Abstract
Purpose
The aim of this study was to investigate the clinical and demographic variation in the prevalence of substance use among the general psychiatric population in Norway.
Methods
A national census in psychiatric institutions and outpatient clinics was conducted. Data were returned for 2358 inpatients (response rate, 65%) and 23,167 outpatients (response rate, 60%). Substance use was measured based on substance use disorder diagnosis or reported substance use in the last 4 weeks (alcohol 2–4 days a week or more frequently/illicit drug use). Regression analyses controlling for demographic and sociodemographic characteristics were carried out.
Results
Substance use was identified in 32.4% of inpatients and 13.9% of outpatients. The most frequently reported substances used were alcohol, sedatives and cannabis. Among inpatients, the prevalence of substance use was highest in patients with schizophrenia, personality disorders and anxiety disorders. Among outpatients, the prevalence was highest in patients with schizophrenia and other psychoses. Inpatients with anxiety disorders and outpatients with schizophrenia and other psychoses had a significantly higher risk of substance use than other patients. In both samples, the prevalence of substance use was higher among males, 24 to 29-year-olds and the most socially deprived.
Conclusions
This study provides further knowledge about patients at risk for co-morbid substance abuse and poor treatment outcomes. Clinicians may consider targeting patients with schizophrenia and other psychoses, young males and those who are socially deprived in efforts to prevent emerging substance abuse and improve outcomes.
Introduction
The high prevalence of co-morbid substance use disorders (SUD) and mental health disorders documented in epidemiological research [Citation1,Citation2] has also been found in studies of the psychiatric patient population. As examples, register-based studies from Denmark and Norway among patients with psychiatric disorders have estimated lifetime prevalence of SUD of 25% for anxiety and depression [Citation3] and a 5-year prevalence of SUD of 25% of patients with schizophrenia [Citation4]. Patients with mental disorders may be especially vulnerable to the negative consequences of substance use. For instance, recent research has suggested that among individuals with schizophrenia, even non-problematic drug use may increase the risk of developing SUD [Citation5].
Most previous studies on substance use among psychiatric patients were carried out among patients within specific diagnostic categories, such as schizophrenia, bipolar disorders and major depression [Citation4,Citation6–10]. A strong association between severe mental disorders and SUD has been shown both among inpatients and outpatients [Citation8], as well as among patients in acute departments [Citation11,Citation12]. The most frequently reported substances used among patients with severe mental disorders were alcohol, cannabis, sedatives and stimulants [Citation3,Citation11,Citation12]. In some studies, alcohol was found to be the most prevalent drug used across all psychiatric disorders [Citation3], whereas other studies estimated the use of illicit substances to be more common than alcohol use among those with severe mental illness [Citation4,Citation8].
While many studies have investigated SUD among patients with severe mental illness, substance use in patients with less severe mental disorders, such as anxiety and mood disorders [Citation13], has received less attention. One of the few studies conducted in a sample of patients drawn from the general psychiatric patient population indicated a higher prevalence of SUD among inpatients than outpatients, and particularly among patients with personality disorders [Citation14]. However, this study did not report data on the type of substances used. Another study of a non-selected sample of patients receiving treatment in community mental health centres in Norway, where anxiety and mood disorders are common psychiatric disorders, identified SUD in 20% of the patients. This study also showed that having SUD was associated with a lower prevalence of anxiety and depression [Citation15].
Despite previous research among psychiatric patients used different samples and different methods to identify substance use, and thus reported varying SUD prevalence rates, the findings regarding the characteristics of patients with substance use problems are consistent. Previous studies have shown that co-occurring mental disorders and SUD are associated with being male [Citation3,Citation8,Citation10,Citation14], younger and single [Citation14,Citation16]. Moreover, research has demonstrated that psychiatric patients with SUD have less educational attainment [Citation3,Citation14,Citation17] and generally more adverse socioeconomic characteristics [Citation15].
The literature, including Nordic studies, suggests that substance use in individuals with mental disorders is associated with higher levels of antisocial and behavioural challenges [Citation14,Citation18,Citation19], more complicated recovery processes [Citation15] and poorer outcomes [Citation20,Citation21]. To date, however, research on the characteristics of patients with substance use in mental health services has mainly focused on delimited patient populations. To the authors’ knowledge, this was the first nationwide European study evaluating the prevalence of co-occurring substance use in the entire general patient population in inpatient and outpatient specialized mental health services. Hence, the current study extended existing knowledge by investigating co-occurring substance use across broader groups of psychiatric disorders.
Aims of the study
The aims of this study were to examine:
The prevalence of co-occurring substance use among inpatients and outpatients in specialized mental health services;
the substance use characteristics of these patients, in terms of psychiatric disorders and type of drug used most frequently; and
the demographic (age and gender) and sociodemographic (education, income and marital status) characteristics of outpatients and inpatients with co-occurring substance use compared with other patients.
Materials and methods
Setting
In Norway, as in most other European countries [Citation22], there are distinct specialized mental health and SUD treatment departments. Specialized mental health services are owned on behalf of the state by four regional health authorities (RHAs), which are responsible for the provision of health services for the population in their area. Specialized mental health services are organized together with general hospital services in 19 health trusts. The services are mostly public, and the private health service providers have an operating agreement with the RHA [Citation23]. General practitioners or other specialist health services make referrals of patients to mental health services. As in most Western countries, the services for people with mental disorders have gone through major changes in recent decades. There has been a reduction in the number of patients staying in psychiatric institutions with most people with mental problems being provided with outpatient mental health services. According to National guidelines for treatment and rehabilitation of substance use problems and dependency [Citation24], patients with severe mental illness such as psychosis, bipolar disorders and severe anxiety and depression and co-occurring SUD should receive treatment for their substance use problems within mental health care. Whereas patients with severe SUD and co-occurring less severe mental health disorders should receive treatment within specialized SUD treatment services.
Design
A comprehensive national census of patients in mental health treatment, commissioned and financed by the Norwegian Directorate of Health, was carried out by the SINTEF Research Foundation. The census was conducted in all psychiatric wards and departments (including acute wards) providing inpatient treatment on a specific date, and in all clinics and departments (including community mental health centres), providing outpatient treatment during a specific 14-day period. Each patient’s clinician was responsible for completing the form. Because the study had a national cross-sectional design with high coverage of institutions in specialized mental health services, it was possible to estimate the point prevalence for the entire patient population. The Regional Committee for Medical and Health Research Ethics (reg. no. 2012/848) approved the current study.
Data collection
All inpatients on a given day (20 November 2012) and all outpatients who had one or more consultations during a 14-day period (15–28 April 2013) were the targeted study participants. All mental health services in public and private sectors were invited to participate in the census. Several months prior to the census, the service managers and clinicians received information describing the project and the data collection procedures. The clinicians completed one form per patient. The registration form included a wide range of topics, including demographics and sociodemographic characteristics, main and secondary diagnosis (International Classification of Diseases, ICD-10) and patient-reported substance use in the last 4 weeks preceding treatment. The clinicians obtained information about substance use by asking whether the patient had used alcohol or drugs during the past 4 weeks preceding treatment. Those who responded positively were asked further: (a) ‘What was your most frequently used substance’ and (b) ‘How frequently did you use this substance?’ The response options included the following: ‘less than once a week;’ almost weekly; 2–4 times a week; almost daily. The completed forms were returned by registered mail to a firm that performed scanning and coarse quality control of the data. The project team performed further quality control of the data files.
Sample
In total, 94 of the 104 psychiatric inpatient departments and 107 of the 110 psychiatric outpatient clinics in the health trusts participated in the census. Most of the units that did not participate were small, and they cited a lack of time as their reason for not participating. Non-participating clinics comprised 1% of all outpatient consultations, and non-participating institutions comprised 4% of all inpatient days during 2012. Data were returned for 2,358 inpatients and 23,167 outpatients. Based on data from the National Patient Register on the number of patients attending the mental health services during the inclusion periods, the response rates were estimated to be 65% of 3618 inpatients and 60% of 38,904 outpatients.
Variables
Psychiatric diagnoses
Data from main psychiatric diagnosis was collected and the following diagnostic categories were used: Schizophrenia (F20), Other psychoses (F22–F25, F28, F29), Bipolar disorder (F31), Depression (F32–F34), Anxiety (F40, F41), PTSD (F43.1), Eating disorders (F50), Personality disorders (F60, F61), Other psychiatric diagnoses or unspecified (all other F-diagnoses).
Substance use
The current measure of substance use was based on the recorded ICD-10 diagnosis of SUD as a secondary diagnosis (F10–F19), or patient-reported substance use. We constructed a dichotomized variable with a value of 1 for the presence of a SUD diagnosis or patient-reported regular alcohol use (i.e. 2-4 times a week or more frequently)/occasional illicit drug use. The type of drug used was categorized according to ICD-10 in the following categories: alcohol (F10), opioids (F11), cannabis (F12), sedatives (F13, benzodiazepines and other addictive drugs), stimulants (F14 and F15, cocaine, amphetamines, and other stimulants) or multiple substance use (F19, combinations of type of drugs used).
Demographic and sociodemographic characteristics
In addition to gender and age, we included education (where low education corresponds to only primary school, medium education to secondary school and high education to a university or other higher education), income (with the categories income from labour, health-related benefits, other economic support) and marital status (grouped in the three categories married/cohabitant/partner, separated/divorced/widow(er) and single/unmarried).
Data analyses
The binary nature of the substance use variable as the dependent variable implies a logit model. The STATA software package was used for all analyses (Stata/SE 14.2 for Windows; StataCorp LP, College Station, TX). We estimated 3 models; the first model included only diagnoses (Model 1), gender and age were added in the second model (Model 2), and the third model also included the level of the sociodemographic variable of education, the main source of income and marital status (Model 3).
Results
Prevalence of substance use
The prevalence of substance use is presented in . Substance use was identified in 390 inpatients (16.4%) based on ICD-10 diagnosis (F10-F19), and in an additional 373 inpatients (15.8%) based on recorded substance use. The total prevalence of substance use among inpatients was 32.4%. Among outpatients, substance use was identified in 1,300 outpatients (5.6%) based on ICD-10 diagnosis (F10-F19), and in an additional 1,910 outpatients (8.2%) based on recorded substance use. The total prevalence of substance use among outpatients was 13.9%.
Table 1. Prevalence of substance use among inpatients and outpatients in specialized mental health services.
Substance use was identified in 42.0% of all male inpatients, whereas the corresponding prevalence in female inpatients was 24.0%. Male patients diagnosed with schizophrenia had almost twice the risk of substance use compared with female patients suffering from the same mental illness. The same result appeared in inpatients diagnosed with bipolar disorders, with substance use being three times more prevalent for male than for female patients.
Substance use was prevalent in 20.0% of all male outpatients, versus only 10.1% of female outpatients. Consistent with inpatient results, male outpatients diagnosed with schizophrenia had more than twice the risk of substance use than female patients suffering from the same mental illness. The same male–female difference in the prevalence of substance use also appeared among patients with bipolar disorders and depression. Among patients with personality disorders, the prevalence was roughly similar for females (13.4%) and males (16.4%). Within the various categories of diagnoses, the prevalence of substance use was lowest among those with eating disorders (8.3%), and few of these patients were men (3.2%).
Substance use characteristics
Substance use characteristics are presented in . Among inpatients, cannabis and sedatives were the most frequently used substances, accounting for 12.3 and 10.9% of the total prevalence of substance use, respectively. The use of any illegal substances, such as cannabis (23.8%) and stimulants (20.8%), was more prevalent among patients diagnosed with schizophrenia than patients with other psychiatric diagnoses.
Table 2. Psychiatric diagnosis and most frequently used drug type among inpatients and outpatients in specialized mental health services.
The substance most frequently used among patients diagnosed with anxiety disorders, personality disorders, and PTSD were sedatives, with rates of 21.0, 17.9, and 17.3%, respectively. Among patients with bipolar disorders, the use of alcohol (11.3%) was more prevalent than the use of any illegal substance.
Among outpatients, the use of alcohol was more prevalent (6.3%) than the use of any illegal substances. In patients diagnosed with depression, who represented the largest diagnostic outpatient group, alcohol use was more prevalent (6.1%) than any illicit drug use. Cannabis and sedatives were the most frequently reported illegal substances used, accounting for 4.0% and 3.7% of the total prevalence of substance use, respectively. Patients with schizophrenia had higher use of illegal substances, particularly stimulants (11.2%) and cannabis (9.2%), than patients with other psychiatric diagnoses.
Demographic and sociodemographic characteristics
shows that the prevalence of substance use was highest among inpatients aged under 40 years, particularly among those aged 24–29 years (43%). Among patients in outpatient treatment settings, there were relatively small differences in the prevalence of substance use between age groups, with rates of 13% and 18% for those aged under 40 years and those aged 60–69 years, respectively. Patients with lower levels of education (primary school or less) had a higher prevalence of substance use than those with higher levels of education (university), both among inpatients (36 and 22%, respectively) and outpatients (17 and 10%, respectively). Among both inpatients and outpatients, those with health-related benefits had a higher prevalence of substance use than those with income from labour or other sources. Finally, being married, cohabiting or having a partner implied a lower prevalence of substance use than having any other marital status.
Table 3. Demographic and sociodemographic characteristics of patients in specialized mental health services with substance use.
Regression results
, and provide the results of multivariate logistic regressions of the association between patient characteristics and odds ratios for substance use. Among inpatients (), the differences in substance use prevalence in diagnoses (Model 1) were reduced when we added demographic (Model 2) and sociodemographic (Model 3) characteristics. Patients with anxiety disorders had significantly higher substance use prevalence than patients with schizophrenia when we controlled for demographic and sociodemographic characteristics.
Figure 1. Regression results showing odds ratios and confidence intervals for inpatients: Model 1 (diagnoses only), Model 2 (diagnoses, gender and age), Model 3 (diagnoses, gender and age, level of education, main source of income and marital status), n = 2358.
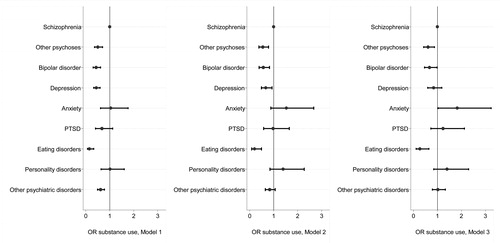
Figure 2. Regression results showing odds ratios and confidence intervals for outpatients: Model 1 (diagnoses only), Model 2 (diagnoses, gender and age), Model 3 (diagnoses, gender and age, level of education, main source of income and marital status), n = 23,167.
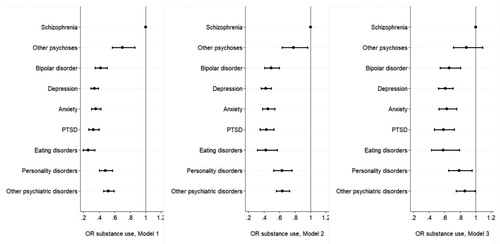
Table 4. Regression results (logit) where the dependent variable is 0 (no co-occurring substance use) or 1 (co-occurring substance use) showing odds ratios and standard errors for inpatients (n = 2358) and outpatients (n = 23,167).
Among outpatients (), demographic and sociodemographic characteristics explained fewer of the differences in substance use prevalence between the diagnostic categories. Patients diagnosed with schizophrenia and patients with other psychoses did not differ significantly in substance use prevalence in Model 3.
Male patients had a higher prevalence of substance use in all model specifications. The youngest age groups (i.e. 18–23 years and 24–29 years) had higher substance use prevalence among inpatients, while the opposite was found among outpatients in Model 3.
The socioeconomic differences found in the descriptive analyses were also valid in the regression analyses; lower education, receiving benefits rather than deriving income from labour, and not having a partner implied higher substance use prevalence in both samples, even when controlling for demographic characteristics and diagnoses.
Discussion
This nationwide census conducted in psychiatric institutions and outpatient clinics showed that substance use occurred more frequently among inpatients than outpatients, and among patients with severe mental illness (e.g. schizophrenia, other psychoses and bipolar disorders) in both treatment settings. Among inpatients, the most frequently used substances were cannabis and sedatives, whereas alcohol was more prevalent than the use of any illegal substances among outpatients. In both samples, substance use was more prevalent in young males and the most socially deprived. The higher prevalence of both SUD diagnosis and substance use found among inpatients aligns with previous studies [Citation8,Citation14] and suggests that in inpatient treatment, there is a different patient case-mix with relatively higher rates of severe mental illness, such as schizophrenia and major depression, which are typically associated with higher rates of co-occurring SUD [Citation3,Citation4,Citation8].
Methodological and sample differences complicate the comparison of results between studies. Of the few studies conducted in general psychiatric outpatient and inpatient treatment settings, Rush and Koegl’s study [Citation14] in mental health services in Ontario is most comparable with the present work. They reported a prevalence of SUD (based on diagnosis) among inpatients of 15.6%, which is similar to the point prevalence of recorded SUD diagnosis in the current inpatient sample (16.4%). However, the current SUD rate of 5.6% based on recorded diagnosis found in the outpatient sample is relatively low in comparison with the 11% SUD prevalence among outpatients reported by Rush and Koegl [Citation14]. When comparing the prevalence of substance use in psychiatric patients across countries, one should take into account possible between-country differences in the organization and delivery of health services. For example, community addiction services have a more prominent role in Norway and other European countries than in the USA [Citation22]. Moreover, in Norway, community-integrated mobile teams offer dual treatment for individuals with mental illness and substance abuse.
Consistent with results from other studies of psychiatric patients, the present results showed that alcohol, cannabis and sedatives were the most commonly used substances [Citation3,Citation11,Citation12]. Also in line with previous reports [Citation4,Citation8], the use of illegal substances, particularly cannabis, occurred more frequently among inpatients than outpatients, and among patients with schizophrenia and other psychoses compared to patients with other mental disorders. Although the association between the use of illicit drugs and severe mental illness is frequently recognized in the literature, the basis for the link is still being discussed [Citation25–27]. For example, research concerning the association between schizophrenia and SUD has suggested a common genetic risk [Citation28], or that patients with a genetic risk for schizophrenia are more vulnerable to substance use [Citation29].
Consistent with previous clinical studies, the current results showed that substance use occurred twice as often among men than among women [Citation8,Citation10]. The prevalence of substance use was particularly high among inpatient young males, aged 18–29 years. This finding may reflect the high prevalence of substance-induced mental disorders among inpatients, which is associated with symptom onset at a younger age [Citation8,Citation30]. Our results also confirmed the sociodemographic differences in the prevalence of substance use reported elsewhere [Citation3].
After adjusting for demographic and sociodemographic variables in multivariate analysis, the differences in prevalence rates of substance use between the psychiatric diagnostic categories among inpatients were reduced, indicating that substance use was associated with greater levels of social and economic disadvantages, as reported elsewhere [Citation3]. The present results showed that independent of demographic and sociodemographic factors, inpatients with anxiety disorders, who constituted a relatively small subsample of those in inpatient treatment (n = 62), had the highest prevalence of substance use, particularly alcohol and sedatives; this suggests that this subsample constituted a group of patients who used substances to cope with severe anxiety symptoms [Citation31,Citation32].
A Canadian study found that sociodemographic characteristics did not explain differences in substance use prevalence among inpatients, while the opposite was found for outpatients [Citation14]. Our results imply that sociodemographic characteristics explain differences in the prevalence of substance use among both inpatients and outpatients. Furthermore, Rush and Koegl [Citation14] found that among outpatients, sociodemographic variables such as young age, being male, single, and having a low level of education were associated with the prevalence of substance use. Our results indicate that outpatients in the youngest age group (18 to 23-years-old) were at lower risk of substance use than patients older than 24 years. However, we also found that less of the difference in the prevalence of substance use between psychiatric disorders was explained by sociodemographic variables among outpatients than inpatients, reflecting a relatively homogeneous outpatient population. Differences in access to health services between countries and subsequent differences in patient composition in specialty mental health services might explain the non-congruent findings.
Strengths and limitations
The current study represents one of the very few nationwide studies investigating the prevalence of co-occurring substance use among both inpatients and outpatients in specialized mental health services. Hence, the current study contributes to increased knowledge on co-occurring substance use across broader groups of psychiatric disorders. Such information is important for the clinicians and providers of specialized mental health care, but also of relevance for community mental health services that are responsible for the further rehabilitation of these patients. However, the study has several limitations that should be noted.
The study included 90% of all inpatient clinics and 97% of all outpatient clinics in Norway. However, not all clinics included all their patients in the census. An important limitation of the current study was that we did not have any information about the individuals who were not included in the census. We were therefore unable to examine the representativeness of the sample and any possible skewness of the prevalence of substance use in the data material. It is possible that clinicians considered reporting as time-consuming and excluded the most complex cases (i.e. especially patients with substance use problems). On the other hand, the study design emphasizes patients in long-term treatment and patients with more frequent consultations, as they were more likely to be receiving treatment at any given time. One possible consequence of this is that the census included relatively more patients with an established relationship with a therapist, among whom the prerequisites for an accurate account of the patients’ substance use were relatively good [Citation33].
A number of studies have documented that substance use and SUD are under-reported and underdiagnosed in psychiatric treatment settings [Citation34–36]. A recent Norwegian Board of Health study highlighted the existing deficiencies in specialized mental health services regarding the investigation and examination of patients with possible concurrent SUD [Citation37]. The under-identification of substance use may be related to insufficient knowledge of substance abuse issues among clinicians [Citation35] and/or the lower status of working with substance users [Citation38]. Moreover, the accuracy of reported substance use may depend on the patients’ responses when asked about substance use. Such conditions may vary between treatment settings [Citation33]. It is possible that the intensive treatment and close monitoring of patients in inpatient treatment allowed clinicians to make a more thorough evaluation of the patients’ substance use behaviour, resulting in higher identification rates than in outpatient treatment settings.
Knowledge of substance use behaviour among mentally ill patients’ may have clinical significance in reducing relapse rates [Citation15] and strengthening treatment efforts to reduce the risk of developing substance abuse [Citation5]. A more detailed measurement of the severity of substance use among the patients could have provided useful information to assess their treatment needs. The current study did not address what kind of treatment was provided. Hence, we do not know whether the patients received adequate treatment for co-occurring substance use.
An additional limitation is that the current results may not generalize to countries with different structures of mental health and addiction treatment services. However, it is reasonable to believe that our findings can generalize to systems with public health services with separated rather than integrated specialized treatment for mental illness and SUD.
Conclusion and implications
The current study included patients from the general psychiatric patient population to provide further knowledge about patients at risk for co-morbid substance abuse. Patient characteristics associated with substance use include having schizophrenia or other psychoses, being a young male and being socially deprived. Clinicians may want to target patients with these characteristics in efforts to identify and prevent emerging substance abuse and improve treatment outcomes.
More research is necessary to investigate more closely the substance use treatment needs among patients in mental health services, and the treatment approaches and services provided for this patient group. Moreover, future research should determine the clinical consequences of substance use in the general psychiatric patient population and investigate whether efforts designed to identify and manage substance use are effective in improving their treatment process and outcome.
Acknowledgements
We would like to thank the personnel in the psychiatric wards and departments for facilitating the data collection, and for their contribution to this research. The Norwegian Directorate of Health funded the data collection.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Notes on contributors
Helle Wessel Andersson
Helle Wessel Andersson M.Sc, Ph.D., Researcher AeO: Addiction research; Health services research; Treatment outcome.
Solfrid E. Lilleeng
Solfrid E. Lilleeng M.Sc, Social scientist AeO: Health services research; Health statistics.
Torleif Ruud
Torleif Ruud MD, Ph.D, Psychiatrist; Professor AeO: Mental illness; Treatment; Public Health.
Solveig Osborg Ose
Solveig O.Ose M.Sc. Ph.D. Social scientist; Researcher AoE: Mental illness; Health statistics; Mental health services.
References
- Kessler RC. Impact of substance abuse on the diagnosis, course, and treatment of mood disorders: the epidemiology of dual diagnosis. Biol Psychiatry. 2004;56:730–737.
- Lai HMX, Cleary M, Sitharthan T, et al. Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990-2014: a systematic review and meta-analysis. Drug Alcohol Depend. 2015;154:1–13.
- Toftdahl NG, Nordentoft M, Hjorthøj C. Prevalence of substance use disorders in psychiatric patients: a nationwide Danish population-based study. Soc Psychiatry Psychiatr Epidemiol. 2016;51(1):129–140.
- Nesvåg R, Knudsen GP, Bakken IJ, et al. Substance use disorders in schizophrenia, bipolar disorder, and depressive illness: a registry-based study. Soc Psychiatry Psychiatr Epidemiol. 2015;50(8):1267–1276.
- Petersen SM, Toftdahl NG, Nordentoft M, et al. Schizophrenia is associated with increased risk of subsequent substance abuse diagnosis: a nation‐wide population‐based register study. Addiction. 2019;114(12):2217–2226.
- Di Florio A, Craddock N, van den Bree M. Alcohol misuse in bipolar disorder. A systematic review and meta-analysis of comorbidity rates. Eur Psychiatry. 2014;29(3):117–124.
- Helseth V, Lykke-Enger T, Johnsen J, et al. Substance use disorders among psychotic patients admitted to inpatient psychiatric care. Nord J Psychiatry. 2009;63(1):72–77.
- Hunt GE, Large MM, Cleary M, et al. Prevalence of comorbid substance use in schizophrenia spectrum disorders in community and clinical settings, 1990-2017: systematic review and meta-analysis. Drug Alcohol Depend. 2018;191(1):234–258.
- Kavanagh DJ, Waghorn G, Jenner L, et al. Demographic and clinical correlates of comorbid substance use disorders in psychosis: multivariate analyses from an epidemiological sample. Schizophr Res. 2004;66(2–3):115–124.
- Messer T, Lammers G, Müller-Siecheneder F, et al. Substance abuse in patients with bipolar disorder: a systematic review and meta-analysis. Psychiatry Res. 2017;253:338–350.
- Fløvig JC, Vaaler AE, Morken G. Substance use at admission to an acute psychiatric department. Nord J Psychiatry. 2009;63(2):113–119.
- Helseth V, Samet S, Johnsen J, et al. Independent or substance-induced mental disorders? An investigation of comorbidity in an acute psychiatric unit. J. Dual Diagn. 2013;9(1):78–86.
- Jané-Llopis E, Matytsina I. Mental health and alcohol, drugs and tobacco: a review of the comorbidity between mental disorders and the use of alcohol, tobacco and illicit drugs. Drug Alcohol Rev. 2006;25(6):515–536.
- Rush B, Koegl CJ. Prevalence and profile of people with co-occurring mental and substance use disorders within a comprehensive mental health system. Can J Psychiatry. 2008;53(12):810–821.
- Wüsthoff LE, Waal H, Ruud T, et al. A cross-sectional study of patients with and without substance use disorders in community mental health centres. BMC Psychiatry. 2011;11:93.
- Mueser KT, Yarnold PR, Rosenberg SD, et al. Substance use disorder in hospitalized severely mentally ill psychiatric patients: prevalence, correlates, and subgroups. Schizophr Bull. 2000;26(1):179–192.
- Clausen H, Ruud T, Odden S, et al. Hospitalisation of severely mentally ill patients with and without problematic substance use before and during assertive community treatment: an observational cohort study. BMC Psychiatry. 2016;16(1):125.
- Ose SO, Lilleeng S, Pettersen I, et al. Risk of violence among patients in psychiatric treatment: results from a national census. Nord J Psychiatry. 2017;71(8):551–560.
- Rund BR. A review of factors associated with severe violence in schizophrenia. Nord J Psychiatry. 2018;72(8):561–571.
- Reininghaus U, Dutta R, Dazzan P, et al. Mortality in schizophrenia and other psychoses: a 10-year follow-up of the ӔSOP first-episode cohort. Schizophr Bull. 2015;41(3):664–673.
- van Dijk D, Koeter MW, Hijman R, et al. Effect of cannabis use on the course of schizophrenia in male patients: a prospective cohort study. Schizophr Res. 2012;137(1–3):50–57.
- van Wamel A, van Rooijen S, Kroon H. 2015. Intergrated tretament: the model and European Experiences. In: Dom G, Moggi F, editors. Co-occurring addicitive and psyschiatric disorders. Heidelberg, Berlin: Springer, pp 28–45.
- Lindahl AK. 2016. The Norwegian health care system, 2015. In: Mossialos E, Wentzl M, Osborn R, Sarak D, editors. International profiles of health care systems, 2015. New York (NY): The Commonwealth Fund; p. 133–141.
- Norwegian Directorate of Health. 2011. [National guidelines for assessment, treatment and follow-up people with concomitant substance abuse and mental illness]. Oslo (Norway): Norwegian Directorate of Health. Norwegian.
- Burns JK. Pathways from cannabis to psychosis: a review of the evidence. Front Psychiatry. 2013;4:128.
- Cerdá M, Sagdeo A, Galea S. Comorbid forms of psychopathology: key patterns and future research directions. Epidemiol Rev. 2008;30(1):155–177.
- Torvik FA, Rosenström TH, Gustavson K, et al. Explaining the association between anxiety disorders and alcohol use disorder: a twin study. Depress Anxiety. 2019;36(6):511–522.
- Ikeda M, Okahisa Y, Aleksic B, et al. Evidence for shared genetic risk between methamphetamine-induced psychosis and schizophrenia. Neuropsychopharmacology. 2013;38(10):1864–1870.
- Khokhar JY, Dwiel LL, Henricks AM, et al. The link between schizophrenia and substance use disorder: a unifying hypothesis. Schizophr Res. 2018;194:78–85.
- Green AI, Tohen MF, Hamer RM, et al. First episode schizophrenia-related psychosis and substance use disorders: acute response to olanzapine and haloperidol. Schizophr Res. 2004;66(2–3):125–135.
- Robinson J, Sareen J, Cox BJ, et al. Self-medication of anxiety disorders with alcohol and drugs: results from a nationally representative sample. J Anxiety Disord. 2009;23(1):38–45.
- Turner S, Mota N, Bolton J, et al. Self-medication with alcohol or drugs for mood and anxiety disorders: a narrative review of the epidemiological literature. Depress Anxiety. 2018;35(9):851–860.
- Chung RK, Large MM, Starmer GA, et al. The reliability of reports of recent psychoactive substance use at the time of admission to an acute mental health unit. J Dual Diagn. 2009;5(3–4):392–403.
- Hansen SS, Munk-Jørgensen P, Guldbaek B, et al. Psychoactive substance use diagnoses among psychiatric in-patients. Acta Psychiatr Scand. 2000;102(6):432–438.
- Sundström C, Petersén E, Sinadinovic K, et al. Identification and management of alcohol use and illicit substance use in outpatient psychiatric clinics in Sweden: a national survey of clinic directors and staff. Addict Sci Clin Pract. 2019;14(1):10.
- Wüsthoff LE, Waal H, Ruud T, et al. Identifying co-occurring substance use disorders in community mental health centres. Tailored approaches are needed. Nord J Psychiatry. 2011;65(1):58–64.
- Norwegian Board of Health. 2019. Oppsummering av landsomfattende tilsyn i 2017-2018 med spesialisthelsetjenster for pasienter med psykiske lidelser og mulig samtidig ruslidelse. (Summary of Resport of the Norwegian Board of Health Supervision). Rapport fra Helsetilsynet, 7/2019. ISBN:978-82-93595-25-0. www.helsetilsynet.no
- Gilchrist G, Moskalewicz J, Slezakova S, et al. Staff regard towards working with substance users: a European multi-centre study. Addiction. 2011;106(6):1114–1125.
