Abstract
Purpose
To share a Latin-American perspective of the use of telemedicine, together with blood pressure measurements outside the medical office, as a potential contribution to improving access to the health system, diagnosis, adherence, and persistence in hypertension treatment.
Material and methods
A document settled by a Writing Group of Mexico Hypertension Experts Group, Interamerican Society of Hypertension, Epidemiology and Cardiovascular Prevention Council of the Interamerican Society of Cardiology, and National Cardiologist Association of Mexico
Results
In almost all Latin American countries, the health sector faces two fundamental challenges: (1) ensure equitable access to quality care services in a growing population that faces an increase in the prevalence of chronic diseases, and (2) optimise the growing costs of health services, maintaining equity, accessibility, universality, and quality. Telehealth proposes an innovative approach to patient management, especially for chronic conditions, intending to provide remote consultation, education, and follow-up to achieve measurements and goals. It is a tool that promises to improve access, empower the patient, and somehow influence their behaviour about lifestyle changes, improving prevention and reducing complications of hypertension. The clinical practitioner has seen increased evidence that the use of out-of-office blood pressure (BP) measurement and telemedicine are helpful tools to keep patients and physicians in contact and promote better pharmacological adherence and BP control. A survey carried out by medical and scientific institutions showed that practitioners are up-to-date with telemedicine, had internet access, and had hardware availability.
Conclusions
A transcendent issue is the need to make the population aware of the benefits of taking blood pressure to avoid complications of hypertension, and in this scenario, promote the creation of teleconsultation mechanisms for the follow-up of patients diagnosed with hypertension.
PLAIN LANGUAGE SUMMARY
What is the context?
In almost all Latin American countries, the health sector faces two fundamental challenges: (1) ensure equitable access to quality care services in a growing population that faces an increase in the prevalence of chronic diseases, and (2) optimise the growing costs of health services, maintaining equity, accessibility, universality, and quality.
What is new?
Telehealth proposes an innovative approach to patient management, especially for chronic conditions, intending to provide remote consultation, education, and follow-up to achieve measurements and goals. It is a tool that promises to improve access, empower the patient, and somehow influence their behaviour about lifestyle changes, improving prevention and reducing complications of hypertension.
What is the impact?
Needs are always infinite, and resources are finite, so according to the World Health Organisation (WHO), advances in electronic, information, and communication technology point to more significant equity in the provision of services, considering the effectiveness, possibility of refining the rationalisation of health spending, and improving health care for remote populations.
A transcendent issue is the need to make the population aware of the benefits of taking blood pressure to avoid complications of hypertension, and in this scenario, promote the creation of teleconsultation mechanisms for the follow-up of patients diagnosed with hypertension.
Hypertension, a public health challenge
Despite having made extraordinary efforts to improve the diagnosis, treatment, and control of patients living with hypertension (Hyp), the accumulated experience shows that in the best case scenario, only 50% of them receive treatment, and half of the treated patients achieve therapeutic goals [Citation1–3].
The 2021 annual global screening campaign named May Measurement Month (MMM) screened 156,513 American subjects, 60,475 (38.6%) were classified as hypertensive, of whom 72.9% were aware, and 59.5% were on antihypertensive medication. Of those on treatment, 55% had controlled BP (32.7% of all hypertensive participants) [Citation4]. Awareness (76.7%), treatment (70.6%), control rates (60.9%) and proportion of all hypertensive participants controlled (43%) were lower than those reported in MMM campaigns before the COVID-19 pandemic [Citation2].
Cohort studies monitoring the treatment of patients with Hyp are based on measurements made at the office; however, ambulatory blood pressure monitoring (ABPM) and home blood pressure monitoring (HBPM) show greater certainty of conclusion [Citation5,Citation6]. Staplin et al. aimed to examine associations of clinic and 24-h ambulatory blood pressure with all-cause and cardiovascular mortality from the database of 59,124 subjects of the Spanish Ambulatory Blood Pressure Registry. After adjustment for clinic blood pressure, 24-h blood pressure remained strongly associated with all-cause deaths (HR 1.43; 95% CI 1.37-1.49). Night-time blood pressure, was more informative about the risk of all-cause death (591%) and cardiovascular death (604%) than clinic blood pressure [Citation7].
The use of Telemedicine, together with blood pressure measurements outside the medical office, could contribute to improving access to the health system, diagnosis, adherence, and persistence in Hyp treatment. The introduction of blood pressure telemonitoring systems could enhance routine screening and management of chronic conditions such as hypertension and as a consequence could reduce the adverse impact on global burden of disease in Latin America.
Telemedicine expectations
The twenty first century is marked by significant improvements in information technology, and one of the most favoured areas has been the new information and communication technologies in health (NICTs). The concept of ‘e-Health’ describes the combined use of information and communication technologies to transmit, store and retrieve data for clinical, administrative, and educational purposes, both locally and remotely, generating direct interaction with public health experts and thereby stimulating health policies in favour of the population [Citation8].
E-Health includes Telemedicine, defined according to the American Telemedicine Association as ‘the exchange of medical information from one site to another through electronic communications to improve the health status of patients’. E-Health proposes an innovative approach to patient management, especially for chronic conditions, intending to provide remote consultation, education, and follow-up to achieve measurements and goals. It is a tool that promises to improve access, empower the patient, and somehow influence their behaviour about lifestyle changes, improving prevention and reducing complications [Citation9]. Needs are always infinite, and resources are finite, so according to the World Health Organisation (WHO), advances in electronic, information, and communication technology point to more significant equity in the provision of services, considering the effectiveness, possibility of refining the rationalisation of health spending, and improving health care for remote populations [Citation10].
Telemedicine opportunities
New applications (apps) are designed to evaluate and propose the actions to be taken by the GP to adequately manage the hypertensive population, with promising expectations for the Latin American population [Citation11–14]. Substantial evidence suggests that there is a significant reduction in blood pressure values over time and an essential impact on empowerment, attitudes, and self-management behaviours in patients with Hyp by implementing these apps. Through the modality of Telemedicine in countries with medium-low economic resources, including those in Latin America, an improvement in blood pressure values has been shown, reaching goals even in rural areas with difficult access to communication networks. In addition, an improvement in the health status of patients with Hyp has been achieved by sending text messages and support materials for the control of blood pressure [Citation15–18].
In recent years, the clinical practitioner has seen increased evidence that the use of out-of-office BP measurement is a helpful tool to keep patients and physicians in contact and promote better pharmacological adherence and BP control [Citation19,Citation20]. Another advantage is that self-measured blood pressure data can be shared with physicians and managed by Telemedicine, which is a valuable tool for the Hyp clinical approach. Health practitioners now have a vast number of systematic reviews and meta-analyses confirming the utility of these applications [Citation8,Citation21–27].
The basis of Telemedicine are the concepts of health parameters, biological signals acquisition and remote management by healthcare providers. Internet is the most common way to deliver these services, and a close and secure e-health system used by trained professionals is essential to privacy guarantee [Citation8,Citation28]. Another critical value of self-measured BP supported by artificial intelligence platforms is the opportunity to build robust databases with the possibility to answer questions related to out of office BP behaviour as well as BP phenotypes [Citation29]. These tools and data have been of enormous value in reviewing traditional home BP concepts and redefining parameters concerning goals and treatment efficacy.
Issues for the application of telemedicine in Hyp management in Latin America
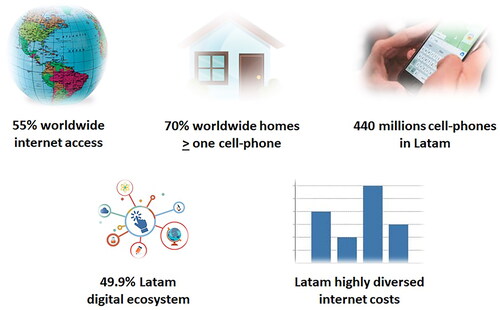
In the year 2020, more than 55% of the world population had access to the Internet, and in 7 out of 10 homes there was at least one cell phone. Therefore, we can conclude that NICTs have played a preponderant role in the countries’ different industrial, commercial, economic, and health development areas. In Latin America, there are still considerable differences in access to health services due to various factors that limit the possibility of receiving timely and quality medical care (). Among these factors are the lack of health policies, the scarcity of resources in technological infrastructure, low levels of income for professionals, the overpopulation of specialists in large cities, large geographical extensions, and sociocultural aspects of the populations [Citation30]. In almost all Latin American countries, the health sector faces two fundamental challenges:
Ensure equitable access to quality care services in a growing population that faces an increase in the prevalence of chronic diseases.
Optimise the growing costs of health services, maintaining equity, accessibility, universality, and quality.
The truth is that Latin American countries are adopting NICTs, either as technological innovation, as an anti-crisis measure in collapsed health systems, or because they are considered as powerful support tools for modern medicine, capable of acquiring, storing and automating processes, but that can never replace the empathic, critical and analytical sense that every doctor must have, and that quality care requires. A deep ethical-moral debate must occur before introducing these disruptive technologies in the doctor-patient relationship, where face-to-face and physical contact seem ideal but do not always necessarily are favourable and cost-effective actions. Between 2005 and 2016, in countries with investments in remote public care, there have been outstanding results, with rates of 70-80% of avoided transfers of patients to specialised or more complex health centres, savings of 10-15% in the municipal health budget, and more than 10 million second opinions on electrocardiograms and imaging tests [Citation31]. In many countries of the region, the developments in digital health enabled the ministries of health to include Telemedicine in their agenda as a support element for processes, regulations, policies, and essential administrative changes that allow for the adoption of new digital technologies [Citation32]. Already at the beginning of this millennium, some studies glimpsed at the possible benefits of Telemedicine to facilitate the development of public policies and improvements to health systems. Among the advantages were access to information, providing services traditionally supplied via face-to-face, educational strengthening, quality control of detection programs, and reduced health care costs. However, some concerns may have acted as barriers to accelerating Telemedicine, such as the possible breakdown of the doctor-patient and interprofessional relationship, loss of the quality of care, lack of regulatory considerations, and reduced accuracy of the records in clinical charts. Most telemedicine interventions have been developed with a primarily technical approach, assuming that key players and stakeholders would accept them ‘by default’. This approach often underestimated relevant issues such as digital literacy, talent creation, and digital culture. So far, telemedicine has been approached in the same way as the traditional practice of medicine, centreing on the perspective of health professionals or service providers, and reducing the focus in the perspective of patients, especially those who are disconnected or less digitally literate [Citation33]. In the future, more attention should be paid to friendliness of the applications, portability (focus on mobile devices, with integrated functionalities), and healthcare workflows, generating pre- and post-in-person digital experiences.
Implementing Telemedicine initiatives taking into account the social, cultural, technical, political, and economic aspects is a big challenge without government support, an intersectoral approach, and transdisciplinary actions. The main critical success factors include developing technical frameworks for action based on international standards, achieving trained health workers, and digitally literate health users. Robust governance requires the incorporation of specialised networks and a group of experts for developing implementation plans, facilitating information, experiences, training, monitoring, and evaluation of programs, and generating containment actions in unexpected changes. The actors involved could document the work processes from macro to micromanagement through clinical practice guidelines, policies, procedures, and similar documents so that those leading the teams work with a shared and proper understanding of the defined telemedicine programs.
Barriers to implementing telemedicine services in Latin America should be considered, such as lack of telehealth licences, patient privacy and confidentiality, data accuracy and misdiagnosis, provider-patient relationship conditions, medical responsibilities, fraud and abuse risks, treatment prescriptions, and reimbursement determination [Citation34]. In addition, Telemedicine services can provide benefits in different scenarios, which must be systematically reviewed, such as in patients with chronic kidney disease, pregnant women, subjects over 80 years of age, resistant hypertension, or in childhood [Citation20]. A controlled clinical trial with a 12-month follow-up in Argentina, Guatemala, and Peru was conducted which included pre-hypertensive individuals under 60 years of age who were not receiving pharmacological treatment, and had monthly telephone calls focused on lifestyle change. This trial showed a reduction in sustained SBP and DBP figures, 0.31 to 1.13 mm Hg and 0.01 to 0.45 mm Hg, respectively [Citation35].
Latin American practitioners’ survey on Telemedicine
A survey carried out by medical and scientific institutions with high representation in Latin America included almost 1,800 professionals from the region and it showed two very important findings. First, they are up-to-date with Telemedicine. Among these professionals, 40.7% have a specialty in cardiology and 14% are interns. In 82.5% of the cases interns regularly receive scientific journals, and in 73.4% of the cases, they carry out academic activities regularly with universities or scientific societies. Second, the fact that 98% of the sample had internet access, and 90.5% had hardware availability proves they are well connected from a technological perspective. The survey revealed that 50.9% of responders considered telemonitoring a highly important consultation complement and 64.1% considered it was precious to improve patient compliance. Out of the total, 43.6% of practitioners are currently conducting telemonitoring, and at the same time, 62% of the surveyed physicians answered that they needed telemonitoring training. Only 10.8% of the doctors thought that patients would prefer telemonitoring to face-to-face consultation, and 16% did not plan to implement these technologies. Around 48.5% of the sample demonstrated an excellent predisposition to control patients with this modality of medical assistance. Higher interest in telemonitoring is related to younger age, medical specialty, team working, residence in the biggest cities, and a more reasonable expectation towards Telemedicine and reimbursement.
Remote monitoring is feasible in Latin America. Specialists and general practitioners, especially living in bigger cities, seem eager and are self-perceived as well-trained and experienced. Facilities and resources do not seem to be a challenge but reinforcing training and promoting telemedicine are more necessary to those health providers who are less motivated [Citation36].
The challenges
Telemedicine has a significant potential to benefit patients with chronic non-communicable diseases such as Hyp, but regulatory and legal aspects must be covered according to international, national, and regional standards [Citation37].
The World Medical Association Statement on the Ethics of Telemedicine was adopted by the 58th General Assembly of the World Medical Association, in Copenhagen, Denmark, in October 2007 and was later amended by its 69th General Assembly in Reykjavik, Iceland, in October 2018 [Citation36]. In most countries, exponential growth in the use of Telemedicine during the COVID-19 pandemic occurred without adequate planning, defined ethical and legal guidelines, and tools to evaluate the results or established quality standards. Telemedicine involves multiple administrative, legal, ethical, economic, political, and philosophical aspects. The aspects required are the ethics code, data protection, privacy and confidentiality, and regulatory aspects (legal framework). Since multiple studies have shown better control of patients with Hyp and other chronic diseases with the use of Telemedicine, it is an excellent area of opportunity in low- and middle-income countries in Latin America, so it is urgent to establish the legal and ethical framework that ensures implementation throughout the region [Citation38,Citation39].
There has been a decline in the educational level in many Latin American countries in recent decades. This issue could challenge the massive involvement of the population in Telemedicine due to Intellectual barriers which implies in many cases the inability to understand slogans and messages adequately [Citation40].
Potential disadvantages of telemedicine
Some patients may feel more emotionally contained with office visit to develop the patient–physician relationship, challenging personal connections.
Other potential disadvantages of telemedicine could include an inability to examine the patient when a physical exam is needed which could hinder accurate diagnosis and treatment.
Visits could be briefer than in-person what can give the sense of being rushed, and therefore, some concerns could emerge that the telehealth environment may reduce physician attention on patient needs.
On the other hand, telehealth could inhibit patient personal expression.
Other challenges include lower use of technology among older adults and co-morbidities as hearing, visual, or cognitive impairment [Citation41,Citation42].
Telemedicine and scientific societies
Academic organisations should promote massive training campaigns and medical education of validated and calibrated equipment to achieve a correct measurement of blood pressure and proper interpretation of the results for both primary care physicians and the community, thus favouring the culture of timely detection of Hyp. Promoting communication technologies, including equipment with automatic connectivity, and creating data monitoring centres and advice or feedback to users is essential. Scientific societies should promote the creation of national Hyp registries that allow epidemiological information to be obtained and establish strategies to avoid Hyp complications. A transcendent issue is the need to make the population aware of the benefits of taking blood pressure to avoid complications of Hyp, and in this scenario, promote the creation of teleconsultation mechanisms for the follow-up of patients diagnosed with Hyp.
Telemedicine is a fertile ground in Latin America, although educational improvement and technological development are still matters to be resolved. Therefore, human resources must be considered when implementing a telemedicine service. A complete training plan must be established including all the skills and knowledge that the work team needs to carry out its task (all the communication, ethical, technical, and health aspects that comprise it), an improvement strategy, and all the necessary professional-level education and certification appropriate for the development and provision of the telemedicine service.
Having a continuing medical education agenda with training programs is a must, together with the academic certification that endorses the training of the health teams.
Online courses should include topics such as information technology and telecommunications, Telemedicine and telehealth, primary health care, as well as legal, medical, epidemiological, technological, and maintenance updates, whose certificates delivered and endorsed by the university, will be an incentive to participation [Citation43]. Having a continuing medical education agenda with training programs is a must, together with the academic certification that endorses the training of the health teams.
Likewise, it is critical to plan for programs that promote and guide epidemiological and clinical research processes, and the formulation, execution, and development of policies, initiatives, and actions that contribute to equity in prevention and health care, as well as to deliver the system information and determination of indicators on the health situation of the community.
Scientific societies and stakeholders should be aware of devices, apps and platforms features to properly advise users. Home blood pressure monitors requirements include availability of a remote sensor unit of a web-based telemedicine service and memory in case of transmission failure, while the apps and platforms must hold a certification as ‘Software as a Medical Device’, automatic and manual functions to forward data, and bidirectional connection capability with the possibility of establishing immediate doctor-patient interaction [Citation44].
Final comments
Recently, more than 1,100 world opinion leaders had raised their concerns on artificial intelligence (AI) at the World Government Summit in Dubai, United Arab Emirates. In a document published at the website Future of Life, named ‘FLI Open Letter: Pause Giant AI Experiments’, they proposed to stop research on AI systems more powerful than GPT-4 during six months to improve the rules that establish limits to their development. Consequently, certain fears arise about the appropriate use and potential deviations of AI systems with human-competitive intelligence that can pose profound risks to society and humanity [Citation45].
This Writing Group composed by the Mexico Hypertension Experts Group, the Interamerican Society of Hypertension, the Epidemiology and Cardiovascular Prevention Council of the Interamerican Society of Cardiology, and the National Cardiologist Association of Mexico propose in the scenario previously described:
Scientific societies should lead the way towards the implementation of traditional health systems complemented by e-health and healthcare professional’s education and training.
Government agencies must ensure accessibility and equity in access to e-health systems and platforms security and confidentiality.
Stakeholders and funders must accept the relevance of e-health and assume their role as facilitators and supporters of its development.
Non-governmental organisations and patient organisations can contribute to e-health education and dissemination, and at the same time, demanding the preservation of the affective, legal, and ethical aspects of the doctor-patient relationship.
Disclosure statement
The authors report there are no competing interests to declare.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Alcocer L, López A, Borrayo Sánchez H, et al. Hypertension as a persistent public health problem. A position paper from alliance for a healthy heart, Mexico. Ann Clin Hypertens. 2019;3(1):1–9. doi: 10.29328/journal.ach.1001015.
- Poulter NR, Borghi C, Damasceno A, et al. May measurement month 2019: results of blood pressure screening from 47 countries. Eur Heart J Suppl. 2021;23(Suppl B):B1–B5. doi: 10.1093/eurheartj/suab014.
- Chow CK, Teo KK, Rangarajan S, Yusuf S; PURE (Prospective Urban Rural Epidemiology) Study investigators, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, Middle-, and low-income countries. JAMA. 2013;310(9):959–968. doi: 10.1001/jama.2013.184182.
- Beaney T, Wang W, Schlaich MP; MMM Investigators, et al. Global blood pressure screening during the COVID-19 pandemic: results from the may measurement month 2021 campaign. J Hypertens. 2023;41(9):1446–1455. doi: 10.1097/HJH.0000000000003488.
- Oseguera HG, Peralta MR, Muñoz JME. ANCAM group for HBPM. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control in Mexico. Ann Clin Hypertens. 2018;2:17–23.
- Stergiou GS, Palatini P, Parati G ; European Society of Hypertension Council and the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability, et al. 2021 European society of hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39(7):1293–1302. doi: 10.1097/HJH.0000000000002843.
- Staplin N, de la Sierra A, Ruilope LM, et al. Relationship between clinic and ambulatory blood pressure and mortality: an observational cohort study in 59 124 patients. Lancet. 2023;401(10393):2041–2050. doi: 10.1016/S0140-6736(23)00733-X.
- Parati G, Dolan E, McManus RJ, et al. Home blood pressure telemonitoring in the 21st century. J Clin Hypertens (Greenwich). 2018;20(7):1128–1132. doi: 10.1111/jch.13305.
- Omboni S, McManus RJ, Bosworth HB, et al. Evidence and recommendations on the use of telemedicine for the management of arterial hypertension. Hypertension. 2020;76(5):1368–1383. doi: 10.1161/HYPERTENSIONAHA.120.15873.
- World Health Organization. Monitoring and evaluating digital health interventions. A practical guide to conducting research and assessment. 2016. Available from: https://apps.who.int/iris/bitstream/handle/10665/252183/9789241511766-eng.pdf;jsessionid=B7457633E61BAB49A91CF9939267525B?sequence=1
- Tsoi K, Yiu K, Lee H; HOPE Asia Network, et al. Applications of artificial intelligence for hypertension management. J Clin Hypertens (Greenwich). 2021;23(3):568–574. doi: 10.1111/jch.14180.
- Hare AJ, Chokshi N, Adusumalli S. Novel digital technologies for blood pressure monitoring and hypertension management. Curr Cardiovasc Risk Rep. 2021;15(8):11. doi: 10.1007/s12170-021-00672-w.
- Santo K, Redfern J. The potential of mHealth applications in improving resistant hypertension self-assessment, treatment and control. Curr Hypertens Rep. 2019;21(10):81. doi: 10.1007/s11906-019-0986-z.
- Chandler J, Sox L, Kellam K, et al. Impact of a culturally tailored mHealth medication regimen self-management program upon blood pressure among hypertensive hispanic adults. Int J Environ Res Public Health. 2019;16(7):1226. doi: 10.3390/ijerph16071226.
- Piette JD, Marinec N, Janda K, et al. Structured caregiver feedback enhances engagement and impact of mobile health support: a randomized trial in a Lower-middle-income country. Telemed J E Health. 2016;22(4):261–268. doi: 10.1089/tmj.2015.0099.
- Piette JD, Marinec N, Gallegos-Cabriales EC, et al. Spanish-speaking patients’ engagement in interactive voice response (IVR) support calls for chronic disease self-management: data from three countries. J Telemed Telecare. 2013;19(2):89–94. doi: 10.1177/1357633x13476234.
- Gonzalez C, Early J, Gordon-Dseagu V, et al. Promoting culturally tailored mHealth: a scoping review of mobile health interventions in latinx communities. J Immigr Minor Health. 2021;23(5):1065–1077. doi: 10.1007/s10903-021-01209-4.
- Hoffer-Hawlik M, Moran A, Zerihun L, et al. Telemedicine interventions for hypertension management in low- and Middle-income countries: a scoping review. PLoS One. 2021;16(7):e0254222. doi: 10.1371/journal.pone.0254222.
- McManus RJ, Mant J, Franssen M; TASMINH4 Investigators, et al. Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): an unmasked randomised controlled trial. Lancet. 2018;391(10124):949–959. doi: 10.1016/S0140-6736(18)30309-X.
- Souza WK, Jardim PC, Brito LP, et al. Self-measurement of blood pressure for control of blood pressure levels and adherence to treatment. Arq Bras Cardiol. 2012;98(2):167–174. doi: 10.1590/s0066-782x2012005000010.
- Niznik JD, He H, Kane-Gill SL. Impact of clinical pharmacist services delivered via telemedicine in the outpatient or ambulatory care setting: a systematic review. Res Social Adm Pharm. 2018;14(8):707–717. doi: 10.1016/j.sapharm.2017.10.011.
- Xiong S, Berkhouse H, Schooler M, et al. Effectiveness of mHealth interventions in improving medication adherence among people with hypertension: a systematic review. Curr Hypertens Rep. 2018;20(10):86. doi: 10.1007/s11906-018-0886-7.
- Ma Y, Cheng HY, Cheng L, et al. The effectiveness of electronic health interventions on blood pressure control, self-care behavioral outcomes and psychosocial well-being in patients with hypertension: a systematic review and meta-analysis. Int J Nurs Stud. 2019;92:27–46. doi: 10.1016/j.ijnurstu.2018.11.007.
- Lu X, Yang H, Xia X, et al. Interactive mobile health intervention and blood pressure management in adults. Hypertension. 2019;74(3):697–704. doi: 10.1161/HYPERTENSIONAHA.119.13273.
- Omboni S, Tenti M, Coronetti C. Physician-pharmacist collaborative practice and telehealth may transform hypertension management. J Hum Hypertens. 2019;33(3):177–187. doi: 10.1038/s41371-018-0147-x.
- Alessa T, Hawley MS, Hock ES, et al. Smartphone apps to support self-management of hypertension: review and content analysis. JMIR Mhealth Uhealth. 2019;7(5):e13645. doi: 10.2196/13645.
- Luo L, Ye M, Tan J, et al. Telehealth for the management of blood pressure in patients with chronic kidney disease: a systematic review. J Telemed Telecare. 2019;25(2):80–92. doi: 10.1177/1357633X17743276.
- Omboni S. Connected health in hypertension management. Front Cardiovasc Med. 2019;6:76. doi: 10.3389/fcvm.2019.00076.
- Barroso WKS, Feitosa ADM, Barbosa ECD, et al. Prevalence of masked and White-Coat hypertension in Pre-Hypertensive and stage 1 hypertensive patients with the use of TeleMRPA. Arq Bras Cardiol. 2019;113(5):970–975. doi: 10.5935/abc.20190147.
- World Health Organization. Panamerican health organization. The sustainable health agenda for the Americas 2018–2030. A call to action for health and well-being in the region. Available from: https://iris.paho.org/bitstream/handle/10665.2/49170/CSP296-eng.pdf?sequence=1&isAllowed=y
- Garcia Saiso S, Marti MC, Malek Pascha V, et al. Facilitadores a la implementación de la telemedicina en las américas [implementation of telemedicine in the americas: barriers and facilitators barreiras e facilitadores Para a implementação da telemedicina nas américas]. Rev Panam Salud Publica. 2021;45:e131. doi: 10.26633/RPSP.2021.131.
- Delevidove de Lima Verde Brito T, Baptista RS, de Lima Lopes PR, et al. Collaboration between medical professionals: special interest groups in the Brazilian telemedicine university network (RUTE). Telemed J E Health. 2019;25(10):902–910. doi: 10.1089/tmj.2018.0075.
- World Health Organization. Panamerican Health Organization Conversaciones sobre eSalud Gestión de información, diálogos e intercambio de conocimientos para acercarnos al acceso universal a la salud. Available from: https://iris.paho.org/bitstream/handle/10665.2/28391/9789275318287_spa.pdf?sequence=1&isAllowed=y
- Gajarawala SN, Pelkowski JN. Telehealth benefits and barriers. J Nurse Pract. 2021;17(2):218–221. doi: 10.1016/j.nurpra.2020.09.013.
- Rubinstein A, Miranda JJ, Beratarrechea A; GISMAL Group, et al. Effectiveness of an mHealth intervention to improve the cardiometabolic profile of people with prehypertension in low-resource urban settings in latin america: a randomised controlled trial. Lancet Diabetes Endocrinol. 2016;4(1):52–63. doi: 10.1016/S2213-8587(15)00381-2.
- Piskorz D, Díaz-Barreiro LA, López Santi R, et al. Blood pressure telemonitoring and telemedicine for hypertension management-positions, expectations and feasibility of Latin-American practitioners. SURVEY carried out by several cardiology and hypertension societies of the americas. Blood Press. 2022;31(1):236–244. doi: 10.1080/08037051.2022.2123781.
- Roldán-Gómez FJ, Jordán-Ríos A, Alvarez-Sangabriel A, et al. Telemedicine as an instrument for cardiological consultation during the COVID-19 pandemic. Arch Cardiol Mex. 2020;90(Supl):88–93. doi: 10.24875/ACM.M20000065.
- Panamerican Health Organization. Framework for the implementation of a telemedicine service. 2016. Available from: https://iris.paho.org/bitstream/handle/10665.2/28413/9789275319031_spa.pdf?sequence=6&isAllowed=y
- Secretarìa de S. Centro nacional de excelencia tecnológica en salud, México. Análisis de plataformas para servicios de telemedicina. Available from: https://cenetec-difusion.com/observatoriotelesalud/wp-content/uploads/2020/12/Analisis-de-Plataformas-para-servicios-de-telemedicina.pdf
- United Nations. ECLAC report. Illiteracy affects almost 38 million people in Latin America and the Caribbean. 2013. Available from: https://www.cepal.org/en/news/illiteracy-affects-almost-38-million-people-latin-america-and-caribbean
- Gopal RK, Solanki P, Bokhour BG, et al. Provider, staff, and patient perspectives on medical visits using clinical video telehealth: a foundation for educational initiatives to improve medical care in telehealth. J Nurse Pract. 2021;17(5):582–587. doi: 10.1016/j.nurpra.2021.02.020.
- Edgoose JYC. Exploring the face-to-Face: revisiting patient-doctor relationships in a time of expanding telemedicine. J Am Board Fam Med. 2021;34(Suppl):S252–S254. doi: 10.3122/jabfm.2021.S1.200398.
- dos Santos AF, Fernández A. Desarrollo de la telesalud en América Latina. Aspectos conceptuales y estado actual. Available from: https://repositorio.cepal.org/bitstream/handle/11362/35453/1/S2013129_es.pdf
- Stergiou GS, Parati G, Kollias A, et al. Requirements for design and function of blood pressure measuring devices used for the management of hypertension: consensus statement by the European society of hypertension working group on blood pressure monitoring and cardiovascular variability and STRIDE BP. J Hypertens. 2023; doi: 10.1097/HJH.0000000000003482.
- Future of Life. FLI open letter: pause Giant AI experiments. Available from: https://futureoflife.org/