Fully adherent subgroup of patients
Direct measurement of adherence by LC-MS/MS was available in a subgroup of 107 patients. Sixty-seven patients (63%) were fully adherent, 12 patients (11%) were partly adherent and 28 (26%) were non-adherent. The sixty-seven fully adherent patients were comparable to the overall cohort in terms of age, sex, comorbidities and major CV risk factors (Table S2). Fully adherent subjects had lower systolic and diastolic BP values at baseline (daytime ambulatory BP 149/88 vs. 160/95 mmHg, p-value <0.001/<0.005; for all the other BP measurements see Table S2) and were on a lower number of antihypertensive drugs (4 vs. 5, p-value =0.005). Despite a longer median follow-up (3 vs. 1.5 years, p-value <0.001), the proportion of patients reaching BP control at the end of the follow-up was similar to that of the overall population (30% vs. 25%; p-value = 0.3) (Table S2).
According to psychological evaluation, fully adherent patients were more likely to modify the emotional impact of stressful situations (“cognitive reappraisal” at ERQ test: 4.9 vs. 4.3, p-value = 0.027).
Finally, when performing the univariate analysis on the fully adherent subgroup, only the “cognitive reappraisal” characteristic (OR 1.95; IC 95% [1.11; 3.4], p-value = 0.019) was found to be a significant predictor of persistent uncontrolled hypertension at follow-up (Table S3).
Subgroup analysis
Comparison of characteristics of patients from Brussels vs. Torino, men vs. women, patients older or less than 60 years old and patients who underwent RDN or not, as well as the corresponding tables, are to be found in the Online Supplement.
Discussion
The main results of our study can be summarized as follows: (1) even in expert centres, only a small percentage of patients with resistant hypertension reached BP control at the end of the follow-up (around 26%), as well in the whole series as in patients fully adherent to antihypertensive regimen; (2) when compared with patients who remained resistant, patients who eventually reached BP control had lower office systolic BP at baseline, despite being on a lower number of antihypertensive drugs, had less stiff arteries as assessed by PP and less target organ damage; (3) in multivariate analysis, the single predictor of eventual BP control was the ability to modify the emotional impact of stressful situations, irrespective of the aforementioned factors; (4) while these conclusions hold true both in the whole series and in fully adherent patients, the latter were also characterized by a better ability to modify their own reaction to emotional stress.
First, our results underline the difficulty to reach BP control in patients with resistant hypertension, irrespective of the expert centre involved or the treatments used. In order to reach BP control in patients with RHTN, current guidelines recommend to implement diuretic treatment by increasing the existing diuretic dosage, or shifting to a more effective one (such as chlorthalidone or indapamide), and by adding as a fourth-line treatment a mineralocorticoid receptor antagonist (MRA) [Citation1–2]. In agreement with these recommendations, in our bi-centric cohort we documented a marked increase in the prescription of spironolactone from baseline to follow-up (from 34% to 48%, p-value <0.001). Though clearly insufficient, a proportion of ∼50% of patients on aldosterone antagonists is higher than that achieved in most resistant hypertension trials and registries [Citation18–21]. In a subset of patients characterized by particularly severe, refractory hypertension (21%), renal denervation was performed. Still, despite intensive attempts to improve BP treatment and use of exceptional therapies, three quarters of the patients remained uncontrolled at the end of follow-up.
Second, patients who remained resistant at the end of the follow-up had higher baseline Office and daytime ambulatory PP values when compared to patients who reached BP control. Overall, these data suggest that reaching BP control could be easier for patients with lower PP values, emphasising the role of arterial stiffness in sustaining resistant hypertension. Accordingly, PP evaluation, often ignored or disregarded, should be more often taken into account in order to predict therapeutic success and/or help selecting patients who could benefit more from specific therapeutic approaches, at least in resistant hypertensive population.
Another explanation to the low rate of BP control achieved may be the higher prevalence of CV complications, particularly of previous myocardial infarction, among those patients who remained uncontrolled at the end of the follow-up. If on one hand, it is well known that patients with resistant hypertension have an increased risk of target organ damage (TOD) and CV complications [Citation1,Citation7], on the other hand, the relations between TOD, CV comorbidities and resistant hypertension can also be bidirectional. Indeed the presence of LVH, aortic stiffness, CKD and/or of other CV structural and functional alterations may contribute, to the maintenance of resistant hypertension. Therefore, therapeutic strategies aiming to reduce TOD should be considered as crucial as antihypertensive medications to increase the probability to reach BP control and improve patient prognosis [Citation22].
Third, ability to modify the emotional impact of stressful situations was associated with a better adherence to antihypertensive drug treatment and, irrespective of adherence, was the single independent predictor of eventual BP control. Along the same lines, in patients with refractory hypertension referred to our centre, poor adherence correlated with a tendency to suppress expression of emotions and an increased difficulty to describe feelings [Citation17]. Besides recent hospital admission for hypertension, the best predictors of poor drug adherence were the lack of recourse to the strategy of putting things in perspective in stressful situations and the level of somatization, while truly resistant patients were characterized by self- and other-blame as well as avoidance and emotional blunting [Citation17]. In many cases these psychological characteristics may reflect maladaptation to previous traumatic events and subsequent post traumatic stress disorder (PTSD) [Citation17,Citation23–25]. Notably, both in the previous and in the current study, no other basic clinical or demographic characteristics allowed predicting either drug resistance, drug adherence [Citation17] or eventual BP control after intensive management in patients with RHTN.
This study has limitations. The first limitation is the retrospective nature of the study. In order to limit the risk of bias, we systematically collected detailed information from all patients, providing an accurate description of their general characteristics and ambulatory monitoring BP values for all participants. Furthermore, our cohort incorporated patients from Brussels and Torino Excellence Centres and, as such, is likely representative for both Northern and Southern Europe. Second, adherence evaluation through therapeutic drug monitoring was only available for a subgroup of patients (111 out of 313 patients). Still, our results (especially the general characteristics at baseline and at follow-up, the rate of hypertension control and the influence of psychological characteristics on BP control) were similar in the overall population (n = 313) and in the subgroup of patients who were fully adherent to antihypertensive regimen (n = 67). Finally, our results may not be readily extrapolated to patients with milder form of RHTN, seen in less specialized settings.
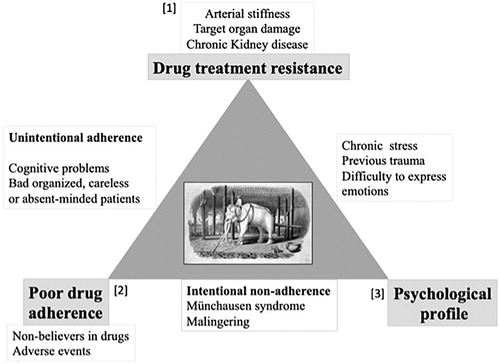
In conclusion, our study further contributes to build evidence on the importance of psychological factors, particularly the ability to adjust expression of emotion in stressful situations in the pathophysiology and response to treatment of severe, resistant forms of hypertension. Overall, our findings [Citation17] add further support to the recommendation to assess psychological profile in patients with drug resistant hypertension before considering complex, potentially dangerous regimens or interventional therapies [Citation26]. Further studies should aim at evaluating the efficacy of psychological interventions to improve BP control in patients with refractory hypertension. More mechanistic studies incorporating hormonal dosages, functional magnetic resonance [Citation27] and/or PET-CT [Citation28] would also be of interest. It is definitely time to widen our perspective [Citation24] and incorporate psychological aspects in our understanding of the pathophysiology of RHTN (see tentative model in ).
Figure 3. Hypothetical model of the interactions between drug adherence, psychological profile and target organ damage in the pathogenesis of resistant hypertension.
Target organ damage, poor drug adherence and previous traumatic experiences/altered psychological profiles are the cornerstones of resistant hypertension, the “white elephant” in the field. They may be involved either separately or jointly. A few possible scenarios include: (i) poor drug adherence (2) may lead to TOD (1), which increases drug resistance even when drug adherence is afterwards improved; (ii) in hypertensive patients with increased arterial stiffness and/or TOD (1), reaching BP control may be difficult, inducing them to stop medications because of discouragement (2); (iii) altered psychological profiles (3) may be responsible for intentional (i.e. Münchausen syndrome) poor adherence (2), leading to an increased risk of TOD and finally of RHTN (1); (iv) or induce neuro-hormonal or inflammatory changes eventually leading to RHTN (1), irrespective of drug adherence.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Supplemental Material
Download MS Word (106.6 KB)Disclosure statement
The authors report no conflict of interest
References
- Williams B, Mancia G, Spiering W, et al. 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC Task Force for the management of arterial hypertension. J Hypertens. 2018;36:2284–2309.
- Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017;71:2199–2269.
- Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension 2008;51:1403–1419.
- Egan BM, Zhao Y, Axon RN, et al. Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation 2011;124:1046–1058.
- Weitzman D, Chodick G, Shalev V, et al. Prevalence and factors associated with resistant hypertension in a large health maintenance organization in Israel. Hypertension 2014;64:501–507.
- Hayek SS, Abdou MH, Demoss BD, et al. Prevalence of resistant hypertension and eligibility for catheter-based renal denervation in hypertensive outpatients. Am J of Hypertens. 2013;26:1452–1458.
- Daugherty SL, Powers JD, Magid DJ, et al. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation 2012;125:1635–1642.
- de la Sierra A, Banegas JR, Oliveras A, et al. Clinical differences between resistant hypertensives and patients treated and controlled with three or less drugs. J Hypertens. 2012;30:1211–1216.
- Lobo MD, Sobotka PA, Pathak A. Interventional procedures and future drug therapy for hypertension. Eur Heart J. 2017; 38:1101–1111.
- Wunder C, Persu A, Lengelé JP, et al. Adherence to antihypertensive drug treatment in patients with apparently treatment-resistant hypertension in the INSPIRED pilot study. Blood Press. 2019;28(3):168–172.
- De Nicolò A, Avataneo V, Rabbia F, et al. UHPLC-MS/MS method with protein precipitation extraction for the simultaneous quantification of ten antihypertensive drugs in human plasma from resistant hypertensive patients. J Pharm Biomed Anal. 2016;129:535–541.
- De Nicolò A, Avataneo V, Rabbia F, et al. UHPLC-MS/MS method with sample diluition to test therapeutic adherence through quantification of ten antihypertensive drugs in urine samples. J Pharm Biomed Anal. 2017;142:279–285.
- Bagby RM, Parker JDA, Taylor GJ. The twenty-item Toronto Alexithymia scale-I. Item selection and cross-validation of the factor structure. J Psychosom Res. 1994;38:23–32.
- Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85:348–362.
- Foa EB, Cashman L, Jaycox L, et al. The validation of a self-report measure of posttraumatic stress disorder: the Posttraumatic Diagnostic Scale. Psychol Assess. 1997;9:445–451.
- Derogatis LR. Brief Symptom Inventory: BSI; administration, scoring, and procedures manual. Minneapolis (MN): Pearson; 1993.
- Petit G, Berra E, Georges CMG, et al. Impact of psychological profile on drug adherence and drug resistance in patients with apparently treatment-resistant hypertension. Blood Press. 2018;27:358–367.
- de Jager RL, de Beus E, Beeftink MM, et al. Impact of medication adherence on the effect of renal denervation: the SYMPATHY trial. Hypertension 2017;60:678–684.
- Bhatt DL, Kandzari DE, O’Neill WW, et. al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014;370:1393–1401.
- Böhm M, Mahfoud F, Ukena C, et al. First report of the Global SYMPLICITY Registry on the effect of renal artery denervation in patients with uncontrolled hypertension. Hypertension 2015;65:766–774.
- Rosa J, Widimský P, Toušek P, et al. Randomized comparison of renal denervation versus intensified pharmacotherapy including spironolactone in true-resistant hypertension: six-month results from the Prague-15 study. Hypertension. 2015;65:407–413.
- Muiesan ML, Salvetti M, Rizzoni D, et al. Resistant hypertension and target organ damage. Hypertens Res. 2013;36:485–491.
- Howard JT, Sosnov JA, Janak JC, et al. Associations of initial injury severity and posttraumatic stress disorder diagnoses with long-term hypertension risk after combat injury. Hypertension. 2018;71:824–832.
- Persu A, Petit G, Georges C, et al. Hypertension, a posttraumatic stress disorder? Time to widen our perspective. Hypertension. 2018;71:811–812.
- Frans O, Rimmö PA, Aberg L, et al. Trauma exposure and post-traumatic stress disorder in the general population. Acta Psychiatr Scand. 2005;111:291–299.
- Berra E, Azizi M, Capron A, et al. Evaluation of adherence should become an integral part of assessment of patients with apparently treatment-resistant hypertension. Hypertension. 2016;68:297–306.
- Naumczyk P, Sabisz A, Witkowska M, et al. Compensatory functional reorganization may precede hypertension-related brain damage and cognitive decline: a functional magnetic resonance imaging study. J Hypertens. 2017;35:1252–1262.
- Tawakol A, Ishai A, Takx RA, et al. Relation between resting amygdalar activity and cardiovascular events: a longitudinal and cohort study. Lancet 2017;389:834–845.
