Abstract
Background
The Covid-19 pandemic necessitated a decrease in non-Covid-19 related diagnostic and therapeutic procedures in many countries. We explored the impact on tertiary hypertension care.
Methods
We conducted an electronic survey regarding 6 key procedures in hypertension care within the Excellence Center network of the European Society of Hypertension.
Results
Overall, 54 Excellence Centers from 18 European and 3 non-European countries participated. From 2019 to 2020, there were significant decreases in the median number per centre of ambulatory blood pressure monitorings (ABPM: 544/289 for 2019/2020), duplex ultrasound of renal arteries (Duplex RA: 88.5/55), computed tomographic/magnetic resonance imaging angiography of renal arteries (CT/MRI RA: 66/19.5), percutaneous angioplasties of renal arteries (PTA RA: 5/1), laboratory tests for catecholamines (116/67.5) and for renin/aldosterone (146/83.5) (p < 0.001 for all comparisons, respectively). While reductions in all assessed diagnostic and therapeutic procedures were observed in all annual 3-months periods in the comparisons between 2019 and 2020, the most pronounced reduction occurred between April and June 2020, which was the period of the first wave and the first lockdown in most affected countries. In this period, the median reductions in 2020, as compared to 2019, were 50.7% (ABPM), 47.1% (Duplex RA), 50% (CT/MRI RA), 57.1% (PTA RA), 46.9% (catecholamines) and 41.0% (renin/aldosterone), respectively. Overall differences in reduction between 3-month time intervals were statistically highly significant.
Conclusion
Diagnostic and therapeutic procedures related to hypertension were dramatically reduced during the first year of the Covid-19 pandemic, with the largest reduction during the first lockdown. The long-term consequences regarding blood pressure control and, ultimately, cardiovascular events remain to be investigated.
Introduction
The unprecedented ongoing global Corona-virus disease 2019 (Covid-19) pandemic undoubtedly has a dramatic influence on many, if not almost all, aspects of daily life. Lifestyle, psychological, socioeconomic and environmental factors have changed profoundly during and in reaction to the pandemic [Citation1,Citation2]. The impact of the Covid-19 pandemic on healthcare was particularly strong. Out of the blue, Covid-19 emerged as the third leading cause of death in the United States in 2020 [Citation3]. The Covid-19 pandemic obviously necessitated healthcare systems globally to focus on its rapid, demanding and persistent management. Consequently, healthcare resources for other diseases had to be redirected to Covid-19 care. This led to a substantial reduction of care for acute non-Covid-19 diseases, but even more for a wide range of chronic diseases. For instance, endoscopies in general [Citation4] and particularly for cancer screening [Citation5] including colorectal cancer service [Citation6], elective urological procedures [Citation7], elective non-urgent orthopaedic operations [Citation8–10], and the access to diabetes education and multidisciplinary care [Citation11] were reduced. In cardiovascular medicine, during the first month of the lockdown in 2020, there have been dramatic reductions in face-to-face clinical meetings in heart failure services and cardiac rehabilitations of up to 100% [Citation12], but also of chest pain, acute coronary syndromes [Citation13] and heart failure admissions as well as emergency department attendance of 50% and more [Citation12–14]. Cardiovascular procedures, such as percutaneous coronary interventions, cardiac pacemaker implantations, coronary artery bypass graft surgery, carotid artery endarterectomy/stenting, cerebral aneurysm coiling, aortic aneurysm repair and limb revascularizations have been reduced by 50–90% [Citation14]. Diagnostic tests for cardiovascular diseases were reduced by 42% (March 2020) and 64% (April 2020), as compared to March 2019 [Citation15], with reductions for individual tests by more than 90% [Citation16]. A closer look at the time course of these changes in the acute setting revealed that hospital admissions for acute coronary syndrome were reduced from mid-February 2020 to the end of March 2020 by 40%, as compared to the previous year. This decline was partly reduced in the following weeks, arriving at a 16% reduction from baseline in the last week of May 2020 [Citation13].
In an attempt to explore the impact of Covid-19 and the associated lockdowns on hypertension management, the European Society of Hypertension (ESH) conducted, in 2020, the first survey among its Excellence Centers [Citation17]. It was observed that the number of patients treated per week by the centers decreased by 90% and that the majority of the centers could not provide ambulatory blood pressure monitoring (ABPM) during the lockdown. In order to investigate these changes in hypertension care in more detail, and to clarify the time course of the reduction in performing hypertension-related diagnostic tests and selected therapeutic procedures, we conducted a second survey among our Excellence Centers in 2021.
Methods
Similar to the first Covid-19 survey of the ESH, we developed a 60-questions electronic survey designed to quantify the impact of Covid-19 and the associated lockdowns in 2020 on 5 diagnostic tests (ABPM, renal artery duplex ultrasound – Duplex RA, renal artery angiography by computed tomography or magnetic resonance imaging – RA CT/MRI, laboratory test for plasma/urinary catecholamines, laboratory test for plasma renin/aldosterone) and one interventional procedure (percutaneous transluminal angioplasty of the renal artery – PTA RA) related to hypertension care (). The survey was drafted by the coordinator of the Excellence Center program (T.W.) and subsequently reviewed and finalised by the Covid-19 Task Force of the ESH. The survey, written in SoGoSurvey software, was made available online to all Excellence Centers between April and June 2021. The participating centers were asked to extract exact numbers of diagnostic tests and selected procedures from departmental and hospital administrative databases for the years 2019 and 2020, divided into 3 months intervals. The results were compiled by ESH staff. The current work was an evaluation of clinical service provided by physicians and nurses and not related to individual patient data, therefore ethical approval was not required.
Table 1. Study questionnaire.
Statistics
Results are presented as medians (interquartile range), as all numerical parameters were not normally distributed. Numbers per time interval were compared, using the Wilcoxon test for paired samples, with Bonferroni correction for multiple testing. Changes in hypertension-related diagnostic tests and therapeutic procedures between 2019 and 2020 were expressed as percentages. Probability (p)-values were calculated with the Friedman test to detect overall differences in reduction between 3-month time intervals; post-hoc analyses using the Wilcoxon test for paired samples using Bonferroni correction were used for pairwise comparison of reduction between 3-month time intervals. Statistical analysis was performed using MedCalc version 13.0.2.0 (MedCalc Software, Mariakerke, Belgium) and Matlab, version 2019b (MathWorks, Natick, MA, USA).
Results
In all, 54 Excellence Centers located in 18 European and 3 non-European countries participated in the survey (10 from Greece, 7 from Italy, 6 from Spain and France, 3 from Belgium and Hungary, 2 from Czech Republic, Germany, Serbia and Switzerland, and 1 from Armenia, Austria, Brazil, Bulgaria, Estonia, Finland, Lebanon, Luxembourg, Poland, Portugal, and Sweden, respectively).
All evaluated diagnostic and therapeutic procedures were performed less often during the pandemic (): The median number of ABPMs dropped from 544 per center in 2019 to 289 in 2020 (p < 0.001), a reduction of 30.8% (, ). Similar changes were observed for the number of Duplex RA (from 88.5 in 2019 to 55 in 2020), the number of CT/MRI RA (from 66 in 2019 to 19.5 in 2020), the number of laboratory tests for catecholamines (from 116 in 2019 to 67.5 in 2020), the number of laboratory tests for renin/aldosterone (from 146 in 2019 to 83.5 in 2020), and the number of PTA RA (from 5 in 2019 to 1 in 2020). Thus, we observed a consistent reduction of hypertension-related diagnostic tests and one selected procedure by roughly one-third. Specifically, the reductions were: for Duplex RA 33.3%, CT/MRI RA 35.1%, laboratory tests for catecholamines 31.7%, laboratory tests for renin/aldosterone 29.7%, and for RA PTA 38.9%, respectively.
Figure 1. Reduction in hypertension-related diagnostic tests and one selected therapeutic procedure from 2019 to 2020. Left side: overall, right side: in 3-month intervals. ABPM: ambulatory blood pressure monitoring; Duplex RA: duplex ultrasound investigations of renal arteries; CT/MRI RA: computed tomographic/magnetic resonance imaging angiography of renal arteries; PTA RA: percutaneous angioplasties of renal arteries.
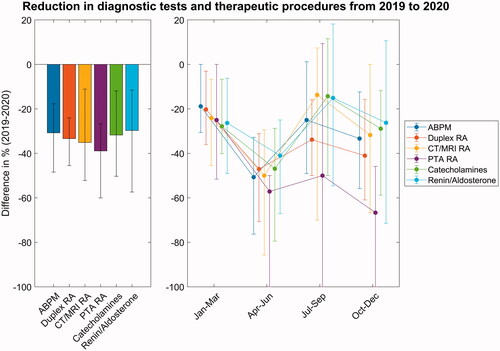
Table 2. Hypertension-related diagnostic tests and one selected therapeutic procedure 2019 and 2020.
Table 3. Changes expressed as percentage [interquartile range] in hypertension-related diagnostic tests and one selected therapeutic procedure from 2019 to 2020.
Breaking down the results by 3-months periods, the reductions analysed in diagnostic procedures and one therapeutic intervention were least pronounced from January to March 2020, reaching a maximum from April to June 2020, slowly returned to the numbers of 2019 in July to September, and increased again from October to December 2020 ().
Discussion
To the best of our knowledge, this is the first multi-national study to quantify the impact of the Covid-19 pandemic on hypertension-associated diagnostic tests and one selected therapeutic procedure. Taking advantage of the Excellence Center network of ESH, we observed on a mainly European level that the Covid-19 pandemic led to a dramatic overall reduction of key diagnostic hypertension-related tests by about one-third and a peak reduction of about one-half in periods with more strict lockdowns.
The current report extends our previous findings in Excellence Centers during the first phase of the pandemic [Citation17], which documented an even greater (by 90%) reduction of face-to-face patient visits. The time course of the reductions in diagnostic tests and therapeutic interventions is fully consistent with our previous findings: the first Covid-19 associated shutdown for hypertension care in Excellence Centers lasted a median of 9 weeks (from March 2020 onwards), and the reductions in diagnostic tests were most striking from April to June 2020. This in turn closely mirrors the evolution of the Covid-19 associated governmental responses across Europe, from school closures to travel bans, expressed in a so-called stringency index [Citation18]. The governmental responses, which can be summarised as ‘lockdown’, started in Europe at the end of February 2020 and were strictest in April and May 2020, somewhat released during summer 2020 and tightened again from October to November 2020 onwards. In parallel, the reductions in hypertension-related diagnostic tests and the evaluated therapeutic procedure just started from January to March 2020 (because the first weeks of the year 2020 were unaffected), were most pronounced from April to June 2020, less pronounced during summer 2020, and increased again from October to December 2020.
The extent of reduction in hypertension-related diagnostic tests in our study (by about 50% from April to June 2020) is of the same magnitude as reported for other diagnostic tests for cardiovascular diseases: global surveys revealed, that diagnostic tests for cardiovascular diseases (transthoracic and transesophageal echocardiography, coronary CT angiography, cardiac MRI, invasive angiography) were reduced by 42% – in March 2020 – and 64% – in April 2020 –, as compared to March 2019 [Citation15], with reductions for individual tests reaching maximum decline of more than 90% [Citation16].
To compensate for the observed reductions in face-to-face consultations, an increase in the use of telehealth using self-home blood pressure monitoring (HBPM) has been recommended in hypertension care [Citation19]. HBPM can be used to confirm or disprove the presence of hypertension in the setting of elevated or normal office blood pressure [Citation20], thus allowing the diagnosis of established, white coat hypertension or masked hypertension. However, as recently outlined [Citation21], the use of HBPM also faces some limitations. Thus, although increasing the use of HBPM may to some degree have attenuated the decrease of Covid-19 lockdown-associated reductions of ABPM, the use of HBPM cannot fully substitute ABPM in several clinical scenarios and needs training and supervision to avoid its drawbacks, such as the use of unreliable devices, measurement in inappropriate posture and conditions, and misreporting of readings by patients [Citation21]. More important, for all other hypertension-related diagnostic tests in our study, alternatives using telehealth methods are not available.
In an excellent summary, the World Health Organisation (WHO) stated that [Citation22], ‘large scale physical distancing measures and movement restrictions, often referred to as ‘lockdowns’, can slow Covid-19 transmission by limiting contact between people. However, these measures can have a profound negative impact on individuals, communities, and societies by bringing social and economic life to a near stop’. On top of that, and worsening the situation, lockdowns considerably impaired healthcare for non-Covid-19 diseases. As medical care even for acute health problems and life-threatening conditions such as myocardial infarctions was compromised [Citation13], healthcare for chronic conditions was – not unexpectedly – much more affected [Citation6,Citation7,Citation9,Citation11]. Hypertension is a classic paradigm of chronic cardiovascular disease and remains the major preventable cause of cardiovascular disease and all-cause death globally, including in Europe [Citation20,Citation23,Citation24]. Although our findings do not show nor necessarily imply a subsequent increase in hypertension-related morbidity and mortality in the future, they may serve as an alarming signal to alert physicians, but also healthcare systems and administrations to monitor closely hypertension awareness, treatment and control rates now and in the future. The next step is to understand the immediate impact of the Covid-19 pandemic on blood pressure levels. Therefore, the Covid-19 Task Force of the ESH has initiated the ESH ABPM COVID-19 study (ClinicalTrials.gov Identifier: NCT05167240), which will compare ABPM results obtained before and during the COVID-19 lockdown in treated hypertensive patients.
A possible limitation of our survey is its retrospective nature and the possibility that some of the investigations have been performed not exclusively for the diagnostic workup of hypertension. Furthermore, a selection bias (Excellence Centers with the availability of the data and less dramatic reductions may have been more willing to report their performance) may have affected the results. Finally, Excellence Centers are mainly secondary and tertiary care centres, and the situation regarding ABPM in primary care may have been different.
In summary, these data document a considerable decline in the use of hypertension-related diagnostic tests and selected therapeutic procedures during the first year of the Covid-19 pandemic, with the largest reduction seen during the first lockdown in the spring of 2020. The long-term consequences regarding blood pressure control and, ultimately, cardiovascular events remain to be investigated.
Author contributions
T.W., R.K., A.J., K.T. and G.M. developed the questionnaire and the study design. C.C.M. performed the statistical analyses. T.W. wrote the first draft of the article and revised it according to coauthors’ and reviewers’ feedback. J.A., T.B., M.v.d.G., P.G., and B.V. were the top 5 recruiting centres. Most of the writing group members contributed data to the analysis, and all writing group members were involved in the interpretation of the results, the development and the submission of the article. The remaining contributing Excellence Centers include:
Writing group:
Thomas Weber (1), Jaques Amar (2), Tine de Backer (3), Thilo Burkard (4), Marcus van der Giet (5), Philippe Gosse (6), Andrzej Januszewicz (7), Thomas Kahan (8), Giuseppe Mancia (9), Christopher C. Mayer (10), Maria Lorenza Muiesan (11), George S. Stergiou (12), Konstantinos Tsioufis (13), Bernard Vaisse (14), and Reinhold Kreutz (5) (writing group). Covid-10 Task Force of the European Society of Hypertension.
Contributing Excellence Centers:
Ábrahám György (15), Istvan Barna (16), Weimar Kunz Sebba Barroso (17), Miguel Camafort-Babkowski (18), Claude Braun (19), Santina Cottone (20), Kathrin Danninger (1), Georg Ehret (21), Daniel Gordin (22), Guido Grassi (23), Charalampos Grassos (24), Fernando Jaén Águila (25), Zoltan Jarai (26), Klaus Kisters (27), Vasilios Kotsis (28), Jean-Marie Krzesinski (29), Marilucy Lopez-Sublet (30), Dragan Lovic (31), Empar Lurbe (32), Thomas K. Makris (33), Athanasios J. Manolis (34), Maria Marketou (35), Pietro Minuz (36), Jean-Jacques Mourad (37), Edgar Nasr (38), Patricia Van der Niepen (39), Olivier Ormezzano (40), Ioannis Papadakis (41), Jorge Polonia (42), Dimitrios Papadopoulos (43), Dimitar Raev (44), Marek Rajzer (45), Josep Redon (46), Nicolás Roberto Robles (47), Riccardo Sarzani (48), Filipo Scalise (49), Anna Oliveras Serrano (50), Vesna Stojanov (51), Costas Thomopoulos (33), Jan Vaclavik (52), Franco Veglio (53), Margus Viigimaa (54), Jiri Widimski (55), Pantelis Zebekakis (56), Parounak Zelveian (57).
1 … Cardiology Department, Klinikum Wels-Grieskirchen, Wels, Austria
2 … Toulouse University Hospital, France
3 … Cardiovascular Center, Heymans Institute of Clinical Pharmacology, University Hospital Gent, Belgium
4 … Medical Outpatient Department and Hypertension Clinic, University Hospital Basel, Basel, Switzerland
5 … Hypertension Centre Berlin Charité, Berlin, Germany
6 … Unité Hypertension Artérielle, University of Bordeaux, Bordeaux, France
7 … Department of Hypertension, Institute of Cardiology, Warsaw, Poland
8 … Department of Cardiology, Danderyd University Hospital, Stockholm, Sweden
9 … University of Milano-Bicocca, Milan, Italy
10 … Austrian Institute of Technology, Vienna, Austria
11 … Centro per la Prevenzione e Cura dell'ipertensione Arteriosa, Department of Clinical and Experimental Sciences, University of Brescia and ASST Spedali Civili, Brescia, Italy
12 … Hypertension Center STRIDE-7, National and Kapodistrian University of Athens, School of Medicine, Third Department of Medicine, Sotiria Hospital, Athens, Greece
13 … 1st Cardiology Clinic, National and Kapodistrian University of Athens, Greece
14 … Service de Rythmologie et d'Hypertension, Pôle Cardiovasculaire et Thoracique, Marseille, France
15 … Nephrology-Hypertension Center 1st Dept. of Medicine, University of Szeged, Hungary
16 … Department of Internal Medicine and Oncology, Semmelweis University, Budapest, Hungary
17 … Hypertension League, Medicine School, Federal University of Goiás, Brasil
18 … Hypertension Centre Hospital Clínic- IDIBAPS, University of Barcelona, Spain
19 … Centre Hospitalier Kirchberg, Hôpitaux Robert Schuman, Luxembourg
20 … Nephrology Unit with Hypertension Excellence Centre, University of Palermo Italy
21 … Department of Cardiology, University of Geneva, Switzerland
22 … Helsinki Hypertension Centre of Excellence, Abdominal Center Nephrology, Minerva Institute for Medical Research, University of Helsinki, Helsinki University Central Hospital, Helsinki , Finland
23 … Clinica Medica Ospedale San Gerardo, Monza, Italy
24 … Hypertension Clinic, Department of Cardiology, KAT General Hospital, Athens, Greece
25 … Vascular Risk Unit, Virgen de las Nieves University Hospital, Granada, Spain
26 … Szt. Imre Teaching Hospital, Budapest, Hungary
27 … Medical Clinic I, St. Anna Hospital, Herne, Germany
28 … Hypertension-24h ABPM Center, Papageorgiou Hospital, Nea Efkarpia, Greece
29 … Centre Universitaire d’approche diagnostique et thérapeutique de l’hypertension artérielle CHU de Liège, Liège Sart Tilman, Belgium
30 … AP-HP Hôpital Avicenne, Centre d’Excellence Européen en Hypertension Artérielle, Médecine Interne, Bobigny, France. INSERM UMR 942 MASCOT, Paris 13-Université Paris Nord. FCRIN INI-CRCT (Cardiovascular and Renal Clinical Trialists), Nancy, France.
31 … Clinic for internal disease Intermedica, Cardiology Department, Hypertension Center Singidunum University, School of Medicine, Nis, Serbia
32 … Pediatric Department, Hospital General, University of Valencia, Valencia, Spain
33 … Dept. of Cardiology, "Helena Venizelou" Maternity and General Hospital, Athens, Greece
34 … Hypertension Center Metropolitan Hospital, Athens, Greece
35 … Cardiology Department of Heraklion University Hospital, Heraklion, Greece
36 … UOC Medicina Generale per lo Studio ed il Trattamento della Malattia Ipertensiva, Dipartimento di Medicina Università di Verona ed Azienda Ospedaliera Universitaria Integrata Verona Policlinico GB Rossi, Italy
37 … Groupe Hospitalier Paris-Saint Joseph, Paris, France
38 … St. George University Medical Center, Beirut, Lebanon
39 … Department of Nephrology & Hypertension, Universitair Ziekenhuis Brussel (VUB), Belgium
40 … Hypertension et Athérothrombose - Service de Cardiologie - Pôle Thorax et Vaisseaux - CHU Grenoble, France
41 … Hypertension Unit, Department of Internal Medicine, University Hospital of Heraklion, Heraklion, Greece
42 … Faculty of Medicine of Porto, Portugal
43 … Hypertension Clinic, University Hospital Laiko, Athens
44 … Clinic of Internal Medicine, University Hospital "St. Anna", Sofia, Bulgaria
45 … I st Department of Cardiology, Interventional Electrocardiology and Arterial Hypertension, Jagiellonian University Medical College, Poland
46 … Hypertension Clinic, Internal Medicine, Hospital Clinico, University of Valencia, Valencia, Spain
47 … Nephrology Department & Hypertension Unit, Hospital Universitario de Badajoz, Universidad de Extremadura, Spain
48 … Internal Medicine and Geriatrics, Hypertension Excellence Centre, University Politecnica delle Marche and IRCCS-INRCA, Ancona, Italy
49 … Centro Studi Ipertensione e Malattie Vascolari, Policlinico di Monza, Verano Brianza, Italy
50 … Hypertension Unit-Hospital del Mar, Barcelona, Spain
51 … The multidisciplinary center for Polyclinic Diagnostics, Assessment and Treatment of Blood Pressure Disorders, Clinic for Cardiology,Clinical Centre of Serbia; Faculty of Medicine, University of Belgrade, Serbia
52 … Department of Internal Medicine and Cardiology, University Hospital Ostrava and Ostrava University Faculty of Medicine, Ostrava, Czech Republic
53 … Internal Medicine and Hypertension Division, Department of Medical Sciences, University of Turin, Italy
54 … North Estonia Medical Centre, Tallinn University of Technology, Tallinn, Estonia
55 … Centre for hypertension, Charles University, IIIrd Internal dep., Prague, Czech Republic
56 … Hypertension Unit of the First Department of Medicine Aristotle University of Thessaloniki, AHEPA Hospital, Greece
57 … Center of Preventive Cardiology, Institute of Cardiology named after Levon Hovhannisyan, Yerevan, Armenia
Acknowledgements
We are indebted to Mandy Eigner, program coordinator of the ESH, for dissemination of the SoGo survey among the Excellence Centers and for compiling the results.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Kreutz R, Dobrowolski P, Prejbisz A, et al. Lifestyle, psychological, socioeconomic and environmental factors and their impact on hypertension during the coronavirus disease 2019 pandemic. J Hypertens. 2021;39(6):1077–1089.
- Onyeaka H, Anumudu CK, Al-Sharify ZT, et al. COVID-19 pandemic: a review of the global lockdown and its far-reaching effects. Sci Prog. 2021;104(2):368504211019854.
- Ahmad FB, Anderson RN. The leading causes of death in the US for 2020. JAMA. 2021;325(18):1829–1830.
- Parasa S, Reddy N, Faigel DO, et al. Global impact of the COVID-19 pandemic on endoscopy: an international survey of 252 centers from 55 countries. Gastroenterology. 2020;159(4):1579–1581.
- Gurney JK, Millar E, Dunn A, et al. The impact of the COVID-19 pandemic on cancer diagnosis and service access in New Zealand-a country pursuing COVID-19 elimination. Lancet Reg Health West Pac. 2021;10:100127.
- Colorectal Cancer COVID Research Collaborative. The impact of the COVID-19 pandemic on colorectal cancer service provision. Br J Surg. 2020;107:e521–e522.
- Cacciamani GE, Shah M, Yip W, et al. Impact of covid-19 on the urology service in United States: perspectives and strategies to face a pandemic. Int Braz J Urol. 2020;46(1):207–214.
- Ong MT, Ling SK, Wong RM, et al. Impact of COVID-19 on orthopaedic clinical service, education and research in a university hospital. J Orthop Translat. 2020;25:125–127.
- Wong JSH, Cheung KMC. Impact of COVID-19 on orthopaedic and trauma service: an epidemiological study. J Bone Joint Surg Am. 2020;102(14):e80.
- Liebensteiner MC, Khosravi I, Hirschmann MT, Board of the AGA-Society of Arthroscopy and Joint-Surgery, et al. Massive cutback in orthopaedic healthcare services due to the COVID-19 pandemic. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1705–1711.
- Quigley M, Earnest A, Szwarcbard N, et al. Impact of COVID-19 on diabetes health care and service provision in Australian diabetes centers. Diabetes Care. 2021;44(8):e163–e164.
- Fersia O, Bryant S, Nicholson R, et al. The impact of the COVID-19 pandemic on cardiology services. Open Heart. 2020;7(2):e001359.
- Mafham MM, Spata E, Goldacre R, et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396(10248):381–389.
- Ball S, Banerjee A, Berry C, et al. Monitoring indirect impact of COVID-19 pandemic on services for cardiovascular diseases in the UK. Heart. 2020;106(24):1890–1897.
- Einstein AJ, Shaw LJ, Hirschfeld C, et al. International impact of COVID-19 on the diagnosis of heart disease. J Am Coll Cardiol. 2021;77(2):173–185.
- Hirschfeld CB, Shaw LJ, Williams MC, et al. Impact of COVID-19 on cardiovascular testing in the United States versus the rest of the world. JACC Cardiovascular Imaging. 2021;14(9):1787–1799.
- The corona-virus disease 2019 pandemic compromised routine care for hypertension: a survey conducted among excellence centers of the European Society of Hypertension. J Hypertens. 2021;39:190–195.
- University of Oxford Blavatnik School of Government. COVID-19 Government Response Tracker [Internet]. 2022 [cited 2022 Jan 15]; Available from: https://covidtracker.bsg.ox.ac.uk/stringency-map
- Ferdinand KC, Vo TN, Echols MR. State-of-the-art review: hypertension practice guidelines in the era of COVID-19. Am J Prev Cardiol. 2020;2:100038.
- Williams B, Mancia G, Spiering W, et al. 2018 practice guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC task force for the management of arterial hypertension. J Hypertens. 2018;36(12):2284–2309.
- Stergiou GS, Palatini P, Parati G, et al. 2021 European society of hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39(7):1293–1302.
- World Health Organization. Coronavirus disease (COVID-19): herd immunity, lockdowns and COVID-19 [Internet]. Geneva (Switzerland): WHO; 2022 [cited 2022 January 15]; Available from: https://www.who.int/news-room/questions-and-answers/item/herd-immunity-lockdowns-and-covid-19.
- Murray CJ, Barber RM, Foreman KJ, et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet. 2015;386(10009):2145–2191.
- Lopez AD, Mathers CD, Ezzati M, et al. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367(9524):1747–1757.
