Introduction
The presence of small (15-50 µm), irregular-shaped microcysts with defined borders in the corneal epithelial layer indicates chronic corneal hypoxia during extended contact lens wear,Citation1 but may also be observed in non-contact lens wearers with less severity.Citation2 They usually cause mild or no visual impairment.
Orthokeratology lenses reshape the corneal surface overnight as a result of mechanical and fluid forces. While mild microcysts have been reported in adult orthokeratology wearers,Citation3 they have not been observed in orthokeratology studies on children, spanning 2–5 years.Citation4–6
Presented here is a case of corneal oedema associated with over-wear of decentred orthokeratology lenses in a child being kept at home during the novel coronavirus (COVID-19) pandemic.
Case report
An 11-year-old female student, with unremarkable ocular health and initial refractive errors R: −3.75/-1.00x175 and L: −4.00/-0.75x180, participated in an orthokeratology myopia control study. She was fitted with KATT BE Free lenses (Precision Technology, Canada), of HDS100 material (oxygen permeability 100 barrer) (Paragon Vision Sciences, Mesa, AZ, USA). Len parameters, base curve/diameter/back optic power were R: 8.31 mm/10.6 mm/+0.50 D and L: 8.41 mm/10.6 mm/+0.50 D.
Orthokeratology lens wear commenced in September 2018. All lens care solutions were provided with compliments of Ophtecs Corporation, Tokyo, Japan (). Instructions on lens use included (a) wearing lenses on a nightly basis for at least eight, but no more than 10 hours, and (b) not to wear lenses when feeling unwell, taking medication, or experiencing ocular discomfort or red/sore eyes. Refraction and ocular health were assessed on a weekly basis in the first month of lens wear and every three months thereafter. Unscheduled visits were arranged as required, for example, in case of adverse events.
Table 1. Orthokeratology care solutions from Ophtecs Corporation (Tokyo, Japan)
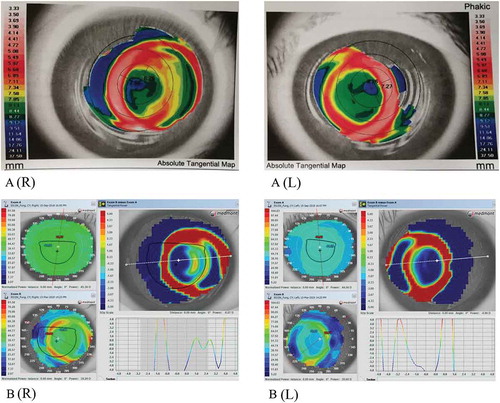
During the first year of orthokeratology treatment, no complaints or significant adverse events were reported or observed; only mild lens decentration of less than 0.50 mm was noted in both eyes (). Distances between the geometric centre of the eye and the nasal/temporal edges of the treatment zone were manually determined, and lens decentration was determined as the average of their differences. At the aftercare visits (May to September 2019), after several lens modifications, monocular UVA, and best-corrected visual acuity (BCVA) ranged from 0.10 to 0.12 and 0.00 to 0.06 LogMAR, respectively.
Table 2. Clinical findings from September 2018 to September 2019
In December 2019, moderate nasal lens decentration (R: 0.85 mm, L: 0.96 mm) () was observed and uncorrected visual acuity was affected (R: 0.24, L: 0.18 logMAR). Vertically curved bands of grade 1 mid-peripheral corneal staining were observed in both eyes. Best-corrected visual acuity was 0.00 logMAR in both eyes. Discontinuation of lens wear for five days was advised.
Figure 1. Corneal topography indicating lens decentration. A: 15-month visit, B: 18-month visit. R-right eye, L-left eye. The Aladdin HW3.0 (Topcon Medical Systems. Inc., Oakland US) was used at 15-month visit, and the Medmont E300 (Version 6.1.2, Medmont Pty. Ltd., Camberwell Australia) was used at 18-month visit
Due to a school trip and a broken left lens, the subject did not resume lens wear until early January 2020. A follow-up visit was scheduled for 23 January; however, one week prior to the appointment, the parent cancelled, and the COVID-19 outbreak commenced a few days later. All clinics were closed until March 2020. In view of (a) the clinical findings from the last aftercare visit, where only mild ocular staining was observed with no other signs and symptoms, and (b) the desire of the parents for the subject to continue lens wear for myopia control, lens wear was allowed to resume in February. Both subject and parents were reminded to contact the clinic should there be any abnormal symptoms.
At the 18-month visit, uncorrected visual acuity was R: 0.12, L: 0.10 LogMAR. Best-corrected visual acuity was 0.10 logMAR in each eye and no symptoms were reported. Slit-lamp examination revealed grade 4 microcysts,Citation2 covering 70% to 80% of the cornea in both eyes (left eye more severe) (). Sclerotic scatter slit lamp technique revealed the presence of concentric white oedematous rings, indicating loss of transparency (corneal haze) (). There were two circular oedematous rings noted in the right eye and three in the left. The most inner circular haze in the right eye and the middle one in the left eye are likely corresponding to the return zone of the lens (by comparing the slit lamp photos with corneal topography in ). The most temporal circular haze in both eyes is probably relevant to the alignment zone of lenses in both eyes by assumption. Grade 1 (depth) and grade 2 (coverage) corneal staining () was also observed in each eye. Anterior optical coherence tomography (CASIA ss-1000; Tomey, Japan) captures showed a 5% and 7% corneal oedema (compared to the 12-month visit) in the thickest part (temporal) of the cornea in the right and left eyes, respectively. The subject was generally healthy without illness. The subject was compliant with the lens care regime recommended: (a) thoroughly rinsing the lens case with lenses in situ with saline, (b) rubbing and rinsing the lenses with saline before insertion, (c) disinfecting lens case with freshly boiled water 10 mins every week and replacing the lens case monthly. Lens care regime remained the same from 12-month to 18-month visits.
Figure 2. Ocular findings showing corneal A: microcystic responses, B: corneal haze, and C: corneal staining when first noted. R-right eye, L-left eye. Images captures using Topcon slit-lamp biomicroscopy (SL-D7, Topcon Medical Systems Inc., Oakland, USA)
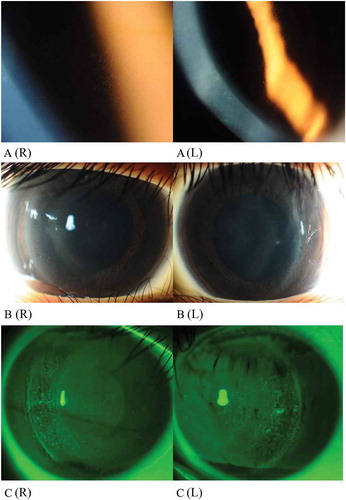
Tangential subtractive topographic maps indicated severe nasal lens decentration (1.57 mm) in the right eye. The left lens displayed severe horizontal decentration (1.03 mm), as well as inferior decentration, with the inner annulus of the corneal steepening very close to the pupil centre (). The corneas were oedematous, especially in the mid periphery (zone of reverse curve of lenses), where light from the slit lamp was apparently bent and distorted ()). On further questioning, the subject admitted that lens wear had increased from eight to nine hours previously, to 12 hours or more, most nights, due to the suspension of school during COVID-19 restrictions during the past month.
Lens wear was terminated. The subject was referred to an ophthalmologist and diagnosed with keratitis due to hypoxia and allergy. TobraDex (0.3% tobramycin and 0.1% dexamethasone) ophthalmic suspension (Alcon Laboratories Inc., Fort Worth, Tex) and Crevit (0.5% levofloxacin hydrate) (Santen, Osaka, Japan) were prescribed, to be applied twice a day for one week.
Six days later, only mild corneal staining and grade 2 microcysts, with reduced density and number (left eye worse than right) were observed. The hazy rings noted previously had subsided significantly in both eyes, and the most temporal hazy ring was no longer observable. Best-corrected visual acuity was R: 0.08, L: 0.10 logMAR at this visit, and improved, about a month later, to R: 0.02, L: 0.04 logMAR.
Forty days later, less than 10 microcysts, scattered over the whole cornea, were observed in each eye, with no corneal haze or corneal staining. Similar findings were observed one week later.
In view of (a) the stable number and size of remaining microcysts, (b) the presence of only mild inferior grade 1 staining in both eyes, and (c) advice from the ophthalmologist, the subject was allowed to resume orthokeratology lens wear in a new pair of lenses one week after the last visit, with wearing time not more than eight hours every night. Potential risks of recurrent hypoxia were explained, and verbal and written consent was re-obtained before resuming lens wear.
At the first-overnight wear visit, grade 1 central staining was observed. Grade 1 microcysts were observed in the inferior cornea from 4 to 7 o’clock. The microcysts were assessed as being grade 2 in both eyes one week later. Topography showed well-centred lenses in both eyes at both the first-overnight and one-week follow-up visits. The subject was asked to cease lens wear immediately. Full recovery was noted 1 month later and the subject was advised to cease ortho-k treatment afterwards.
Discussion
This is believed to be the first reported case of bilateral corneal haze from ‘extended’ orthokeratology lens wear. Corneal haze reduced in severity during the first six days after ceasing lens wear and application of topical drugs, and had subsided completely after 18 days. However, microcysts reappeared one week after resuming lens wear. Epithelial microcysts are important indicators of chronic metabolic stress and are postulated to be cellular debris accumulated due to reduced metabolism induced by chronic hypoxia.Citation2 Previous studies in orthokeratology patients have reported either a mildCitation3 or absentCitation4–6 microcystic response. There do not appear to be any previously published reports of diffuse grade 4 microcysts after 18 months of orthokeratology lens wear.
Oxygen transmissibility required to avoid corneal oedema during closed-eye soft lens wear is estimated to be 125.0 × 10−9 barrer.Citation7 However, orthokeratology lenses do not cover the entire cornea, so the critical oxygen transmissibility required to avoid corneal oedema during overnight orthokeratology lens wear is unknown. In the present case, the orthokeratology lenses used had a moderate oxygen transmissibility of about 50 × 10−9 barrer (calculated with a 0.2 mm centre lens thickness), which is comparable to that used in a previous study reporting no microcystic oedema.Citation6 Since no problems were reported prior to the changes in sleeping patterns, and no adverse signs were observed in other subjects participating in the same study, the corneal oedema observed in this subject was likely to be due to lens over-wear.
Significant lens decentration may also be of aetiological significance, but this could have been a result of the induced oedema. Moderate lens decentration had been observed starting from 15 months of lens wear and was considered to be clinically relevant since vision was affected; however, follow-up arrangement was interrupted due to personal reasons of the subject and commencement of the COVID pandemic. The significant lens decentration observed at the 18-month visit could have changed the lens–cornea relationship. This could lead to a tight fit at the peripheral, resulting in mechanical trauma, which might contribute to the oedema observed. shows a grading scale for lens decentration, based upon observations in the present study, as well as reports of successful orthokeratology wearers and LASIK procedures.Citation8–10
Table 3. Grading scale for orthokeratology lens decentration
The lens care regime was reviewed and there was no change in solution use during the 18 months of follow-up. The subject was using a povidone iodine-based care solution and hence, the situation was unlikely to be solution related.
Uneven distribution of fluid beneath the lens may also contribute, either by exerting force on the cornea or reducing oxygen transmissibility where there is a thickening of the tear film. Before the COVID-19 pandemic, the subject wore lenses around 8–9 hours every night. However, with school suspension, lenses were worn at least 12 hours every night for more than one month prior to the day of examination. The longer hours of sleep with the lenses on may have exacerbated corneal metabolic stress. Additionally, the corneal findings were greater than normally observed (5-7% swelling in the afternoon) and there was an inadequate eye-opening period during the day, making it difficult to dissipate the overnight swelling. It is unclear when the severe decentration and cornel oedema commenced, as the subject did not report any symptoms. Cumulative effects of the above-listed factors are thought to have led to the significant corneal haze and oedema observed on the day of examination.
In conclusion, although overnight lens wear may be initially successful, corneal oedema may develop for extraneous reasons. Therefore, the use of higher oxygen permeability lenses and frequent aftercare visits would be prudent, to provide a ‘safety net’ for the wearer and to ensure early detection of adverse ocular pathology. Practitioners are advised to reinforce the importance of proper lens wear habits, as this will further reduce the risk of complications.
Acknowledgements
The authors are grateful to Precision Technology Services (Canada) and Ophtecs Corporation (Japan) for sponsoring the lenses and contact lens care solutions, respectively.The work was supported by The Hong Kong Polytechnic University Research Residency Scheme of the School of Optometry.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Keay L, Sweeney DF, Jalbert I, et al. Microcyst response to high Dk/t silicone hydrogel contact lenses. Optom Vis Sci. 2000;77:582–585.
- Efron N. Epithelial microcysts. In: Efron N, editor. Contact lens complications. 4nd ed. Philadelphia: Elsevier; 2019. p. 210–215.
- Rah MJ, Jackson JM, Jones LA, et al. Overnight orthokeratology: preliminary results of the lenses and overnight orthokeratology (LOOK) study. Optom Vis Sci. 2002;79:598–605.
- Cho P, Cheung SW. Retardation of myopia in orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012;53:7077–7085.
- Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, et al. Orthokeratology vs. spectacles: adverse events and discontinuations. Optom Vis Sci. 2012;89:1133–1139.
- Hiraoka T, Kakita T, Okamoto F, et al. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: a 5-year follow-up study. Invest Ophthalmol Vis Sci. 2012;53:3913–3919.
- Harvitt DM, Bonanno JA. Re-evaluation of the oxygen diffusion model for predicting minimum contact lens Dk/t values needed to avoid corneal anoxia. Optom Vis Sci. 1999;76:712–719.
- Tsai YY, Lin JM. Ablation centration after active eye-tracker-assisted photorefractive keratectomy and laser in situ keratomileusis. J Cataract Refract Surg. 2000;26:28–34.
- Hiraoka T, Mihashi T, Okamoto C, et al. Influence of induced decentered orthokeratology lens on ocular higher-order wavefront aberrations and contrast sensitivity function. J Cataract Refract Surg. 2009;35:1918–1926.
- Yang X, Gong X, Dai Z, et al. Topographical evaluation on decentration of orthokeratology lenses. Zhonghua Yan Ke Za Zhi. 2003;39:18–21.
