Abstract
Background: Childhood obesity, including overweight, continues increasing worldwide affecting health expectancy, quality of life and healthcare expenditure. These subjects have higher probability of suffering or developing cardio metabolic risk factors. Recent studies have revealed cardiorespiratory fitness (CRF) as a valuable clinical parameter to identify these subjects and have even suggested cut-off values. However, evaluating CRF in overweight and obese youth can be difficult to implement, unfriendly and expensive.
Objective: Develop a screening tool to identify high-risk subjects in a representative population of those attending overweight/obesity assessment programmes without prior intervention. It will be based on heart rate variability parameters, which has strong association with CRF and cardio metabolic risk factors.
Methods: Sixty-three subjects, overweight and obese, between 9 and 17 years of age, and of both sexes were enrolled. None of them had secondary obesity syndromes and/or suffered from acute or chronic disease. Anthropometric parameters, electrocardiogram signal recording under resting conditions and cardiorespiratory fitness – evaluated by oxygen consumption and time elapsed of cardiopulmonary exercise test – were measured.
Results: Significant differences in the sympathetic nervous system activity – assessed by heart rate variability analysis – are observed when grouping by overweight and obesity degree as well as by CRF (poor/normal). Body mass index, puberty and sympathetic nervous system activity are the significant variables of a logistic regression model develop to identify poor CRF individuals. Its accuracy reaches 92%.
Conclusions: A screening tool based on heart rate variability and anthropometric parameters was developed to identify subjects with higher probability of suffering or developing cardio metabolic risk factors.
Introduction
Over the last decades the prevalence of obesity in children and adolescents has increased worldwide [Citation1,Citation2] affecting health expectancy, quality of life and healthcare expenditures. Most of the implemented interventions are based on adopting healthier lifestyle habits focussing on an increase in physical activity and/or on nutritional aspects.
Improving health outcomes is directly related with a high degree of customization to enhance both the subject’s and their family’s motivation. In this context, variables such as cardiorespiratory fitness (CRF), normally assessed by oxygen consumption while performing a normalized exercise protocol, are relevant not only to design and implement personalized clinical strategies based on promoting physical activity but also contributes to identify subjects at higher risk of suffering or developing cardio metabolic and cardiovascular risk factors [Citation3,Citation4].
While there is agreement in the fact that a cardiopulmonary exercise test (CPET) can be considered as the gold standard to assess CRF in youth and the relevance of such a parameter, there are strong limitations for its implementation outside specific clinical departments. In addition, there is still controversy regarding which is the most appropriate stopping criterion and which parameters are the most meaningful [Citation5–11]. For example, for risk classification, the VO2max variable must be accurately measured by performing a CPET test to exhaustion and/or till the oxygen consumption plateau is reached. However, the overweight/obese population rarely reach such plateau and ethical issues might arise regarding the performance of this unfriendly procedure in the target population.
To overcome these limitations empirical and theoretical equations as well as outdoor protocols have been developed in the recent past [Citation12,Citation13]. Unfortunately, the results obtained by these means are in most cases cohort and protocol dependent, causing an increase in the heterogeneity of the values and making it more difficult to compare the findings of different studies [Citation13].
Heart rate variability (HRV), from an electrocardiogram (ECG) signal obtained under resting conditions, has shown to have a strong relationship with CRF and with intermediate mechanisms involved in developing cardio metabolic abnormalities in obese adults and youths [Citation4,Citation14–18], even though in this latter one, the number of studies is scarce [Citation19]. Even though evaluating HRV is not exempt of complexities, it is by far easier to perform, less expensive and easier to implement than the cardiopulmonary exercise test procedure [Citation20].
In this context, the main objective of the present research is to study the feasibility of developing a screening tool to identify poor CRF subjects in a representative population of those attending overweight/obesity assessment programmes without prior intervention. This tool will be based on heart rate variability parameters and should be easily applicable in a clinical context.
Methods
A total of 63 subjects, overweight and obese, between the ages of 9 and 17, and of both sexes, who underwent an assessment of overweight/obesity in the Paediatric Department of the Consorcio Hospital General de Valencia (Spain), were enrolled in this research study, which was approved by the Ethical Committee of the Consorcio Hospital General de Valencia, as well as by the parents and participants being 12 years or older. None of the subjects involved had secondary obesity syndromes and/or suffered from acute or chronic disease.
Anthropometric parameters, BP measurements, electrocardiogram signal recording in resting conditions and CRF, evaluated by VO2peak and time elapsed of cardiopulmonary exercise test, were measured in all subjects.
Anthropometrics
Body weight and height were measured using a standard beam balance scale and a standardized wall-mounted height board. In both cases, the subjects were wearing light indoor clothing and no shoes. Overweight, moderate and severe obesity were classified in this research paper according to the extended international body mass index (BMI) cut-offs [Citation21]. This classification is exclusively for children and is not linked to the corresponding adult BMI values.
Recording electrocardiogram in resting conditions and calculating heart rate variability
The electrocardiogram signal was continuously measured and recorded using a TIPS shirt for a 15-minute period while the subject was in fasting conditions and lying down in a quiet room at 23 °C temperature [Citation22,Citation23].
Heart rate variability parameters were calculated from the recorded ECG signal. Linear parameters in the time and frequency domains as well as non-linear dynamics were analysed:
Standard deviation of the NN interval series (SDNN),
Percentage of consecutive NN intervals that differed by more than 50 ms (pNN50).
Power density corresponding to low frequency (LF: 0.04–0.15) and high frequency (HF: 0.15–1) using the Lomb–Scargle method [Citation24].
Poincare’s plot to determine short (SD1) and long term (SD2) variation.
Entropy based measures (sampEn).
And Fractal based measures using the Detrended Fluctuation Analyses method to determine short (α1) and long (α2) term variation.
Evaluating cardiorespiratory fitness through oxygen consumption in effort conditions
The CRF of all subjects was evaluated by measuring the oxygen consumption (VO2) with an indirect calorimeter [Citation25], while performing a cardio pulmonary exercise test (CPET). Normalized effort conditions were established according to a modified version of the Balke protocol for treadmills [Citation26]. Despite the modifications performed in speed, slope and stopping criterion to assure a more secure environment the procedure still retains its discriminatory effect. Once the stopping criterion was reached, the oxygen consumption (VO2peak) and the elapsed time (teff) were recorded. In case VO2max was not reached it was calculated according to the Wasserman equation [Citation27], one of the recommended by the American Thoracic Society/American College of Chest Physicians (ATS/ACCP), and by far the most implemented in cardiopulmonary exercise test equipment.
Statistical analysis
The data obtained from each of the participants were statistically analysed using the SPSS version 16 (SPSS Inc., Chicago, IL, USA). To confirm the cohort’s normal distribution, the Shapiro–Wilk and normal Q-Q plots analyses were performed. One-way ANOVA was used to compare quantitative variables, followed by Bonferroni test to control for multiple comparisons. Logistic regression analysis was performed to develop the mathematical predictive models capable of identifying potential individuals with low CRF. The accuracy of the model was tested using the ROC curve analysis. In all cases, p-values lower than 0.05 were considered statistically significant. Cross-validation was performed using the R Studio software, version 3.5.1, by applying the k-fold method included in the Caret library. In this case, k was equal to 10.
Results
Cohort classified according to obesity degree
The general characteristics of the studied population, grouped by overweight and degree of obesity, are summarized in . Significant differences between moderate and severe obese with overweight subjects were observed regarding anthropometrics variables (weight: p < 0.000, height: p < 0.016, fat percentage: p < 0.001, waist: p < 0.001, BMI: p < 0.000 and BMI zScore: p < 0.000) and CRF (VO2peak: p < 0.000). In addition, significant differences in time elapsed (teff: p < 0.000) were present between the severe and the moderate obese with the overweight group. Regarding HRV parameters, only aHF (ms2) (p < 0.038) presented significant differences between the obese groups.
Table 1. General characteristics of the studied cohort classified according to obesity degree following the IOTF criteria.
Cohort classified according to cardiovascular disease risk assessed by VO2max
The general features of the groups classified according to the CRF level (e.g. poor or normal) are listed in . Poor CRF corresponds to VO2max ≤ 41.8 mlO2 kg−1min−1 and VO2max ≤ 34.6 mlO2 kg−1min−1 for males and females, respectively [Citation3]. These subjects have a higher probability of suffering or developing cardiovascular and/cardio metabolic risk factors than those with normal CRF. Despite the heterogeneity of both groups, poor CRF is mainly made up of post-pubertal and severe obese individuals in comparison with normal CRF, which consists of pre-pubertal and overweight individuals. Moreover, gender distribution considerably varies from one group to the other. For example, 47% of the subjects with poor CRF are females in contrast with 27% in the normal CRF group.
Table 2. General characteristics of the cohort when classified as poor or normal CRF – evaluated by VO2max calculated with the Wasserman equation – using the cut-off values of 41.8 and 34.6 mlO2/kg−1 min−1 for boys and girls, respectively.
Significant differences regarding BMI, weight, teff, VO2peak/VO2max are present. BMI (p < 0.000) and weight (p < 0.005) decrease from poor CRF to normal CRF while teff (p < 0.045), VO2max (p < 0.000) and VO2peak/VO2max (p < 0.000) increases. It is also interesting to point out that those subjects with poor CRF reach VO2peak values closer to VO2max during cardiopulmonary exercise tests in comparison with their normal CRF peers.
Also, significant differences are observed with respect to heart rate variability parameters (aHF (ms2): p < 0.001; aTotal (ms2): p < 0.001; nLF (n.u): p < 0.01; nHF (n.u): p < 0.01).
Logistic regression model
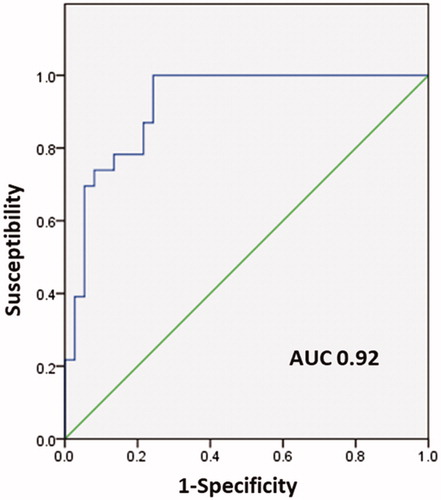
A logistic regression model was developed to identify subjects attending overweight/obesity assessment with poor CRF by making use of the aforementioned cut-off values. The Forward Wald procedure showed BMI (p < 0.005), height (p < 0.019), nLF (n.u) (p < 0.009) and puberty stage (p < 0.002) as significant covariates (). The area under the curve (AUC) from the ROC curve analysis, illustrated in , reveal an accuracy of 92%.
Table 3. Logistic regression model to identify subjects with poor CRF – evaluated by VO2max calculated with the Wasserman equation – according to the cut-off values 41.8 and 34.6 mlO2/min kg for boys and girls, respectively.
The k-fold method, with k equal to 10, was used to study the reproducibility of the model. The results are summarized in . The model not only has a high reproducibility (Sensitivity of 95% and Specificity of 50%) but also a high capability to minimize false negatives (Recall 95%). This is especially relevant when considering that the prevalence of poor CRF in the studied cohort is only of the 22%. Consequently, the model contributes to identify these subjects which could be, in the future, at higher risk of developing cardiometabolic risk factors according to the CRF threshold values used in the present study.
Table 4. Summary of the performance parameters yield by applying the k-fold method using R studio, version 3.5.1, to test the reproducibility of the developed logistic regression model.
Discussion
The main finding of the present study performed on youth attending overweight/obesity clinical assessment is that significant differences in heart rate variability parameters, calculated under resting conditions, are observed between subjects with poor and normal CRF levels independently of their obesity degree, pubertal stage and age. This allows clinicians to develop an easily implementable screening tool to identify subjects with poor CRF without undergoing a cardiopulmonary exercise test, which is expensive and highly disturbing. These subjects are well known to have a higher probability of developing cardiovascular and/or cardio metabolic risk factors than their fitter or more physically active peers [Citation3,Citation4].
Since the recent past, CRF, evaluated through oxygen consumption, has gained relevance due to its predictive capability of morbidity and mortality in the adult population. Scientific associations like the American Heart Association (AHA) [Citation28] have recently recommended its evaluation in the daily clinical routine. This increase in interest is also plausible in children and adolescents due to several studies that have identified reference values for healthy and unhealthy subjects [Citation3,Citation29,Citation30] as well as strong associations with cardiometabolic and cardiovascular risk factors [Citation4,Citation26].
The inverse relationship between CRF and obesity is evident in the studied cohort when grouping according to obesity degree () or by CRF condition (), considering the cut-off values of VO2max ≤ 41.8 mlO2 kg−1min−1 and VO2max ≤ 34.6 mlO2 kg−1min−1 for males and females, respectively [Citation3]. On one hand, as obesity degree increases, VO2peak, teff and VO2max diminish, even though only the first two show significant differences. On the other hand, the poor CRF group presents significantly higher weight and BMI values in comparison with normal CRF peers.
In contrast with the cardiopulmonary exercise test, the study and analysis of HRV has become a very popular tool due to its simplicity and low cost. However, its employment in the paediatric population has been scarce, even though it has been applied in several fields, such as cardio metabolic, cardiovascular disease and CRF [Citation3,Citation4,Citation19]. Despite there being no total consensus regarding the impact of metabolic risk factors and physical activity on HRV parameters in obese youth, it seems to be accepted that the overall activity of the Autonomic Nervous System (ANS), evaluated as the sum of power in High (0.15–1) and Low (0.04–0.15) frequency bands, is related with higher performance of physical activity and inversely with body weight. Moreover, an activity increase in the Sympathetic Nervous System, measured by the power in the low frequency bands, is associated with some metabolic risk factors, such as hyperglycaemia and hypertension [Citation4,Citation31–38]. These relationships are not evident by looking at and , even though significant differences in the frequency domain parameters are observed between groups. This can be explained by the fact that none of the subjects included in the studied suffered from hyperglycaemia or hypertension. However, it is also well known that age, puberty, gender, breathing rate and even obesity duration can modify HRV [Citation38].
A logistic regression model taking into consideration the potential impact of the aforementioned parameters, except obesity duration, was performed. The main reason was because these subjects had no prior intervention and were attending for the first time the overweight/obesity clinical assessment programme at the Paediatric Department of Consorcio Hospital General Universitario de Valencia. The model revealed BMI, height, puberty and nLF as significant variables (). According to the ROC curve analysis the model is capable of identifying these high-risk subjects with 92% accuracy according to the ROC curve analysis illustrated in . In addition, it shows a high reproducibility (Specificity 95% and Sensitivity 50%) and a high capability to minimize false negatives (Recall 95%) (). Both features suggest its applicability for clinical decision taking because it is capable of accurately identifying subjects which could be, in the future, at higher risk of developing cardio-metabolic or cardiovascular risk factors and therefore might require a closer clinical follow up to prevent a health deterioration.
The fact that puberty is significant highlights its contribution in modifying heart rate variability parameters [Citation38] and can help to explain the lack of clear trends regarding these parameters in and . In the case of nLF it seems to corroborate the strong association between obesity and cardio metabolic and cardiovascular risk factors with a higher activity of the sympathetic nervous system [Citation4,Citation31–38].
The model can help physicians to identify subjects with poor CRF without the need of performing a CPET test, which is expensive and disturbing, and popularizing CRF as a clinical parameter worthy of routine measurement, in agreement with the recommendations of the American Heart Association [Citation28].
Regardless of the results it is worth mentioning that this is a cross-sectional study with a limited sample size that does not allow establishing casual relationships among the tested parameters. Moreover, the findings are not representative of the general population because the main target was overweight and obese youth attending a clinical assessment programme without prior intervention. These subjects are expected to have a higher probability to suffer or develop cardio metabolic and/or cardiovascular risk factors than their normal weight peers. Unfortunately, no information was available regarding the duration of overweight/obesity, a factor that could influence the ANS activity, neither the amount of physical activity performed outside school.
Conclusions
A logistic regression model based on anthropometric and heart rate variability parameters, calculated from the ECG signal under resting conditions, has demonstrated its usefulness to identify subjects with poor CRF without the need to perform a cardiopulmonary exercise test, which is expensive and disturbing. These subjects can require in a near future a closer supervision to prevent the development of cardiovascular and cardio metabolic risk factors.
Author contributions
PR carried out the heart rate variability analysis and the statistical analyses. It also helped in the coordination of the technical part (i.e. signal acquisition) of the project. JP carried out the cardiopulmonary exercise tests where maximum oxygen consumption was evaluated. GG contributed in the process of interpreting heart rate variability analysis from a clinical point of view and determining potential applications. GG, JR and EL participated in the design and coordination of the project. All authors were involved in writing the paper and had a final approval of the submitted versions.
Disclosure statement
The authors declare no conflicts of interest. They also declare no conflicts from outside the present work.
Additional information
Funding
References
- WHO. Prevention and control of non-communicable diseases. Report of the Secretary-General. United Nations General Assembly A/66/83. 2011 May 19 [cited 2013 Dec 9]. Available from: http://www.un.org/ga/search/view_doc.asp?symbol=A/66/83&Lang=E
- World Health Organization. Global status report on noncommunicable diseases. 2014 [cited 2015 Nov 10]. Available from: http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf
- Ruiz JR, Cavero-Redondo I, Ortega FB, et al. Cardiorespiratory fitness cut points to avoid cardiovascular disease risk in children and adolescents; what level of fitness should raise a red flag? A systematic review and meta-analysis. Br J Sports Med. 2016;50:1451–1458.
- Redón P, Grassi G, Redon J, et al. Sympathetic neural activity, metabolic parameters and cardiorespiratory fitness in obese youths. J Hypertens. 2017;35:571–577.
- Pianosi PT, Liem RI, McMurray RG, et al. Pediatric exercise testing: value and implications of peak oxygen uptake. Children (Basel). 2017;4:E6.
- Barker AR, Williams CA, Jones AM, et al. Establishing maximal oxygen uptake in young people during a ramp cycle test to exhaustion. Br J Sports Med. 2011;45:498–503.
- Astrand P, Rodahl K. Textbook of work physiology: physiological bases of exercise. 3rd ed. New York: McGraw-Hill; 1986.
- Rowland TW, Cunningham LN. Oxygen uptake plateau during maximal treadmill exercise in children. Chest. 1992;101:485–489.
- Hebestreit H, Staschen B, Hebestreit A. Ventilatory threshold: a useful method to determine aerobic fitness in children? Med Sci Sports Exerc. 2000;32:1964–1969.
- Yeh MP, Gardner RM, Adams TD, et al. “Anaerobic threshold”: problems of determination and validation. J Appl Physiol Respir Environ Exerc Physiol. 1983;55:1178–1186.
- Weisman IM, Zeballos RJ. A step approach to the evaluation of unexplained dyspnea: the role of cardiopulmonary exercise testing. Pulm Perspect. 1998;15:8–11.
- Sartor F, Vernillo G, de Morree HM, et al. Estimation of maximal oxygen uptake via submaximal exercise testing in sports, clinical and home settings. Sports Med. 2013;43:865–873.
- Evans HJ, Ferrar KE, Smith AE, et al. A systematic review of methods to predict maximal oxygen uptake from submaximal, open circuit spirometry in healthy adults. J Sci Med Sport. 2015;18:183–188.
- Malpas SC. Sympathetic nervous system overactivity and its role in the development of cardiovascular disease. Physiol Rev. 2010;90:513–557.
- Baum P, Petroff D, Classen J, et al. Dysfunction of autonomic nervous system in childhood obesity: a cross-sectional study. PLoS One. 2013;8:e54546.
- Thorp AA, Schlaich MP. Relevance of sympathetic nervous system activation in obesity and metabolic syndrome. J Diabetes Res. 2015;2015:1.
- Kotsis V, Nilsson P, Grassi G, et al. WG on obesity, diabetes, the high risk patient, European Society of Hypertension. New developments in the pathogenesis of obesity-induced hypertension. J Hypertens. 2015;33:1499–1508.
- Grassi G, Seravalle G, Dell'oro R. Sympathetic activation in obesity: a noninnocent bystander. Hypertension. 2010;56:338–340.
- Da Silva DF, Bianchini JA, Antonini VD, et al. Parasympathetic cardiac activity is associated with cardiorespiratory fitness in overweight and obese adolescents. Pediatr Cardiol. 2014;35:684–690.
- Sassi R, Cerutti S, Lombardi F, et al. Advances in heart rate variability signal analysis: joint position statement by the e-Cardiology ESC Working Group and the European Heart Rhythm Association co-endorsed by the Asia Pacific Heart Rhythm Society. Europace. 2015;17:1341–1353.
- Cole TJ, Bellizzi MC, Flegal KM, et al. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–1243.
- Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J. 1996;17:354–381.
- Compher C, Frankenfield D, Keim N, et al.; Evidence Analysis Working Group. Best practice methods to apply to measurement of resting metabolic rate in adults: a systematic review. J Am Diet Assoc. 2006;106:881–903.
- Clifford GD, Azuaje F, McSharry PE. Advanced methods and tools for ECG data analysis. Boston (MA): Artech House Publishing; 2006.
- Wahrlich V, Anjos LA, Going SB, et al. Validation of the VO2000 calorimeter for measuring resting metabolic rate. Clin Nutr. 2006;25:687–692.
- Guixeres J, Redon P, Saiz J, et al. Cardiovascular fitness in youth: association with obesity and metabolic abnormalities. Nutr Hosp. 2014;29:1290–1297.
- Wasserman K, Hansen JE, Sue DY, et al. Principles of exercise testing and interpretation: including pathophysiology and clinical applications. 3rd ed. Philadelphia (PA): Lippincott, Williams &Wilkins; 1999.
- Ross R, Blair SN, Arena R, et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016;134:e653–e699.
- Ortega FB, Artero EG, Ruiz JR, et al. Physical fitness levels among European adolescents: the HELENA study. Br J Sports Med. 2011;45:20–29.
- Eisenmann JC, Laurson KR, Welk GJ. Aerobic fitness percentiles for U.S. adolescents. Am J Prev Med. 2011;41:S106–S110.
- Brands MW, Hildebrandt DA, Mizelle HL, et al. Sustained hyperinsulinemia increases arterial pressure in conscious rats. Am J Physiol. 1991;260:R764–R768.
- Berne C, Fagius J, Pollare T, et al. The sympathetic response toeuglycaemic hyperinsulinaemia. Evidence from microelectrode nerve recordings in healthy subjects. Diabetologia. 1992;35:873–879.
- Lembo G, Napoli R, Capaldo B, et al. Abnormal sympathetic overactivity evoked by insulin in the skeletal muscle of patients with essential hypertension. J Clin Invest. 1992;90:24–29.
- Guarino D, Nannipieri M, Iervasi G, et al. The role of the autonomic nervous system in the pathophysiology of obesity. Front Physiol. 2017;8:665.
- Canale MP, Manca di Villahermosa S, Martino G, et al. Obesity-related metabolic syndrome: mechanisms of sympathetic overactivity. Int J Endocrinol. 2013;2013:1.
- Smith MM, Minson CT. Obesity and adipokines: effects on sympathetic overactivity. J Physiol. 2012;590:1787–1801.
- Grassi G, Mark A, Esler M. The sympathetic nervous system alterations in human hypertension. Circ Res. 2015;116:976–990.
- Oliveira RS, Barker AR, Wilkinson KM, et al. Is cardiac autonomic function associated with cardiorespiratory fitness and physical activity in children and adolescents? A systematic review of cross-sectional studies. Int J Cardiol. 2017;236:113–122.