ABSTRACT
Clinical Relevance
Reducing the time between drop instillation and refraction reduces the time paediatric patients and young adults spend in practice, facilitating more eye examinations daily.
Background
The current procedure for paediatric cycloplegic refraction is to wait for at least 30-minutes post-instillation of a cycloplegic before measuring spherical equivalent refraction. This study compared cycloplegia at 20- and 30-minutes following 0.5% proxymetacaine and 1.0% cyclopentolate in 12-13-year-olds.
Methods
Participants were 99 white 12-13-year-olds. One drop of proxymetacaine hydrochloride (Minims, 0.5% w/v, Bausch & Lomb, UK) followed by one drop of cyclopentolate hydrochloride (Minims, 1.0% w/v, Bausch & Lomb, UK) was instilled into both eyes. Spherical equivalent refraction was measured by autorefraction (Dong Yang Rekto ORK-11 Auto Ref-Keratometer) at 20- and 30-minutes post-instillation. Data were analysed through paired t-testing, correlations, and linear regression analysis.
Results
There was no significant difference in level of cycloplegia achieved at 20- (Mean spherical equivalent refraction (standard deviation) 0.438 (1.404) D) and 30-minutes (0.487 (1.420) D) post-eyedrop instillation (t (98) = 1.667, p = 0.099). The mean spherical equivalent refraction difference between time points was small (0.049 (0.294) D, 95% confidence interval =-0.108 ̶ 0.009D). Agreement indices: Accuracy = 0.999, Precision = 0.973, Concordance = 0.972. Spherical equivalent refraction at 20- and 30-minutes differed by ≤0.50D in 92% of eyes, and by <1.00D in 95%.
Conclusions
There was no clinically significant difference in spherical equivalent refraction or level of cycloplegia at 20- and 30-minutes post-eyedrop instillation. The latent time between drop instillation and measurement of refractive error may be reduced to 20 minutes in White 12-13-year-olds and young adults. Further studies must determine if these results persist in younger children and non-White populations.
Introduction
Cyclopentolate hydrochloride is an antimuscarinic agent used routinely in optometric practice to induce cycloplegia to accurately measure refractive error in children and young adults up to 20 years old,Citation1 and conduct a thorough fundus examination.Citation2 It temporarily paralyses the ciliary body to suspend the accommodative system, hence achieving cycloplegia and the iris sphincter muscle to achieve pupil dilation.Citation3 This is particularly important in paediatric settings as the accommodative system is highly active in children; the measured refractive error without cycloplegia may be skewed towards myopia or lower degrees of hyperopia.Citation4 The most commonly used concentration is 1.0%, but it is available in concentrations of 0.5% and historically 2.0%.Citation3,Citation5 The duration of action of cyclopentolate hydrochloride 1.0% ranges from 15 minutes to 24 hours following administration, with maximum cycloplegic effect achieved between 30–50 minutes.Citation5,Citation6
Proxymetacaine hydrochloride 0.5% (also known as proparacaine hydrochloride) may be instilled before cyclopentolate hydrochloride to improve corneal permeability and allow more cyclopentolate hydrochloride to reach the anterior chamber receptor sites, enhancing the efficacy of the cycloplegic agent.Citation7 It also anaesthetises the cornea, reducing the discomfort caused by cyclopentolate hydrochloride.Citation8 This is beneficial for patient and practitioner relationships, as the instillation of the cycloplegic agent is less traumatic for young patients, and the active compound is not diluted by reflex tearing.Citation9–11 Although proxymetacaine hydrochloride can cause stinging, Sutherland et al.Citation8 showed it was nearly four times less painful than cyclopentolate hydrochloride upon instillation. Proxymetacaine hydrochloride is reported to cause less discomfort than other topical anaesthetics, such as oxybuprocaine hydrochloride 0.4%, possibly due to its less acidic pH.Citation12 Adverse reactions to 0.5% proxymetacaine hydrochloride are very rare; however, instillation may cause conjunctival irritation or an allergic-type corneal response if the patient is sensitive to the compound (including diffuse epithelial keratitis, a grey ground-glass corneal appearance, or the presence of corneal filaments).Citation13
In practice, clinicians are advised to wait for 30-minutes post-instillation of cyclopentolate hydrochloride 1.0% before measuring refractive error in children and young adults, even with pre-instillation of proxymetacaine hydrochloride 0.5%.Citation14 As a result, patients and their parents/legal guardians spend more time in the practice, which limits the number of patients examined daily. If there is no clinically significant difference between the level of achieved cycloplegia at 20- and 30-minutes, in that case, an argument could be made for reducing the recommended waiting period between instillation of cyclopentolate hydrochloride (and pre-instillation of proxymetacaine hydrochloride) and the eye examination to 20 minutes. This study aims to ascertain the time to total efficacy of cyclopentolate hydrochloride 1.0% enhanced by the prior instillation of the topical anaesthetic proxymetacaine hydrochloride 0.5% in white 12-13-year-olds.
Methods
Ethical considerations
This study formed part of the Ireland Eye Study,Citation15 and ethical approval was granted by the Technological University Dublin Research Ethics Committee. All research activities adhered to the tenets of the Declaration of Helsinki. Prior to data collection, the principal investigator discussed the effects of eyedrops on class and sports participation for 24 hours following eyedrop instillation. Information packs, including a storyboard to make the study accessible to children were provided to participants and their parents/legal guardians. Informed assent and consent were obtained from the participants and their parents/legal guardians. Participants were provided with disposable sunglasses to aid with cycloplegia-induced light sensitivity.
Data collection
Presented data were collected in September to October 2016 from 99 Ireland Eye Study participants. Participants were white 12-13-year-old school children. Participants were tested during the school day on school premises once written informed parental consent, and child assent were obtained. One drop of proxymetacaine hydrochloride (Minims, 0.5% w/v, Bausch & Lomb, UK, https://www.bausch.com/) followed two minutes later by one drop of cyclopentolate hydrochloride (Minims, 1.0% w/v, Bausch & Lomb, UK, https://www.bausch.com/) were instilled in each eye. Following eyedrop instillation, participants were advised to close their eyes, and nasolacrimal occlusion was applied by the clinician to reduce systemic absorption.Citation14 Participants were advised to wash their hands following administration. Refractive error was measured by cycloplegic autorefraction (Dong Yang Rekto ORK-11 Auto Ref-Keratometer, Everview, Seoul, Korea) at 20- and 30-minutes following 1.0% cyclopentolate HCL instillation. Hence, two measurements of refractive error were obtained in both eyes of 99 participants aged 12-13-years. The same optometrist performed both refractive error measurements using the same autorefractor, and in all instances, the right eye was measured first. Spherical equivalent refraction (SER) (sphere + (cylinder/2)) was analysed for this study.
Statistical methodology
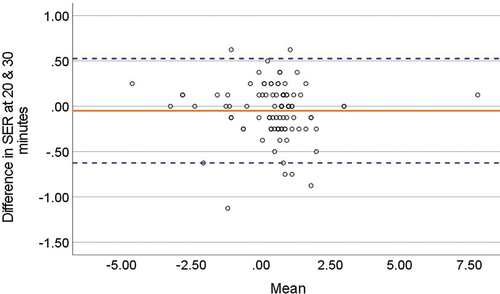
Anonymised data were entered into a Statistical Package for Social Sciences V.28.0 (SPSS) (IBM Corp, Armonk, NY, USA) spreadsheet. SER data were non-normally distributed (Kolmogorov-Smirnov test, p < 0.05); however, these data were continuous, linear, the mean was the centre of the distribution, and the sample size was large enough to invoke the central limit theoremCitation16; hence, SER data were compared at 20- and 30-minutes post-instillation using linear regression analysis to assess the relationship between refractive error measured at 20- and 30-minutes post-instillation of cycloplegia (). Parametric testing was deemed appropriate as the clinical relevance of the results can be examined more readily than with a non-parametric test.Citation16 In addition, a two-tailed paired t-test was used to compare the mean (standard deviation (SD)) SER at 20- and 30-minutes. As the paired t-test may fail to detect poor agreement in pairs of data when the means are equal,Citation17 concordance analysis (Bland Altman plots and the clinical concordance coefficient (CCC)) was also employed (). The CCC is a measure of distance from the 45-degree line (perfect agreement y=x) and therefore quantifies the (dis)agreement between the two sets of observations (see supplementary Table S1 for additional information). Confidence intervals (CI) were 95% and a p-value of <0.05 was considered significant. Equivalence and non-inferiority testing were performed. Two one-sided tests (TOST) were carried out for the 20- and 30-minute SER measurements in SPSS, and the calculated means and standard deviations were entered into an effect size calculator to determine 90% CI for the SER measurements at the two time points.
Figure 1. Scatter plot of spherical equivalent refraction (SER) measures in dioptres (D) at 20-minutes (y-axis) and 30-minutes (x-axis). The best fitting regression line (solid line) and also the y=x line (dotted line) are overlaid to quantify the extent of (dis)agreement between spherical equivalent refraction measured at 20-minutes and 30-minutes post-instillation of cycloplegic eyedrops.
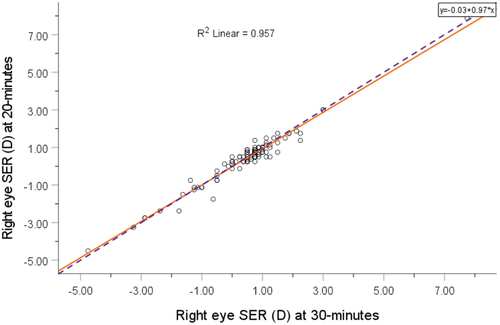
Figure 2. A plot presenting the equivalence bounds (−0.50, 0.50) in relation to the 90% confidence interval (−0.296, 0.366). As the 90% confidence interval values are within the equivalence bounds, this signifies equivalence of the 20- and 30-minute SER measurements.
Figure 3. Bland-Altman plot of the difference in mean readings at 20- and 30-minutes post-instillation of one drop of 0.5% proxymetacaine hydrochloride followed by one drop of 1.0% cyclopentolate hydrochloride. The solid line represents the mean difference, and the dotted lines represent upper and lower 95% confidence intervals.
Results
Data were collected from both the right and left eyes of each participant. There was no significant difference in SER between right and left eyes (Pearson’s correlation coefficient r = 0.946, r < 0.001 at 20-minutes, r = 0.933, r < 0.001 at 30-minutes). Hence, right eye data only are presented. Supplementary Table S1 presents left eye data, and Table S2 presents results for both the right eye and left eye combined. Summary statistics of the group mean (SD) spherical equivalent refraction at 20-minutes was 0.438 (1.404) D (r = 99, range −4.50 to 7.875 D). The group mean (SD) spherical equivalent refraction at 30-minutes was 0.487 (1.420) D (r = 99, range −4.75 to 7.75 D). The mean difference in individual eye SER taken at 20- and 30-minutes was ±0.049 (0.294) D. The 95% CI’s of the mean difference were (0.043 to 0.055). There was no statistically significant difference in cycloplegic refraction measured at 20- 30-minutes (paired t-test: mean difference (standard deviation (SD)) = 0.049 (0.294); t = 1.667; df = 98; p = 0.099).
Comparing agreement of SER measured at 20- and 30-minutes was examined using agreement indices. The agreement indices were as follows: Accuracy = 0.999, Precision = 0.973 (), and Concordance = 0.972. Measurements of SER taken at 20- and 30-minutes were strongly correlated (Pearson correlation coefficient r = 0.978, r < 0.001, solid line representing the linear regression best-fit line, r2 = 0.957).
Furthermore, as the CCC = 0.972, the two sets of measurements are equivalent as a CCC = 1.00 indicates perfect agreement with measurements y=x. displays SER measurements taken at 20-minutes (y-axis) and 30-minutes (x-axis) with y=x line (dotted line − 45-degree line) overlaid (indicating near-perfect agreement). As can be seen, there is little scatter about the y=x line; furthermore, the best fitting regression line (solid line ) closely aligns with the y=x concordance line (dotted line ).
There was no statistically significant difference in SER at 20- and 30-minutes in hyperopic (SER≥+2.00) (paired t-test: mean difference (standard deviation (SD)) = −0.250 (0.379); t =-1.615; df = 5; t = 0.167), myopic (SER≤-0.50D)(−0.049 (0.372); t = −0.555; df = 17, t = 0.586) or emmetropic (−0.50<SER<+2.00D) participants (−0.033 (0.263); t = −1.096; df = 74; t = 0.277). Comparison of SER at 20- and 30-minutes in both right and left eyes of each participant (t = 99, 198 eyes) was performed and is detailed in supplementary Figures S1-4(c), and supplementary Tables S3(a – e). These findings indicate no additional benefit in waiting for 30-minutes compared to 20-minutes before refraction.
Upper and lower bounds of +0.50 and −0.50D respectively were chosen for equivalence testing. Using the TOST method, means and standard deviations (mean (SD)) for 20-minute (0.438(1.404)) and 30-minute (0.487(1.420)) measurements were calculated (). Both values of the 90% CI (−0.296, 0.366) were within ±0.50D, meaning that the SER measurements at 20- and 30-minutes were equivalent.
presents the Bland Altman plot, which was constructed to display the relationship between the measurements taken at 20- and 30-minutes and to determine the 95% limits of agreement. The Bland Altman plot () demonstrates that the two measurements were in close agreement as the mean-of-all-differences line is very close to zero. The SER at 20- and 30-minutes differed by ≤0.50D in 92% of eyes and by <1.00D in 95%, as seen in . Therefore, there appears to be no systematic difference in 20- and 30-minute SER measurements.
Discussion
This study demonstrated no statistical or clinically significant difference in refractive error measured 20- and 30-minutes post instillation of proxymetacaine hydrochloride 0.5% followed by cyclopentolate hydrochloride 1.0%, in White 12-13-year-olds. Clinical significance refers to how much of an effect the results would have on clinical practice, whereas statistical significance refers to the reliability of the results, considering, for example, sample size and p-values. In the optometric context, a measured difference in SER of ≤0.50D is deemed clinically insignificant; any difference of 0.50D or less is insignificant and does not affect the patient. In this study, 92% of participants satisfied this criterion. The findings for participants whose SER was within ±3.00D were similar to those with more extreme SER, suggesting that the findings are transferrable to larger prescriptions. However, further research including more participants with prescriptions exceeding +6.00D is indicated as Al-Omari et al.Citation18 showed that most highly hyperopic, brown-eyed patients only achieved maximum cycloplegia 45 minutes following the instillation of the first of two drops of cyclopentolate hydrochloride 1.0%. Most highly myopic patients (≤-6.00D) achieved maximum cycloplegia 30-minutes following cyclopentolate hydrochloride instillation.Citation18 Al Omari et al.Citation18 did not pre-instil topical anaesthetic, warranting further research into the effect of proxymetacaine hydrochloride 0.5% on the efficacy of cyclopentolate hydrochloride 1.0% in highly hyperopic paediatric patients.
Autorefraction repeatability
Cycloplegic refractive error values have been found to be repeatable across various autorefractors with different mechanisms of measurement.Citation19,Citation20 The repeatability of four autorefractors with various measurement principles were compared by Padhy et al.Citation19 and Moore et al.Citation20 These studies reported that repeated measures of refractive error were within ±0.81D of each other across different autorefractors. As the autorefractor used in the current study was a conventional autorefractor, the limits of agreement from the aforementioned studies (±0.81D) were extended to the present study in the absence of a specific repeatability study. The findings of these studies support the statistically insignificant differences observed in SER between 20- and 30-minutes, as minor differences between measurements may in part be due to instrument repeatability. The current study findings suggest that for white 12-13-year-olds, waiting for only 20-minutes allows a sufficient level of cycloplegia to obtain an accurate refractive measurement once proxymetacaine hydrochloride 0.5% is instilled before cyclopentolate hydrochloride 1.0%. The present study demonstrates that waiting an additional 10-minutes after eyedrop instillation does not increase the level of cycloplegia; in some instances, the 30-minute reading was either slightly less hyperopic than the 20-minute reading or more hyperopic by an insignificant amount.
Corneal absorption
The corneal epithelium provides an effective barrier to topical medications, with <5% of active ingredients penetrating the anterior chamber.Citation21 Proxymetacaine hydrochloride 0.5% increases corneal permeability, improving the intraocular bioavailability of cyclopentolate hydrochloride. This may occur due to transient corneal epithelial damage caused by proxymetacaine hydrochloride and alterations to corneal epithelial adhesions.Citation22–25 Another mechanism by which the prior instillation of proxymetacaine hydrochloride may improve the efficacy of cyclopentolate hydrochloride is by reducing reflex tearing, which is stimulated by the stinging sensation induced by cyclopentolate hydrochloride.Citation8,Citation23 Dilution and drainage of the active ingredient is decreased following anaesthetic, increasing both the volume of the active ingredient, as well as corneal contact time.Citation8,Citation23 Approximately 90% of the active ingredient is lost to nasolacrimal drainage if light pressure is not applied to the puncta following eyedrop instillation.Citation21 Haddad et al.Citation11 reported the instillation of one drop of proxymetacaine hydrochloride 0.5% did not enhance the mydriatic effects of tropicamide 0.5%. Due to tropicamide being a largely non-ionised compound, it is more readily absorbed by the cornea than cyclopentolate hydrochloride; hence, proxymetacaine hydrochloride does not potentiate absorption of tropicamide hydrochloride as much as cyclopentolate hydrochloride.Citation23 The cycloplegic effect was not analysed by Haddad et al. A limitation of the current study is that pupil size was not noted at either timepoint or before eyedrop instillation. Mydriasis has been shown to lag behind cycloplegia, meaning that the pupil may not be fully dilated at the point at which cycloplegia is achieved.Citation26
Ideally, the fellow eye would be included without prior instillation of 0.5% proxymetacaine hydrochloride as a control, however 1.0% cyclopentolate hydrochloride instillation without prior instillation of topical corneal anaesthesia has been linked to children having a negative experience during an eye examination.Citation10 Additionally, cyclopentolate hydrochloride concentration may differ between anaesthetised and non-anaesthetised eyes due to reflex tearing and subsequent dilution due cyclopentolate-induced stinging. This might impact the comparison of fellow eyes where one eye receives 1.0% cyclopentolate hydrochloride alone with the fellow pre-anaesthetised eye, as there is no guarantee that fellow eyes receive the same amount of 1.0% cyclopentolate hydrochloride despite fellow eyes receiving an equal amount of 1.0% cyclopentolate hydrochloride eyedrops.
Pigmentation
The present study findings may not be applicable to all children seen in optometric practice. Laojaroenwanit et al.Citation6 found that Asian children (aged 5-14-years-old) with darkly pigmented irides only achieve maximal cycloplegia 30-minutes post-instillation of three drops of cyclopentolate hydrochloride 1.0% instilled 10 minutes apart. However, the effects of pre-instillation of topical anaesthetic on cycloplegia were not studied. Kyei et al.Citation9 found that one drop of cyclopentolate hydrochloride 1.0% could achieve cycloplegia in a population (aged 15-24-years-old) with darkly pigmented irides. Still, maximal cycloplegia was only achieved after 90-minutes, and cycloplegic effects persisted for eight hours or more.Citation9 This delay and subsequent persistence in cycloplegic effect were due to iris melanin binding with antimuscarinic compounds and releasing them slowly over time.Citation27 However, topical anaesthetic was not used before the instillation of cyclopentolate hydrochloride, which may have delayed cycloplegic effects further. A study involving an Asian population (aged 19-25-years-old) with darkly pigmented irides found that instillation of topical anaesthetic oxybuprocaine hydrochloride 0.4% reduced the time at which 95% cycloplegia was achieved by 8.85 minutes on average.Citation28 LovasikCitation29 showed that blue eyes experienced a deeper and more rapid depth of cycloplegia following cyclopentolate hydrochloride 1.0% compared to brown eyes. It was found that the preinstallation of proparacaine hydrochloride reduced the time between cyclopentolate hydrochloride administration and cycloplegia in adult participants.Citation29 A limitation of the current study is that eye colour was not noted. However, white European populations have a higher prevalence of lighter-coloured eyes compared to Asian ethnicities, and darker irides are more common among Asian and African populations.Citation30 Further research involving paediatric and young adult participants with darkly pigmented irides is indicated to ascertain appropriate time frames to maximal cycloplegia with prior instillation of topical anaesthetic.
Accommodation
It is well known that non-cyclopleged refraction results in a more myopic refraction in children and young adults up to 20 years of age due to active accommodation.Citation1 However, younger children have a larger amplitude of accommodation (AA) than teenagers and adults. One study found that children between 6-10-years of age have a median AA of 15.5D, whereas 15-year-olds have a median AA of 12.9D.Citation31 Manny et al.Citation26 showed that cycloplegia may be achieved in adults with light irides in 10-minutes. Spherical equivalent refraction was not reported nor compared between timepoints, as the measurement of residual accommodation was the marker for the level of cycloplegia.Citation26 A small sample (n = 4) of children aged 9–11 years with light irides achieved similar cycloplegia to their adult counterparts at 10-minutes, but meaningful analysis of these results was precluded by the small sample size.Citation26 Access to ample accommodation can artificially reduce hyperopic prescriptions or increase myopic prescriptions if children are refracted without cycloplegia, which may lead to errors in correction. Due to the higher levels of active accommodation in younger children, further research is indicated on the effectivity of cyclopentolate hydrochloride 1.0% at 20- and 30-minutes post-instillation of proxymetacaine hydrochloride 0.5% on younger age groups to determine whether the clinically insignificant difference in the level of cycloplegia at these time points in 12-13-year-olds persists in younger patients.
Time between eyedrops and refraction
The results of the current study indicate that it may be suitable to reduce the wait time between drop instillation and the measurement of refractive error from 30-minutes to 20-minutes in white 12-13-year-olds once temporary obstruction of the nasolacrimal channel following the instillation of proxymetacaine hydrochloride 0.5% and cyclopentolate hydrochloride 1.0% is practiced. One study investigating the effect of reducing the time of a patient visit by six minutes in a primary care clinic found that this small reduction improved patient satisfaction and allowed more patients to attend care per day.Citation32 This may apply to eye care practices as 10 minutes would be gained per appointment for patients up to the age of twenty, as evidence suggests that refraction results may be artificially more myopic due to active accommodation in teenagers.Citation1 From a public health perspective, this information is vital in streamlining paediatric eye care provision, conveniently reducing the time patients and their guardians spend in the practice, allowing more children and young adults to be examined daily, and improving the efficiency of the current system.
Conclusions
The present study demonstrates that refractive results obtained 20-minutes post-instillation of 0.5% proxymetacaine hydrochloride followed by 1.0% cyclopentolate hydrochloride are highly comparable to those obtained at 30-minutes post-instillation in white 12-13-year-old children. Thus, these results suggest that it is possible to establish accurate refraction results 20-minutes instead of 30-minutes post-instillation of proxymetacaine hydrochloride 0.5% and cyclopentolate hydrochloride 1.0%. This information is relevant to streamlining the delivery of paediatric and adolescent eyecare worldwide. Further research involving younger white and non-white populations is indicated to ascertain whether this clinically insignificant refractive difference is consistent at these time points in younger participants with more active accommodation and those with highly pigmented irides.
Table 1
Download PDF (86.8 KB)Table 2
Download PDF (65.7 KB)Table 3
Download PDF (117 KB)Table 4
Download PDF (65.4 KB)Supplementary Figures 1, 2, 3
Download PDF (363.7 KB)Supplementary Figures 4, 5
Download PDF (162.1 KB)Acknowledgment
The authors would like to thank Professor Kathryn Saunders (NICER study, School of Biomedical Sciences, University of Ulster, County Londonderry, Northern Ireland), Dr Jim Stack (Biostatistician Waterford Institute of Technology) and Professor John Kearney (Epidemiology, Technological University Dublin) for their valuable input in the Ireland Eye Study. In addition, the authors would like to acknowledge the support and participation of the schools, the children, and their parents and guardians in the Ireland Eye Study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/08164622.2023.2166398
Additional information
Funding
References
- Sanfilippo PG, Chu BS, Bigault O et al. What is the appropriate age cut-off for cycloplegia in refraction? Acta Ophthalmol 2014; 92: 458–462.doi:10.1111/aos.12388.
- Bausch & Lomb. Minims cyclopentolate hydrochloride 1%, Eye drops solution - Summary of product characteristics (SmPC) [Internet]. medicines.org.uk. 2021 [cited 2021 Dec 13]. Available from: https://www.medicines.org.uk/emc/product/4258/smpc#gref
- Jones LWJ, Modes DT. Possible allergic reactions to cyclopentolate hydrochloride: case reports with literature review of uses and adverse reactions. Ophthalmic Physiol Opt 1991; 11: 16–21. doi:10.1111/j.1475-1313.1991.tb00189.x.
- Funarunart P, Tengtrisorn S, Sangsupawanich P et al. Accuracy of noncycloplegic refraction in primary school children in Southern Thailand. J Med Assoc Thai [Internet] 2009; 92: 806–812. [cited 2022 Jan 24] Available from: http://www.mat.or.th/journal
- Health Products Regulatory Authority Summary of Product Characteristics [Internet]. 2020 [cited 2021 Dec 14]. Available from: https://www.hpra.ie/img/uploaded/swedocuments/Licence_PA22709-003-001_03122020100947.pdf
- Laojaroenwanit S, Layanun V, Praneeprachachon P et al. Time of maximum cycloplegia after instillation of cyclopentolate 1% in children with brown irises. Clin Ophthalmol [Internet] 2016 May 18; 10: 897–902. [cited 2021 Dec 13]. Available from: https://www.dovepress.com/time-of-maximum-cycloplegia-after-instillation-of-cyclopentolate-1-in–peer-reviewed-fulltext-article-OPTH
- Talley DK, Bartlett JD. Topical and regional anesthesia. In: Bartlett J Jaanus S, editors. Clinical Ocular Pharmacology. 5th ed. St Louis: Butterworth-Heinemann; 2008. p. 322.
- Sutherland S, Young J. Does instilling proxymetacaine before cyclopentolate significantly reduce stinging? The implications for paediatric cycloplegia [letter]. Br J Ophthalmol [Internet] 2001; 85: 244. [cited 2022 Feb 16]. Available from www.bjophthalmol.com
- Kyei S, Nketsiah AA, Asiedu K et al. Onset and duration of cycloplegic action of 1% cyclopentolate — 1% tropicamide combination. Afr Health Sci [Internet] 2017; 17; 923–932. [cited 2021 Dec 14]. Available from: /pmc/articles/PMC5656211/
- Shah P, Jacks AS, Adams GGW. Paediatric cycloplegia: a new approach. Eye [Internet] 1997; 11: 845–846. [cited 2022 Feb 21]. Available from: https://www.nature.com/articles/eye1997216
- Haddad DE, Rosenfield M, Portello JK et al. Does prior instillation of a topical anaesthetic alter the pupillary mydriasis produced by tropicamide (0.5%)? Ophthalmic Physiol Opt 2007; 27: 311–314. doi:10.1111/j.1475-1313.2007.00472.x.
- Lawrenson JG, Edgar DF, Tanna GK et al. Comparison of the tolerability and efficacy of unit-dose, preservative-free topical ocular anaesthetics. Ophthalmic Physiol Opt 1998; 18: 393–400. doi:10.1046/j.1475-1313.1998.00381.x.
- Bausch & Lomb U.K Limited. Minims proxymetacaine hydrochloride 0.5% w/v, eye drops solution [Internet]. Electronic Medicines Compendium. 2016. Available from: https://www.medicines.org.uk/emc/product/3745/smpc#gref
- College of Optometrists’ Formulary [Internet]. 2016. Available from: http://www.wolvesloc.net/media/3891/college-formulary.pdf
- Harrington SC, Stack J, Saunders K et al. Refractive error and visual impairment in Ireland schoolchildren. Br J Ophthalmol Internet 2019 Aug 1; 103: 1112–1118. [cited 2022 Apr 21]. Available from: https://pubmed.ncbi.nlm.nih.gov/30315130/
- le Cessie S, Goeman JJ, Dekkers OM. Who is afraid of non-normal data? Choosing between parametric and non-parametric tests. Eur J Endocrinol 2020 Feb 1; 182: E1–3. [cited 2022 May 16]. Available from: https://eje.bioscientifica.com/view/journals/eje/182/2/EJE-19-0922.xml
- Lin L-K. A concordance correlation coefficient to evaluate reproducibility. Biometrics 1989; 45: 255. doi:10.2307/2532051.
- Al-Omari R, Atoum D, Khader Y et al. Time for effective cycloplegia in patients with brown iris. Strabismus [Internet] 2022 Jan 6; 30: 29–34. [cited 2022 Nov 3]. Available from: https://www.tandfonline.com/doi/pdf/10.1080/09273972.2021.2022716?casa_token=CzyZuwpUhX4AAAAA:f0QMi0Fy5r_kD-to-bfSOBlknID9jcZD5IUDF7_ek0tT6okkuubu3JKBA-61uGcAitdqi0brEk_i
- Padhy D, Bharadwaj SR, Nayak S et al. Does the accuracy and repeatability of refractive error estimates depend on the measurement principle of autorefractors? Transl Vis Sci Technol [Internet] 2021 Jan 1; 10: 1–11. [cited 2022 Apr28] /pmc/articles/PMC7794271/
- Moore KE, Berntsen DA. Central and peripheral autorefraction repeatability in normal eyes. Optom Vis Sci [Internet] 2014; 91: 1106. [cited 2022 Apr 25]. Available from: /pmc/articles/PMC4142103/
- Cholkar K, Dasari SR, Pal D et al. Eye: anatomy, physiology and barriers to drug delivery. In: Mitra A, editor. Ocular transporters and receptors: their role in drug delivery. Cambridge: Woodhouse Publishing;2013. pp. 1–36.
- Brewitt H, Bonatz E, Honegger H. Morphological changes of the corneal epithelium after application of topical anaesthetic ointments. Ophthalmologica 1980; 180: 198–206. doi:10.1159/000308974.
- Apt L, Henrick A. Pupillary dilatation with single eyedrop mydriatic combinations. Am J Ophthalmol [Internet] 1980; 89; 553–559. doi:http://dx.doi.org/10.1016/0002-9394(80)90065-3.
- Herse P, Siu A. Short-term effects of proparacaine on human corneal thickness. Acta Ophthalmol [Internet] 1992 May 27; 70: 740–744. doi:10.1111/j.1755-3768.1992.tb04879.x.
- Moiseev RV, Morrison PWJ, Steele F et al. Penetration enhancers in ocular drug delivery. Pharmaceutics [Internet] 2019 Jul 1; 11: 321. [cited 2022 Feb 28]. Available from: /pmc/articles/PMC6681039/
- Manny RE, Fern KD, Zervas HJ et al. 1% cyclopentolate hydrochloride: another look at the time course of cycloplegia using an objective measure of the accommodative response. Optom Vis Sci [Internet] 1993; 70: 651–665. https://pubmed.ncbi.nlm.nih.gov/8414387/
- Gunawan F, Irfani I, Memed FK et al. Comparison of cycloplegic and mydriatic effect between cyclopentolate, tropicamide, and combination in children : a narrative review. Bali J Ophthalmol 2021; 5: 1–6.
- Siu AW, Sum AC, Lee DT et al. Prior Topical anaesthesia reduces time to full cycloplegia in Chinese. Jpn J Ophthalmol 1999; 43: 466–471. doi:10.1016/S0021-5155(99)00113-6.
- Lovasik J. Pharmacokinetics of topically applied cyclopentolate HCL and tropicamide. Am J Optom Physiol Opt [Internet] 1986 Oct; 63: 787–803. [cited 2022 Nov 3]. Available from: https://pubmed.ncbi.nlm.nih.gov/3777109/
- Katsara MA, Nothnagel M. True colors: a literature review on the spatial distribution of eye and hair pigmentation. Forensic Sci Int Genet 2019 Mar 1; 39: 109–118. doi:10.1016/j.fsigen.2019.01.001.
- Castagno VD, Vilela MAP, Meucci RD et al. Amplitude of accommodation in schoolchildren. Curr Eye Res [Internet 2016; 42: 604–610. doi:http://dx.doi.org/10.1080/02713683.2016.1220586.
- Robinson J, Porter M, Montalvo Y et al. Losing the wait: improving patient cycle time in primary care. BMJ Open Qual [Internet] 2020; 9: e000910. doi:10.1136/bmjoq-2019-000910.
