Abstract
Purpose
Compared to unattended office blood pressure (uOBP), attended office blood pressure (aOBP) is higher. It is not known, however, to what extent distance between physician and patient influences blood pressure (BP) values.
Materials and methods
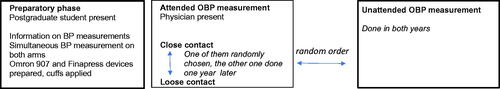
Participants were stable hypertensive patients, followed in the university hospital-based out-patient center. During a session, automated office BP was measured three times after a pre-set five-minute pause, using the Omron 907 device; both aOBP and uOBP were done, in a random order. Simultaneously, beat-to-beat BP measurement was performed using the Finapress device. During aOBP, some participants were in close contact with the physician while others were in loose contact where the doctor was sitting in the room about 2.5 m apart. One year later, the second session with the same protocol was organized, but the close and loose contact were interchanged. The data were analyzed using a paired t-test.
Results
Complete data were collected in 32 patients, baseline uOBP was 122.8 ± 14.8/69.5 ± 11.7 mmHg. Systolic and diastolic aOBP with close contact was higher by 4.6 ± 6.9 and 1.9 ± 3.4 mmHg (p < 0.0007 and 0.0039, respectively), while aOBP with loose contact was not different from uOBP. Beat-to-beat BP increased during aOBP by 6.5 ± 8.5/3.3 ± 4.8 mmHg. The increase persisted during all the three aOBP measurements (p < 0.0001 for all systolic and diastolic BP values); the results were similar for close and loose contact. The peak increase during uOBP was of similar magnitude as during aOBP but it lasted shorter: it reached the significance level of p < 0.0001 only during the first uOBP measurement.
Conclusions
Compared to uOBP, aOBP values were higher with close, but not with loose contact between physician and patient. These differences were, however, not detected by beat-to-beat BP measurement.
Introduction
Automated office blood pressure (BP) measurement which enables to measure BP with patient left alone in the room has been developed during the last 15–20 years [Citation1]. SPRINT has been the first and so far the only large randomized prospective trial where unattended office BP (uOBP) measurement was used [Citation2]. Its results provoked much discussion, mainly about the interpretation of the data and their implementation to clinical practice. When the SPRINT data were matched with previous trials according to ambulatory BP monitoring, the office BP values in SPRINT were much lower [Citation3]. Unattended and attended office blood pressure (aOBP) measurements were compared in numerous studies; while some showed a very large difference – up to 16/8 mmHg [Citation4] – other ones found practically identical values [Citation5].
Strictly taken, uOBP should be done in a separate room, free from noise and with no one passing through. It is difficult to find such space in many clinical centers, and in real-world clinical practice automated BP is often measured with staff member(s) present in the room, who are, however, often busy doing other things and are not concentrated to the BP measurement. In our study, we aimed to evaluate office BP measurements in two situations: (1) the physician is sitting close to the patient, similarly as during BP measurement with auscultatory method and (2) the physician is only present in the room, at a distance more than two meters from the patient. These measurements were compared to uOBP.
Methods
Study participants
Subjects were recruited from out-patient hypertensive center of the Faculty Hospital in Pilsen. The inclusion criteria were age between 40 and 80 years, medically treated hypertension with no change of treatment within the last six months, hemodynamic stability and absence of any severe illness including symptomatic heart failure. Of 40 patients examined at baseline (March 2019), five were not able to attend the second examination (March 2020), and we had to exclude other three patients because we were not able to measure BP by beat-to-beat method. Data on 32 patients who had complete data on both examinations were analyzed.
Study procedures
The study was approved by the Ethics Committee of the Charles University Medical Faculty and Teaching Hospital, and all participants signed informed consent. The sessions were performed in the morning, in a fasting state in a quiet room, with temperature of approximately 22–23 °C (see for schedule). ECG was registered, blood sample was taken, body weight and height were measured, and a standard questionnaire was administered to obtain information on medical history including drug treatment. The postgraduate student in casual clothing (VK) was responsible for the preparations; she gave a detailed information about the study procedures and instructed patient to sit quietly during BP measurements, not to talk, not to use mobile phone, to sit with back supported, not to cross legs and to have feet resting on the floor. BP was then measured simultaneously on both arms using Watch BP tonometer (Microlife AG Swiss Corporation, Widnau, Switzerland) to exclude a possible inter-arm difference. For office BP measurements, the Omron 907 device was used. Simultaneously, beat-to-beat BP was measured with a finger photoplethysmographic device (Finapress Medical Systems BV, Enschede, The Netherlands); it was shown to provide accurate estimate of means and variability of intra-arterial radial BP [Citation6]. The Finapress device was sent to the producer for a regular check-up before the study. The Finapress arm cuff and finger cuffs were placed on the left arm and left mid or ring fingers; the device was then calibrated. The Omron arm cuff was placed on the right arm. Then, the student marked the start on the Finapress and left the room.
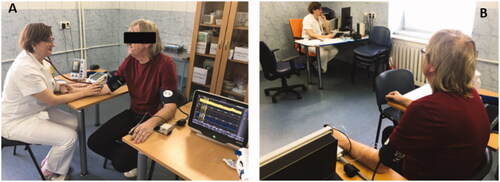
During the BP measurements, the patient was sitting with both forearms on the table (). Office BP was measured with oscillometric method three times after the pre-set five-minute pause with one-minute intervals. During each session, both aOBP and uOBP were measured. For aOBP, the physician in a white coat (JS, JF), other than the one who follows patient regularly, entered the examination room 3 to 4 min after the start of the rest. For uOBP, the patient stayed alone during a five-minute resting period and BP measurement. There were two types of aOBP – (1) with close contact: in order to have standardized distance from the patient, the physician placed the stethoscope to the cubital fossa as if he measured BP with auscultatory method and (2) with loose contact where the doctor was sitting in the room, about 2.5 m apart, and worked on the computer (). In both aOBP types, the physician first came close to the patient, greeted him and introduced himself, but he did not talk to the participant anymore. The order of measurement (attended vs. unattended) was randomized. The session was planned for 90 min, because mainly the preparation and calibration of Finapress measurements lasted long. Its length was the reason why we planned the second session one year later in order to have complete data in all the subjects. During the second session, the type of contact and the order of measurement were reversed, i.e. altogether, each participant had one aOBP measurement with close contact, another one with loose contact and two uOBP measurements.
For each set of BP measurements, five 20-second recordings of beat-to-beat BP were used for analysis. They were defined as follows:
Start: the recording started after the student had marked on the Finapress that the procedure was prepared and left the examination room.
During 1st OBP measurement: five minutes after the start had been marked on the Finapress.
During 2nd OBP measurement: 80 seconds after the end of 20-second recording of the first measurement.
During 3rd OBP measurement: 80 seconds after the end of 20-second recording of the second measurement.
Recovery period: 5 min after the 3rd Omron measurement.
Statistical analysis
SAS 9.4 software (SAS Inc., Cary, NC) was used for analysis. Paired Student’s t-test was used for comparison between different measurements.
Results
Basic characteristics of the sample is shown in . Most of the patients (84%) took at least two antihypertensive drugs, 67% were on hypolipidemic therapy and 41% had diabetes mellitus. shows average office BP values measured using Omron device according to the presence or absence of the physician. The mean difference between aOBP and uOBP was 3.6 ± 7.2 mmHg (p = 0.0002) and 1.9 ± 3.4 mmHg (p = 0.0011) for systolic and diastolic BP, respectively, when all measurements were taken into account. However, when we analyzed separately aOBP with close and with loose contact, only aOBP with close contact was significantly higher in comparison with uOBP values: the differences were 4.6 ± 6.9 mmHg (p = 0.0007) and 1.9 ± 3.4 mmHg (p = 0.0039) for systolic and diastolic BP, respectively. The order of measurements played a role: the difference between aOBP and uOBP was slightly higher when aOBP was performed first. Systolic, but not diastolic aOBP was significantly higher in both years. shows the analysis of beat-to-beat BP with all the measurements included. BP increased during aOBP by up to 6.5 ± 8.5/3.3 ± 4.8 mmHg (corresponding to the 2nd aOBP measurement, p < 0.0001), as compared to baseline BP values (‘start’) measured before the physician entered the office. The increase persisted during all the three aOBP measurements (p < 0.0001 for all systolic and diastolic BP values). The peak increase during uOBP was of similar magnitude as during aOBP (by up to 6.1 ± 5.4/2.0 ± 3.4 mmHg, corresponding to the 1st uOBP measurement, p < 0.0001) but it lasted shorter: it reached the significance level of p < 0.0001 only during the first uOBP measurement. Supplemental Table 1 shows the values of three office BP measurements. They correspond to the BP curves obtained by beat-to-beat measurements (): the three aOBP values were not significantly different from each other – this agrees with the plateau of increased BP values shown in – while during uOBP, the office BP slightly dropped and the third office BP measurement was significantly lower than the first one (p = 0.0032 and 0.045 for systolic and diastolic BP, respectively).
Figure 3. Changes in beat-to-beat systolic and diastolic blood pressure. Values are means ± standard deviation. ***p < 0.0001, **p < 0.001 for difference in BP value from the start BP; calculated using paired t-test.
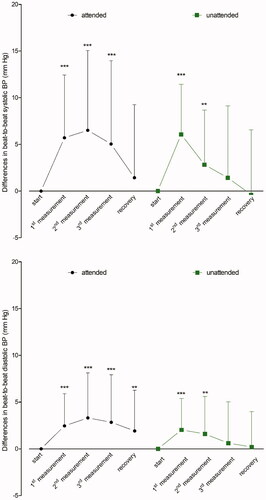
Table 1. Baseline characteristics of the study population.
Table 2. Differences between attended and unattended office blood pressure.
Supplemental Figures 1–3 show changes in beat-to-beat BP according to the type of contact, order of measurement and study visit. They have similar patterns as shown in .
Discussion
To our knowledge, this is the first study designed to investigate the impact of close or loose physician – patient contact during office BP measurement. We found that close contact, compared to uOBP, resulted in significant BP increase, while with loose contact, the BP values were only slightly higher and they did not reach statistically significant difference from uOBP in our relatively small sample.
The office BP changes during different BP measurements were rather small. This was due to several factors: our probands were stable well controlled hypertensive patients, familiar with the staff and premises, followed usually for a long time. The session with uOBP and aOBP measurement was long and this could have diminished the alarm reaction. During aOBP of both types, there was no talking after the formal greeting and no noise, e.g. phone ringing; these conditions, difficult to keep in clinical practice, could also contribute to the small BP reaction.
The strong sides of our work, however, lie in the careful adherence to the study protocol, homogeneity of the study group and random assignment to the type of contact and order of measurement.
In our study, we used the same device and protocol of BP measurement as in SPRINT; this trial is still in the center of debate about uOBP and aOBP. While the 2017 US guidelines for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults changed the definition of hypertension mainly based on the SPRINT results [Citation7], the ESC/ESH guidelines remained more reserved [Citation8]. The reason is that prognostic data based on uOBP are very preliminary [Citation9] and there are no data comparing the prediction of cardiovascular morbidity/mortality by uOBP and classic office BP measurements. After the SPRINT trial had been finished, questionnaires about how BP was measured were sent to the participating centers. The results were heterogeneous across centers [Citation10] and it seems that health care personnel was often present, either during the five-minute pause before the first measurement or during the measurements. In accordance with our results, automated office BP can probably give lower values even in the presence of staff members when the contact is not close.
Beat-to-beat systolic BP increased similarly during aOBP in our study, with no difference between the type of contact, and during uOBP as well (by about 6 mmHg). The only difference against uOBP was that the increase during aOBP lasted longer. Using the same method, a higher increase during aOBP – by 12 mmHg – was observed by Saladini et al. [Citation11], but this study was done in untreated hypertensive subjects. Our results are different from the findings of a recently published study performed in 18 subjects, where the authors showed that beat-to-beat peak systolic BP was 14 mmHg lower during uOBP compared to aOBP [Citation12]. The subjects were, however, newly diagnosed untreated subjects and their mean office BP was 153/102 mmHg while in our group, it was 123/70 mmHg. BP level is known to be a crucial factor determining the BP increase during stress.
In conclusion, despite a relatively small number of subjects and moderate BP changes, we proved that physician’s close proximity to the patient increased office BP; this was not the case when the physician was only present in the room and left the patient undisturbed. This aspect of office BP measurement merits further attention.
Supplemental Material
Download MS Word (14.3 KB)Supplemental Material
Download MS Word (176.5 KB)Supplemental Material
Download MS Word (183.2 KB)Supplemental Material
Download MS Word (176.8 KB)Disclosure statement
The authors report no conflict of interest.
Additional information
Funding
References
- Myers MG, Valdivieso MA. Use of an automated blood pressure recording device, the BpTRU, to reduce the ‘white coat effect’ in routine practice. Am J Hypertens. 2003;6:494–497.
- The SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–2116.
- Parati G, Ochoa JE, Bilo G, et al. SPRINT blood pressure: sprinting back to Smirk's basal blood pressure? Hypertension. 2017;69(1):15–19.
- Filipovsky J, Seidlerova J, Kratochvil Z, et al. Automated compared to manual office blood pressure and to home blood pressure in hypertensive patients. Blood Pressure. 2016;25:228–234.
- Bauer F, Seibert FS, Rohn B, et al. Attended versus unattended blood pressure measurement in a real life setting. Hypertension. 2018;71(2):243–249.
- Parati G, Casadei R, Groppelli A, et al. Comparison of finger and intra-arterial blood pressure monitoring at rest and during laboratory testing. Hypertension. 1989;13(6 Pt 1):647–655.
- Whelton PK, Carey RM, Aronow WS, et al. High blood pressure clinical practice guideline: executive summary. J Am Coll Cardiol. 2018;71(19):2199–2269.
- Williams B, Mancia G, Spiering W, et al. ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953–2041.
- Johnson KC, Whelton PK, Cushman WC, et al. Blood pressure measurement in SPRINT (systolic blood pressure intervention trial). Hypertension. 2018;71(5):848–857.
- Myers MG, Kaczorowski J, Dolovich L, et al. Cardiovascular risk in hypertension in relation to achieved blood pressure using automated office blood pressure measurement. Hypertension. 2016;68(4):866–872.
- Saladini F, Benetti E, Malipiero G, et al. Does home blood pressure allow for a better assessment of the white-coat effect than ambulatory blood pressure? J Hypertens. 2012;30(11):2118–2124.
- Grassi G, Quarti-Trevano F, Seravalle G, et al. Sympathetic neural mechanisms underlying attended and unattended blood pressure measurement. Hypertension. 2021;78(4):1126–1133.