In recent decades, great efforts have been dedicated to the recognition and promotion of women’s health as in the prevention and management of health conditions in women [Citation1–5]. Important initiatives have also been implemented by institutions supporting biomedical research, such as the US National Institutes of Health and the European Commission, to increase the participation of women in the medical sciences and to incorporate more systematically sex (a biological characteristic) and gender (a social construct) analyses into the design of research projects [Citation2,Citation3]. An analysis of more than 1.5 million medical research papers has shown that integrating more women into research projects is associated with greater attention to gender- and sex-related factors in disease-specific research, which should be globally beneficial for women’s health globally [Citation6].
In addition to their gender-specific health problems, women face the same diseases and risk factors that men do. Nonetheless, for a wide range of diseases, there are sex and gender differences that influence this biology, epidemiology, diagnosis, and life trajectory, as discussed recently in the context of hypertension, obesity and diabetes [Citation7]. In addition, gender differences that affect the knowledge and the perception of the disease-associated risk, often lead to health misconceptions and hence to poor screening, insufficient implementation of preventive measures and inadequate global management.
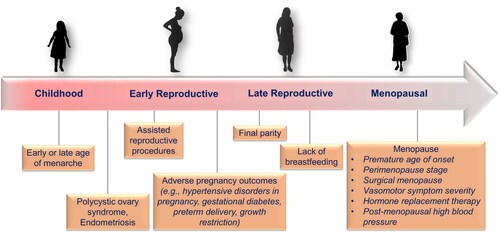
A striking example is the poor recognition on the part of women that cardiovascular diseases (CVD) are the leading cause of death in both genders, not exclusively in men. Several surveys have reported that knowledge and risk perception of CVD is low among women, in particular among those below the age of 35 [Citation8–11]. Interestingly, awareness of the CVD risk of American women nearly doubled between 1997 and 2009 (from 30 to 54%) [Citation10], but awareness of the presence of established heart disease subsequently declined from 65% in 2009 to 44% in 20198. This trend contrasts with observations reporting increases in hospitalisations for myocardial infarction among women aged 25–34 and a lack of reduction of CVD mortality rate in women aged 35 to 54 in the US, whereas it did decrease in older women [Citation12]. There are several possible explanations for the low CVD awareness in women. One of them may be the widespread opinion that CVD mainly affects men. In an Italian survey, more than 60% of women considered CVD as an almost exclusively male condition [Citation9]. Another reason may be that women rightly consider themselves as belonging to a low cardiovascular risk group until menopause and that CVD risk factors can easily be handled. Therefore, their fears are focused on the risk of cancer, especially breast cancer, which they identify wrongly as their leading cause of death [Citation8]. In addition, a large proportion of women, especially younger ones, are not conscious of their level of CVD risk because their risk factors have not been assessed [Citation4]. This is particularly common among women belonging to a minority or to low socioeconomic class [Citation13]. Another important aspect is that most women who develop sex-specific medical events (hypertensive disorders of pregnancy, polycystic ovary syndrome, assisted reproductive procedures) are not aware that their reproductive history might significantly impact their long-term cardiovascular health [Citation11,Citation14,Citation15] and that the menopause transition represents a period of accelerated CVD risk associated with an increase in blood pressure (). One important point could also be women’s life perspective at a younger age since at that period their life focus is their family, especially small children. A lot of housekeeping problems occupy their mind and no time is left for self-care.
Figure 1. Women’s life trajectory and clinical situations possibly affecting their cardiovascular risk.
Another critical issue is the low participation of women in clinical trials of cardiovascular disease treatment developments, which sometimes raises questions regarding the validity and the application of the conclusions of new findings to women. Indeed, despite repeated international recommendations, the involvement of women in CVD trials remains insufficient. In an analysis of 300 randomised control trials (RCT) conducted in various disease areas, the median enrolment rate of women was 41% and even lower in ischaemic heart disease (22%) or hypertension trials (38%) [Citation16]. In trials such as SPRINT in hypertension [Citation17] or major RCTs demonstrating the clinical benefits of SGLT2 inhibitors [Citation18,Citation19] or finerenone [Citation20], the proportion of participating women was 30–35%, despite the fact that mean age ranged between 58 and 68 in these trials. This is an age where the prevalence of these diseases is comparable in males and females. There is no clear explanation for this gap except that females may perhaps be more reluctant than males to participate in trials or that they may perceive more harm from trial participation.
Under-representation of women in clinical trials may also affect the management of women with CVD. For example, hypertension guidelines do not recommend the sex-specific diagnosis, treatment and follow-up strategies. Yet, it is well known that there are significant sex- and gender-related differences in the regulation of BP [Citation21,Citation22], as well as in hypertension prevalence, clinical manifestations, effects of therapy and incidence and perception of adverse effects. Moreover, the association between hypertension and cardiovascular outcomes differs between males and females. In this respect, a recent analysis of 27,542 persons (54% women) without baseline CVD who had standardised systolic BP measurements performed in 1 of 4 previously published community-based cohort studies, suggested that the risk of developing cardiovascular disease, including myocardial infarction and stroke, was associated with BP elevations from lower ranges in women compared with men [Citation23]. As concluded by the authors, this observation could suggest a need for a lower sex-specific definition of optimal SBP for women. Similarly, a posthoc analysis of SPRINT has questioned the benefits of more intensive lowering of BP in women, as a significant reduction of the primary composite cardiovascular outcome was found in men (−27%) but not in women (−16%) when analysing data separately in men and women [Citation24]. Statistical issues may have been responsible for the lack of benefit in women (e.g. insufficient power), but other major differences have been reported that could have accounted for the difference in clinical benefit, mainly a worse profile of CVD risk factors in men.
As discussed by Delles and Currie [Citation25], these new analyses reveal that the binary approach that is regularly used to assess the sex effects of interventions is probably insufficient, as it does not capture the male and female-specific conditions. Lastly, one should perhaps be more sensitive to the fact that there is sexual dimorphism in the pharmacology of antihypertensive drugs and the risk of developing drug-related adverse reactions [Citation26]. A Polish survey conducted on 1000 treated hypertensive patients showed that the frequency of reported adverse drug-induced symptoms was significantly higher in females (54%) than in male patients (41%), even though females were taking significantly fewer drugs [Citation27]. This study, like many others before, confirms the sex and gender-specific differences in drug tolerability and safety further emphasising the need for closer attention in the prescription of drugs (which often differs in women and men), and in the monitoring of adverse reactions during follow-up.
In recent years, there has been a proliferation of publications asking for a change in the way one addresses women’s health. Major improvements have occurred in the development of sex-specific scientific knowledge, but the gender approach remains often ignored. This is illustrated in a recent review that analysed international and selected national guidelines for the management of hypertension representing all continents [Citation28]. The purpose of this review was to underline between-guideline similarities and differences in epidemiology, diagnosis, and treatment of hypertension in men and women. This interesting review reveals that all guidelines essentially focus on sex-specific aspects and cover mainly hypertensive disorders of pregnancy and, to a lesser extent, contraception and contra-indications to antihypertensive drugs. Is it reasonable to confine women’s life trajectory in hypertension to these events? Certainly not. There is an urgent need to modify our perspective to give more consideration to gender aspects, including social and behavioural factors, beliefs and specific needs and use and access to health care. Because of the low involvement of women in trials, other sources of information such as real-world data from large registries should be explored. For example, in Sweden, a real-world analysis of primary care data has found that women had higher BP, less treatment and worse BP control than men, and the female sex was a significant predictor of less intensive antihypertensive treatment [Citation29]. This finding is the reverse of what was found in population-based studies in the same country, probably because not all age categories were considered in some studies. Today we do not need sex-specific guidelines, but the format of guidelines should likely be modified in order to provide more specific information on women, considering their entire life trajectory and gender-specific ways of preventing hypertension and CVD. We must continue to work for more health equity that begins with increased recognition of the specific situations and needs of women.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Wenger NK, Lloyd-Jones DM, Elkind MSV, et al. Call to action for cardiovascular disease in women: epidemiology, awareness, access, and delivery of equitable health care: a presidential advisory from the American heart association. Circulation. 2022;145:1–4.
- Accounting for sex and gender makes for better science. Nature. 2020;588:196.
- Arnegard ME, Whitten LA, Hunter C, et al. Sex as a biological variable: a 5-year progress report and call to action. J Womens Health. 2020;29:858–864.
- Gooding HC, Brown CA, Liu J, et al. Will teens go red? Low cardiovascular disease awareness among young women. J Am Heart Assoc. 2019;8:e011195.
- Gerdts E, Sudano I, Brouwers S, et al. Sex differences in arterial hypertension. Eur Heart J. 2022;43:4777–4788.
- Nielsen MW, Andersen JP, Schiebinger L, et al. One and a half million medical papers reveal a link between author gender and attention to gender and sex analysis. Nat Hum Behav. 2017;1:791–796.
- Regensteiner JG, Reusch JEB. Sex differences in cardiovascular consequences of hypertension, obesity, and diabetes: JACC focus seminar 4/7. J Am Coll Cardiol. 2022;79:1492–1505.
- Cushman M, Shay CM, Howard VJ, et al. Ten-Year differences in women’s awareness related to coronary heart disease: results of the 2019 American heart association national survey: a special report from the American heart association. Circulation. 2021;143:e239–e248.
- Maffei S, Meloni A, Deidda M, Igenda Study G, et al. Cardiovascular risk perception and knowledge among italian women: lessons from IGENDA protocol. J Clin Med. 2022;11(6):1695.
- Mosca L, Mochari-Greenberger H, Dolor RJ, et al. Twelve-year follow-up of American women’s awareness of cardiovascular disease risk and barriers to heart health. Circ Cardiovasc Qual Outcomes. 2010;3:120–127.
- Beussink-Nelson L, Baldridge AS, Hibler E, et al. Knowledge and perception of cardiovascular disease risk in women of reproductive age. Am J Prev Cardiol. 2022;11:100364.
- Arora S, Stouffer GA, Kucharska-Newton AM, et al. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation. 2019;139:1047–1056.
- Brown RM, Tamazi S, Weinberg CR, et al. Racial disparities in cardiovascular risk and cardiovascular care in women. Curr Cardiol Rep. 2022;24:1197–1208.
- O'Kelly AC, Michos ED, Shufelt CL, et al. Pregnancy and reproductive risk factors for cardiovascular disease in women. Circ Res. 2022;130:652–672.
- Davis GK, Henry A, Arnott C, et al. The long-term cardiovascular impact of hypertension in pregnancy – a missed opportunity. Austr N Z J Obstetr Gynaecol. 2021;61:474–477.
- Daitch V, Turjeman A, Poran I, et al. Underrepresentation of women in randomized controlled trials: a systematic review and meta-analysis. Trials. 2022;23:1038.
- Group SR, Wright JT, Jr., Williamson JD, et al. A randomized trial of intensive versus standard Blood-Pressure control. N Engl J Med. 2015;373:2103–2116.
- Bhattarai M, Salih M, Regmi M, et al. Association of sodium-glucose cotransporter 2 inhibitors with cardiovascular outcomes in patients with type 2 diabetes and other risk factors for cardiovascular disease: a meta-analysis. JAMA Netw Open. 2022;5:e2142078.
- Razuk V, Chiarito M, Cao D, et al. SGLT-2 inhibitors and cardiovascular outcomes in patients with and without a history of heart failure: a systematic review and meta-analysis. Eur Heart J Cardiovasc Pharmacother. 2022;8:557–567.
- Agarwal R, Filippatos G, Pitt B, et al. Cardiovascular and kidney outcomes with finerenone in patients with type 2 diabetes and chronic kidney disease: the FIDELITY pooled analysis. Eur Heart J. 2022;43:474–484.
- Reckelhoff JF. Mechanisms of sex and gender differences in hypertension. J Hum Hypertens. 2023; 16:1–6.
- Barris CT, Faulkner JL, Belin de Chantemèle EJ. Salt sensitivity of blood pressure in women. Hypertension. 2023;80(2):268–278.
- Ji H, Niiranen TJ, Rader F, et al. Sex differences in blood pressure associations with cardiovascular outcomes. Circulation. 2021;143:761–763.
- Foy CG, Lovato LC, Vitolins MZ, et al. Gender, blood pressure, and cardiovascular and renal outcomes in adults with hypertension from the systolic blood pressure intervention trial. J Hypertens. 2018;36:904–915.
- Delles C, Currie G. Sex differences in hypertension and other cardiovascular diseases. J Hypertens. 2018;36:768–770.
- Cífková R, Strilchuk L. Sex differences in hypertension. Do we Need a Sex-Specific Guideline? Front Cardiovasc Med. 2022;9:960336.
- Polaczyk M, Olszanecka A, Wojciechowska W, et al. The occurrence of drug-induced side effects in women and men with arterial hypertension and comorbidities. Kardiol Pol. 2022;80:1094–1103.
- Meinert F, Thomopoulos C, Kreutz R. Sex and gender in hypertension guidelines. J Hum Hypertens. 2023;10:1–8.
- Bager JE, Manhem K, Andersson T, et al. Hypertension: sex-related differences in drug treatment, prevalence and blood pressure control in primary care. J Hum Hypertens. 2023;27(3):176–181.
