Abstract
Purpose
In patients with diabetes, unrecognised hypertension is a serious problem risk factor for the development and progression of chronic complications. The study aimed to determine the prevalence of masked hypertension in normotensive diabetic patients, the factors affecting it, and its association with diabetes complications using ambulatory blood pressure monitoring (ABPM).
Materials and methods
A cross-sectional observational study was conducted on 150 normotensive diabetic patients. Patients were subjected to an interview and clinical examination to record demographic data, epidemiological data, and significant past history. ABPM was performed for each patient. Urine samples, echocardiogram, and ophthalmologic fundoscopy were done to check for diabetes-related complications.
Results
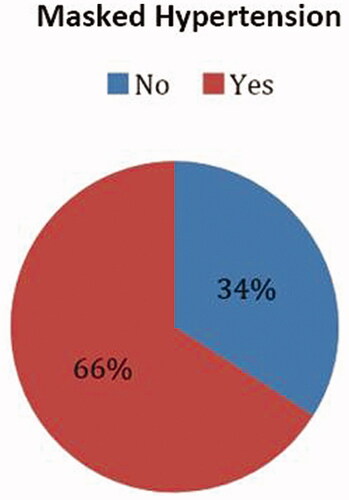
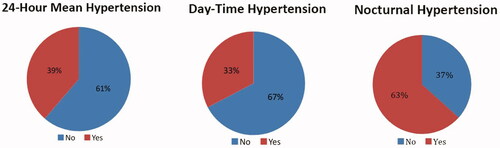
The mean age of all participants was 56.7 ± 7.8 years. A total of 93 patients (62%) were males. 99 (66%) patients had masked hypertension. A total of 85 (56.7%) were non-dippers, 49 (32.7%) were dippers, 1 (0.7%) was extreme dipper and 15 (10%) were reverse dippers. Non-dipping and reverse dipping were associated with concentric left ventricular hypertrophy LVH (p < .001). Masked hypertension was associated with concentric LVH (p = .001) and nephropathy (p =.008) whereas, nocturnal hypertension was associated with concentric LVH (p = .001) and nephropathy (p =.003).
Conclusions
A single office blood pressure (BP) reading cannot rule out hypertension in patients with diabetes. Regardless of hypertension, clinicians should have all patients, especially patients with diabetes, undergo ABPM at least once. Masked hypertension, changes in nocturnal dipping and other phenomena that raise the risk of diabetes complications but cannot be measured by office BP can be measured by ABPM, and thus ABPM can provide a good prognostic benefit.
Introduction
Hypertension is a major risk factor for the development and progression of chronic complications in type 2 diabetes mellitus (T2DM) [Citation1]. It is thought to be responsible for 35–75% of diabetes complications [Citation2]. Blood pressure (BP) ≥ 115/75 mmHg in patients with diabetes is highly associated with an increased incidence of atherosclerotic cardiovascular disease, heart failure, retinopathy, renal disease, and eventually death, indicating that controlling BP is an important determinant in the clinical consequences of DM [Citation1].
In diabetic patients, undetected hypertension is a serious problem and hypertensive target organ damage progresses faster in them than in patients without diabetes [Citation3]. Moreover, missed diagnoses of hypertension and poor BP management are fairly common in them [Citation4,Citation5]. According to an earlier study, one-third of normotensive T2DM patients have masked hypertension (normal office BP but elevated true BP), which is invariably associated with an increase in albuminuria and left ventricular hypertrophy (LVH) [Citation6]. This makes the diagnosis of masked hypertension in this group of utmost importance. Routinely recorded office BP is vulnerable to numerous kinds of errors, which probably influences both the epidemiology and clinical assessment of hypertension. Furthermore, office BP gives just a ‘snap-shot’ of the patient’s real BP and may not necessarily reflect true BP. ABPM is one of the important solutions for this problem. BP values obtained through ABPM in patients with diabetes are found to correlate better than office BP with organ (in particular renal [Citation4]) damage and cardiovascular events [Citation2,Citation7]. For measurements derived with ABPM, the correlation between BP and target organ damage, and vascular risk is stronger as compared to office BP. Patient prognosis is also evidently better when ABPM is utilised for monitoring BP in patients with diabetes [Citation2]. BP determination by ABPM allows better patient risk stratification and is an essential utility for BP control.
This study concentrates on these aspects of ABPM, justifying its use in a normotensive diabetic population by describing the relationship between ABP parameters, such as nocturnal dipping, masked hypertension, and nocturnal hypertension with microvascular and cardiovascular complications of T2DM, and thus about being a better predictor of these complications than office BP. The study aimed to determine the prevalence of masked hypertension in normotensive diabetic patients, the factors affecting it, and its association with diabetes complications using ambulatory blood pressure monitoring (ABPM).
Materials and methods
Study design and participants
A cross-sectional observational study was conducted on normotensive diabetic patients who visited the in-patient department (IPD) and out-patient department (OPD) of Internal Medicine at Sir JJ Hospital in Mumbai between January 2019 and December 2020. The research only included patients who met the defined inclusion and exclusion criteria. Inclusion criteria: 1) Patients diagnosed with T2DM (aged > 30 years at diagnosis of DM, no previous episode of ketoacidosis and treated with insulin only after five years of diagnosis [if treated]). 2) HbA1c between 6.5 and 8.5% at the time of inclusion. 3) Patients who gave written informed consent. Exclusion criteria: 1) BP at office evaluation ≥ 140/90 mmHg on two occasions taken 5 min apart. 2) Patients with serum creatinine > 1.5 mg/dl or end-stage renal disease. 3) Patients with a history of stroke or ischaemic heart disease. 4) Patients with atrial fibrillation and sleep apnoea, as well as night shift workers. 5) Patients who were not able to attend the OPD for two consecutive days for completing ABPM. 6) Patients on any anti-hypertensive drugs or any other drugs. 7) Patients who did not give written informed consent.
Collection of data
After obtaining approval from the institutional ethics committee (Document Number: IEC/PG/377/Oct/2018, Institutional Ethics Committee, Grant Government Medical College and Sir JJ Group of Hospitals, Byculla, Mumbai), patients were subjected to an interview and clinical examination to record demographic data and epidemiological data like time since the diagnosis of DM, past history of stroke or ischaemic heart disease or any cardiovascular events (defined as an episode of CCU admission, myocardial infarction, history of coronary artery bypass graft surgery or percutaneous intervention), and family history of DM, hypertension, stroke or ischaemic heart diseases. Anthropometric data, like height and weight, were recorded. BMI was calculated with weight in kg/height in m2.
BP reading for each patient was obtained under-standardised conditions using the patients’ non-dominant arm with an automatic blood pressure monitor (Omron HEM 8712 Blood Pressure Monitor, Omron Corporation, Kyoto, Japan). Readings were taken with the patient in the sitting position after five minutes of rest. A mean office BP was calculated with three readings taken using the automatic BP monitor. Patients with mean BP < 140/90 from three readings were included in the study.
From this cohort, after applying careful inclusion and exclusion criteria, patients were considered further for the study. Of these subjects, 10 ml of venous blood sample was taken for routine laboratory tests like high-performance liquid chromatography (HbA1c), serum lipid profile, renal function tests, and liver biochemistries. All participants were screened for diabetic retinopathy with the help of an ophthalmologic fundoscopic examination. Early morning spot urine was obtained for testing urine albumin and creatinine. The urine albumin to creatinine ratio was calculated (UACR). An echocardiogram was obtained using standard parasternal and apical views, and patients were classified based on concentric LVH versus normal study. The device used for the echocardiography was Philips Affiniti 70 (Philips Corporation, Eindhoven, Netherlands).
Ambulatory blood pressure measurement
In our study, we used the SunTech Medical® Oscar 2™ Ambulatory Blood Pressure Monitor (SunTech Medical, Morrisville, NC) for measuring ambulatory BP. Patients were advised to continue their routine activities during the study. Sleep time was defined as the time between when the patient went to bed and when he or she awoke in the morning. ABP recordings were interpreted in the form of mean daytime systolic and diastolic BP readings, mean night-time systolic and diastolic BP readings, mean 24-hour systolic and diastolic BP readings, and nocturnal dipping.
Outcome measures
depicts the outcome definitions of the study. Patients’ outcomes were recorded based on these criteria.
Table 1. Outcome definitions in the study.
Primary outcomes
The descriptive reporting of the prevalence of the various parameters of ABP and diabetes-related complications (viz. day-time hypertension, night-time hypertension, masked hypertension [Citation8], and 24-hours ABP hypertension) were the primary outcomes of this study.
Secondary outcomes
The associations and correlations (wherever applicable) between abnormal ABP patterns (nocturnal dipping, nocturnal hypertension, and masked hypertension) and complications of diabetes mellitus were studied and reported.
Analysis of data
The data was entered in Microsoft Office Excel version 2016, and the statistical analysis was done using Statistical Package for Social Sciences version 20.0 (SPSS Inc., Chicago, IL). Categorical variables were presented in number and percentage (%), and continuous variables were presented as mean ± SD and median, as appropriate. Normality of data was tested by Kolmogorov–Smirnov test. If the normality was rejected then non-parametric tests were used for analysis. Quantitative variables were compared using an unpaired t-test/Mann–Whitney U test as appropriate. Qualitative variables were compared using the Chi-square test/Fisher’s exact test. The differences between the group of subjects with normal BP and subjects with masked hypertension were obtained by statistical parameters using the t-test. All tests were considered statistically significant for a two-tailed significance level (p) ≤ .05.
Results
Participants
Through the first screening, 167 of the 291 individuals with T2DM who visited the hospital during the study period were considered eligible to participate in the research. During the evaluation, the most common cause for exclusion was the presence of hypertension among the subjects. A total of 86 patients were hypertensive, 13 patients denied informed consent, 14 had their HbA1C above 8.5%, four were having kidney disease and seven patients had a history of stroke or ischaemic heart disease. A total of 17 patients were excluded from the final analysis due to incomplete ABP data. The remaining 150 patients were included in the final analysis.
Demographic characteristics
The mean (SD) age of all participants was 56.7 ± 7.8 years. A total of 93 patients (62%) were males, and 57 (38%) patients were females. The mean duration from diagnosis of diabetes was 5.2 ± 4.7 years. A total of 40 participants (27%) were either smokers or used any other form of tobacco. A total of 39 (26%) participants consumed alcohol. The mean urine ACR of the participants was 80 ± 177 mg/g. A total of 16 (11%) participants had diabetic retinopathy and 17 (11.3%) had concentric LVH.
ABP parameters
In the study, 99 (66%) patients were found to have masked hypertension. A total of 58 (38.7%) patients, 49 (32.7%) patients, and 95 (63.3%) patients had 24-hours mean hypertension, day-time hypertension and nocturnal hypertension, respectively. pictures the comparison of the baseline characteristics of the population under masked hypertension and normal BP groups. Among the baseline characters, mean serum HDL was higher in the normotensive group (p = .02), and mean serum VLDL level was higher in the masked hypertension group (p = .01). The distributions of masked hypertension and abnormal ABP parameters are illustrated in and .
Table 2. Comparison of the baseline characteristics of the population (mean ± SD).
Nocturnal dipping patterns
Of the total 150 subjects studied, 85 (56.7%) were non-dippers, 49 (32.7%) were dippers, 1 (0.7%) was extreme dipper and 15 (10%) were reverse dippers. depicts the association of nocturnal dipping patterns with complications of diabetes. Concentric LVH was the only complication of diabetes that is found to be associated with nocturnal dipping variations (non-dippers and reverse dippers) (p < .001). depicts the frequency of diabetes complications in dippers, extreme dipper, non-dippers, and reverse dippers.
Figure 3. Bar graph showing the frequency of diabetes complications in dippers, extreme dippers, non-dippers and reverse dippers.
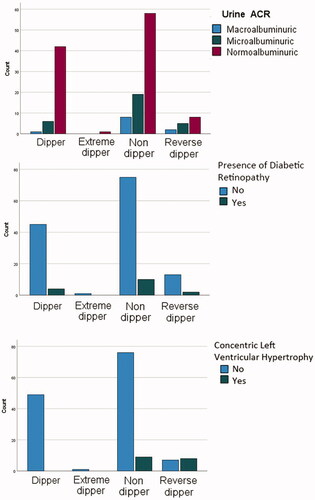
Table 3. Association of abnormal ABP parameters with complications of diabetes.
Non-dippers, dippers and reverse dippers showed a weakly negative but statistically insignificant correlation with concentric LVH.
Masked hypertension
shows the association between masked hypertension and diabetes complications. Masked hypertension was found to have a significant association with concentric LVH and albuminuria.
Nocturnal hypertension
shows the association between nocturnal hypertension and diabetes complications. There is a significant association between nocturnal hypertension and concentric LVH, as well as nocturnal hypertension and albuminuria, according to the data.
Discussion
This study found that 66, 38.7, 32.7 and 63.3 percent of the patients had masked hypertension, 24-hours mean hypertension, day-time hypertension and nocturnal hypertension, respectively. The presence of concentric LVH was found to be significantly associated with masked hypertension, nocturnal hypertension and nocturnal dipping. We found albuminuria to be strongly associated with masked and nocturnal hypertension. Diabetic retinopathy was not found to be associated with any of these variables.
The majority of previous studies related to the utility of ABPM have been conducted on hypertensive patients [Citation9–14]. The present study was conducted in normotensive patients to find the association of abnormal ABPM parameters with DM complications. Since masked hypertension was identified as a novel risk factor in T2DM [Citation5], studies of this sort have emphasised the necessity of detecting masked hypertension in patients with diabetes. In this study, we found a high prevalence of masked hypertension, non-dipping and reverse dipping patterns, and nocturnal hypertension in normotensive patients with diabetes. A significant association of these parameters with diabetes-related complications was also found. ABPM and its significance are largely underrated in India despite the rising trends of cardiovascular events, probably due to financial constraints, limited availability of ABPM devices and low level of awareness among physicians.
This study was an observational study conducted in a tertiary care institute in a developing country where the relative prevalence of hypertension is low. We included normotensive patients in the study so that we could specifically assess risk factors in this population. Usually, in patients with DM, hypertension and nephropathy often coexist. The prevalence of nephropathy was 58.33% in hypertensive patients, as reported in the study conducted by Equiluzbruck et al. [Citation15], much higher than in our study. However, it is important to note that the degree of albuminuria varies depending on the population studied, subjects on antihypertensive medications, and other factors such as prostate disease or infection. Studies by Najafi et al. [Citation2] and Kramer et al. [Citation16] show a higher prevalence of diabetic retinopathy. However, surprisingly presence of DR in these patients was associated with an afternoon rise in BP in their study, in contrast to our study where we did not get any ABP parameter associated with DR. In their study, Fogari et al. showed that in non-dipping patients, the prevalence of LVH and atherosclerotic cardiovascular disease increased, consistent with our study [Citation17].
The prevalence of the non-dipper pattern in the medical literature is highly inconsistent, ranging broadly from 30 to 73% [Citation18], possibly because of disparities between the different studies in the population studied, relatively small sample sizes, the use of single and therefore, poorly reproducible ABPM and inadequate definition of the activity and rest periods. This disparity may also be due to the recognised events related to non-dipping and studies concentrating only on them, e.g. secondary hypertension, heart failure, sleep disturbances, shift working, autonomic neuropathy and LVH [Citation15].
Even hypertensive T2DM patients seem to be equally affected by these circadian BP abnormalities. For instance, in the study conducted by Moran et al. [Citation19], 70% of patients lacked the normal fall in nocturnal BP (non-dippers) despite 80% of the population under study being treated with anti-hypertensives. The non-dipping phenomenon was observed in 38% of hypertensive DM subjects in the Hänninen et al.’s study [Citation20].
The prevalence of masked hypertension in the population is surprisingly very high in this study. More recently, in the study conducted by Hadjkacem F et al. [Citation21], the prevalence of masked hypertension in type 2 diabetics was 64%, comparable with our study. Earlier, Anstey et al. [Citation22] and Marchesi et al. [Citation23] found the prevalence of masked hypertension 25.8 and 47%, respectively. This large variation might be due to differences in the definition of normal ABP levels as well as due to variations in patient demographic characteristics, such as age and BMI [Citation24]. This is particularly important in developing Asian countries because the International Ambulatory Blood Pressure Registry: Telemonitoring of Hypertension and Cardiovascular Risk Project Study (ARTEMIS) said that masked hypertension was more likely to be diagnosed in Asia than in any other region [Citation25].
The relatively high prevalence of nocturnal hypertension in our study could be because of multiple contributing factors like sleep apnoea and the lack of previous normotensive T2DM studies for comparison. Larger sample size studies and similar normotensive diabetic studies in India are further needed to substantiate these results.
It had previously been stated in the literature that identification by ambulatory monitoring could be of prognostic and therapeutic value [Citation17]. In line with this, our study highlights the important prognostic benefits of ABPM. Prognostic benefits and superiority of ABPM compared to office BP has been confirmed in many studies previously [Citation12,Citation14,Citation26,Citation27]. Further studies with larger sample sizes, especially in the Indian population, are needed to substantiate these results. The study holds the advantage in terms of ABPM being put on an OPD basis which removes the ‘stress’ of hospitalisation and measures BP values in the subject’s comfortable environment. In clinical settings, ABPM should be recommended for normotensive diabetic patients regularly, considering its prognostic benefits.
Limitations of the study
The study being cross-sectional holds off conclusions about the cause-and-effect relationship between masked hypertension and the renal and echocardiographic outcomes and also does not provide prognostic information. The study being a one-time study, the accuracy and reproducibility of ABPM could not be commented upon. There is no information on the quality of sleep since sleep apnoea and degree of desaturation during sleep may interfere with the dipping pattern. A smaller sample size may have led us to the low power of the study. Future studies with larger sample sizes should be planned.
Conclusions
A simple single reading of office BP cannot rule out the presence of hypertension in patients with diabetes. Regardless of hypertension, physicians should have the general population, particularly diabetic patients, undergo ABPM at least once. The presence of an altered circadian BP rhythm/reverse circadian BP profile in the ABPM data should alert the clinician to the possibility of problems and prompt measures to treat hypertension adequately, mainly nocturnal hypertension. Because nocturnal BP has such a high predictive value for diabetes complications, it is critical to pay more attention to it in clinical practice.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
References
- de Boer IH, Bangalore S, Benetos A, et al. Diabetes and hypertension: a position statement by the American diabetes association. Diabetes Care. 2017;40(9):1273–1284.
- Najafi MT, Khaloo P, Alemi H, et al. Ambulatory blood pressure monitoring and diabetes complications: targeting morning blood pressure surge and nocturnal dipping. Medicine. 2018;97(38):e12185.
- Eguchi K, Ishikawa J, Hoshide S, et al. Masked hypertension in diabetes mellitus: a potential risk. J Clin Hypertension. 2007;9(8):601–607.
- Parati G, Bilo G. Should 24-h ambulatory blood pressure monitoring be done in every patient with diabetes? Diabetes Care. 2009;32(2):S298–S304.
- Wijkman M, Länne T, Engvall J, et al. Masked nocturnal hypertension–a novel marker of risk in type 2 diabetes. Diabetologia. 2009;52(7):1258–1264.
- Leitão CB, Canani LH, Silveiro SP, et al. Ambulatory blood pressure monitoring and type 2 diabetes mellitus. Arq Bras Cardiol. 2007;89(5):315–321.
- Kario K, Hoshide S, Chia Y-C, et al. Guidance on ambulatory blood pressure monitoring: a statement from the HOPE Asia network. J Clin Hypertens (Greenwich). 2021;23(3):411–421.
- Pickering TG, Eguchi K, Kario K. Masked hypertension: a review. Hypertens Res. 2007;30(6):479–488.
- Bendzala M, Kruzliak P, Gaspar L, et al. Prognostic significance of dipping in older hypertensive patients. Blood Press. 2015;24(2):103–110.
- Rugnath T, Pillay BJ, Cassimjee MH. Twenty-four hour ambulatory blood pressure monitoring in general practice. S Afr Med J. 2000;90:898–904.
- Verdecchia P, Porcellati C, Schillaci G, et al. Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension. Hypertension. 1994;24(6):793–801.
- Dolan E, Stanton A, Thijs L, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension. 2005;46(1):156–161.
- Salles GF, Reboldi G, Fagard RH, et al. Prognostic effect of the nocturnal blood pressure fall in hypertensive patients: the ambulatory blood pressure collaboration in patients with hypertension (ABC-H) Meta-Analysis. Hypertension. 2016;67(4):693–700.
- Grezzana GB, Stein AT, Pellanda LC. 24-Hour ambulatory blood pressure monitoring predicts outcomes of hypertensive patients in primary care: a cohort study. Int J Cardiovasc Sci 2017;30:285–292.
- Equiluzbruck S, Schnack C, Kopp H, et al. Nondipping of nocturnal blood pressure is related to urinary albumin excretion rate in patients with type 2 diabetes mellitus. Am J Hypertens. 1996;9(11):1139–1143.
- Kramer CK, Leitão CB, Canani LH, et al. Late afternoon blood pressure increase is associated with diabetic retinopathy in normotensive type 2 diabetes mellitus patients. Diabetes Res Clin Pract. 2009;84(1):e12–e14.
- Fogari R, Zoppi A, Malamani GD, et al. Ambulatory blood pressure monitoring in normotensive and hypertensive type 2 diabetes. Prevalence of impaired diurnal blood pressure patterns. Am J Hypertens. 1993;6(1):1–7.
- American Diabetes Association. Implications of the United Kingdom prospective diabetes study. Diabetes Care. 2000;23 (1):S27–S31.
- Moran A, Palmas W, Pickering TG, et al. Office and ambulatory blood pressure are independently associated with albuminuria in older subjects with type 2 diabetes. Hypertension. 2006;47(5):955–961.
- Hänninen J, Takala J, Keinänen-Kiukaanniemi S. Blood pressure control in subjects with type 2 diabetes. J Hum Hypertens. 2000;14(2):111–115.
- Hadjkacem F, Triki F, Frikha H, et al. Masked arterial hypertension in patients with type2 diabetes mellitus: prevalence, associated factors and cardiovascular impact. Ann Cardiol Angeiol (Paris). 2022. doi: 10.1016/j.ancard.2021.10.018.
- Anstey DE, Muntner P, Bello NA, et al. Diagnosing masked hypertension using ambulatory blood pressure monitoring, home blood pressure monitoring, or both? Hypertension. 2018;72(5):1200–1207.
- Marchesi C, Maresca A, Solbiati F, et al. Masked hypertension in type 2 diabetes MellitusRelationship with Left-Ventricular structure and function. Am J Hypertens. 2007;20(10):1079–1084.
- Leitão CB, Canani LH, Kramer CK, et al. Masked hypertension, urinary albumin excretion rate, and echocardiographic parameters in putatively normotensive type 2 diabetic patients. Diabetes Care. 2007;30(5):1255–1260.
- Hoshide S, Cheng HM, Huang Q, et al. Role of ambulatory blood pressure monitoring for the management of hypertension in Asian populations. J Clin Hypertens (Greenwich). 2017;19(12):1240–1245.
- Niiranen TJ, Mäki J, Puukka P, et al. Office, home, and ambulatory blood pressures as predictors of cardiovascular risk. Hypertension. 2014;64(2):281–286.
- Ohkubo T, Imai Y, Tsuji I, et al. Prediction of mortality by ambulatory blood pressure monitoring versus screening blood pressure measurements: a pilot study in Ohasama. J Hypertens. 1997;15(4):357–364.