ABSTRACT
Purpose
Corneal perforations are common corneal emergencies faced by ophthalmologists across the globe. There are multiple modalities of management, most of which require an eye bank support or availability of tissue adhesives. Tenon's patch graft (TPG) is a technique that does not depend on these factors as the graft is harvested from the same eye of the patient. The aim of this review is to provide an overview of the indications, technique, normal postoperative course, and management of complications.
Methods
After carrying out a literature search on “tenon's capsule”, “corneal patch graft”, “tenon's patch graft”, “multilayered amniotic membrane” and “corneal perforations”, 28 articles were included for this review.
Results
TPG graft can be performed in cases of small to moderate perforations without active suppuration. The procedure can also be combined with amniotic membrane grafting or tissue adhesives to provide additional tectonic support. Postoperatively, the epithelium heals over a course 2–3 weeks and restoration of a stable ocular surface with a corneal scar is completed by the third postoperative month. Complications following the surgical procedure are rare but can include graft displacement, melt and pseudoectasia. Subsequent visual rehabilitation with contact lenses or keratoplasties can be planned in these eyes that yields good visual outcomes.
Conclusions
Tenon's patch graft is a simple yet viable option in management of small to moderate corneal perforations. The procedure does not necessitate the prior availability of specialized products and can be performed with routine equipment of an ophthalmic theatre, making it an attractive option in low resource settings.
Introduction
Corneal perforations often have myriads of clinical presentations and are usually associated with a variety of underlying clinical diagnoses.Citation1,Citation2 They contribute significantly to the overall burden of blindness due corneal pathologies. Their management is dependent upon the size of the perforation, its location, the involvement of the surrounding ocular structures and the severity of the causal disease. The primary purpose of any surgical intervention in these cases is the restoration of the tectonic support of the eye and the reformation of a watertight anterior chamber. A number of surgical options are available and often more than one procedure can be utilized to seal the perforation and render the globe tectonically stable. These include the use of tissue adhesives with bandage contact lenses (BCL), conjunctival flaps, amniotic membrane (AM) grafting, corneal patch grafts and penetrating keratoplasties.Citation3–5 One of the techniques in this armamentarium is a tenon's patch graft (TPG).
A tenon's graft is harvested from the same eye of the patient and thus obviates the need for procurement or storage.Citation6,Citation7 This is the biggest advantage of the technique given the emergent nature of perforations of the cornea. The earliest use of autologous tenon's capsule was described to address leaking blebs following glaucoma filtering surgeries.Citation8 Its use in the management of corneal perforations was first elucidated by Vajpayee in 2012, in cases with small to medium-sized perforations.Citation9 A few subsequent case series and reports have demonstrated the efficacy of this procedure in the restoration of a formed globe.Citation7,Citation10–13 This review aims to provide a comprehensive understanding of the process of case selection for this procedure, the surgical technique, the natural course of healing and the outcomes of TPG.
Method of review
Literature searches for this review were completed using PubMed, in July 2021. The following keywords and their duplications were used for the searches, “tenon's capsule”, “corneal patch graft”, “tenon's patch graft”, “multilayered amniotic membrane” and “corneal perforations”. These were entered into PubMed generating 3468 related articles. From these articles we included those publications in the English language, relevant to the disease conditions listed above and a final of 28 articles were included for this literature review. The collective experience of the authors has also been added to the review.
Clinical anatomy
The tenon's capsule is a layer of connective tissue that encloses the eyeball.Citation14,Citation15 Different anatomical boundaries have been described in literature, dividing this layer into an i) anterior and posterior segment ii) anterior, mid-posterior and posterior area, based on the thickness of this fascial layer.Citation14,Citation16 Embryologically also, the anterior segment forms earlier than the posterior segment.Citation17 The components of this layer vary with the presence of smooth muscle cells in the anterior part, while the posterior segment is devoid of these cells and is formed by the condensation of fibers of collagen.Citation18–20 The insertion of the capsule is 1.5–2 mm behind the corneoscleral junctionCitation21 (). The anterior segment is thicker than the posterior segment.Citation16,Citation19 Furthermore, the anterior layer is longer in the nasal half than the temporal wherein the transition into the thinner posterior occurs earlier.Citation21 Also, adherence of the capsule to the underlying episcleral tissue is also stronger in the anterior segment when compared to the posterior one. These factors need to be taken into consideration while harvesting the graft tissue.
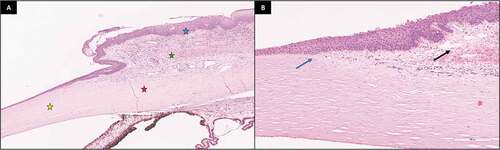
Figure 1. Histopathology images of tenon's capsule a) Low magnification image (10x) showing the lamellar collagen within the cornea (yellow star), the limbus (red star), tenon's capsule (green star) and the conjunctival epithelium (blue star) b) High magnification (40x) image depicting the insertion of the tenon's capsule (blue arrow) and the tenon's capsule (black arrow) beneath the substantia propria of the conjunctiva. Images courtesy Dr Saumya Jakati, Ophthalmic Pathology Laboratory, LV Prasad Eye Institute, Hyderabad, India.
Case selection
As mentioned earlier, a number of factors need to be taken into consideration when planning surgical intervention in a case of corneal perforation. The choice of intervention may be obvious in some cases such as perforations smaller than 1 mm requiring only tissue adhesives or very large perforations >6 mm with collagenolysis in the adjacent cornea necessitating therapeutic keratoplasties for restoring the integrity of the globe. Cases that lie between the two ends of this spectrum often pose a dilemma to the treating surgeon, as they may be amenable to more than one surgical procedure. Unless there is no access to tissue adhesive and an eye bank backup is not available, TPG is not recommended in a corneal perforation due to acute suppuration. The inflammatory cells will cause rapid degradation of the tenon's layer via secretion of proteases and other inflammatory mediators.Citation22
A TPG is primarily indicated in eyes wherein the perforation is secondary to an underlying autoimmune or neuropathic pathology and the size of the perforation is between 2 and 5 mm.Citation10,Citation11 details the etiologies wherein a TPG can be considered if a perforation occurs. As mentioned earlier, these perforations may also be sealed with tissue adhesives or AM grafts or corneal patch grafts. However, the degree of involvement of the surrounding structures will offer a distinct advantage to one procedure over the other. In cases of cicatrizing conjunctivitis, there may be extensive forniceal shortening or symblephara that make the placement of a BCL difficult. Also, the vascularization induced by tissues adhesives may not be desirable in such eyes. And so, performing a multilayered AM graft or a TPG will be the better option is these cases. However, the former may not always be available, while in case of the latter, this restriction is not there as autologous harvesting is carried out.
Table 1. List of indications for Tenon's patch graft.
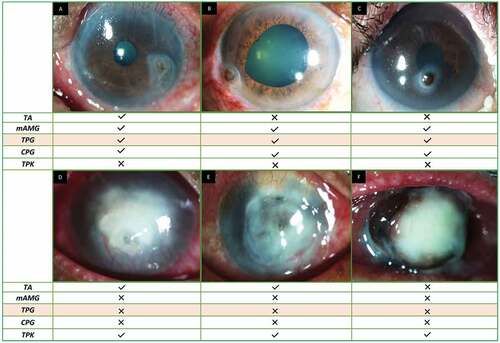
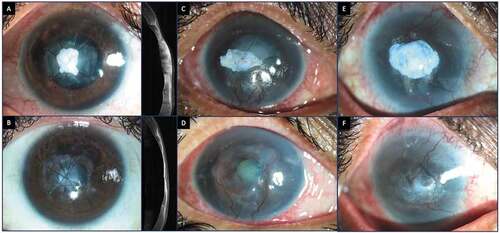
Corneal perforations can be associated with loss of corneal tissue and thus a volume deficit. Application of tissue adhesive in these perforations would only bridge the aperture and would not help replace the lost volume. Often these eyes require repeated applications of tissue adhesive with suboptimal outcomes. In these cases, a multilayered AM graft, TPG or a keratoplasty (either a patch graft or a penetrating keratoplasty) would be considered better options. However, a keratoplasty or an AM graft will require the support of a well-equipped eye bank. Also subjecting the eye to a keratoplasty will mean having to deal with risk of graft rejection and subsequent graft failure. Moreover, the follow-up of these cases is more rigorous, with use of long-term steroids, which in itself is associated with numerous side effects. As a TPG employs an autologous graft, there is no risk of tissue rejection or need for long-term corticosteroid therapy. depicts different types of corneal perforations and the various modalities that can be employed in their management, while compares and contrasts the different surgical techniques.
Table 2. This table depicts the advantages and disadvantages of different surgical options for corneal perforations.
Figure 2. Different types of corneal perforations and the various modalities that can be employed in their management. a) Paracentral small sterile perforation b) Peripheral large sterile perforation c) Central sterile perforation with shallow fornices in Stevens-Johnson syndrome d) Central perforation with microbial keratitis with active infiltration e) Central large perforation with microbial keratitis with significant collagenolysisf) Total corneal melting with pseduocornea formation. TA: Tissue adhesive, mAMG: multilayered amniotic membrane graft, TPG: tenon's patch graft, CPG: corneal patch graft, TPK: therapeutic penetrating keratoplasty.
Presurgical considerations
Preoperative Workup and Medications
Determination of the underlying cause is essential and so subjecting the patient to a detailed history and comprehensive ocular examination prior to the surgery is of utmost importance. Several cases with systemic autoimmune disorders will require a dose of intravenous immunosuppression prior to surgery. This is usually given as 500–1000 g of I V methyl prednisolone and rarely I V cyclophosphamide is also added to the regimen. Signs of an underlying neurotrophic disorder must be carefully looked for. If present a concurrent tarsorrhaphy can be planned with the patch graft. The instillation of brimonidine tartrate 0.15% eye drops results in vasoconstriction and thus ensures lesser bleeding of the donor site intraoperatively.Citation23 These drops can be instilled 5–10 minutes prior to the surgery to ensure maximum efficacy intraoperatively.
Preoperative Counselling
That the primary goal of the surgery is to reestablish a stable globe, has to be clearly explained to the patient. It is important that they understand the natural postoperative course of the procedure and the resultant scarring that ensues which may affect the visual acuity. The need for a secondary procedure for visual rehabilitation should also be explained to the patient.
Anesthesia
The surgery can be performed under topical anesthesia in case of small perforations and if the patient is deemed cooperative for the same. Peribulbar anesthesia can be administered in cases with larger perforations. The injection of the anesthetic agent into the peribulbar space must be gradual and can be done in a step wise spaced fashion. This is done to ensure there is no extension of the perforation or extrusion of intraocular contents. Ocular massage should also be avoided for the same reasons. Addition of adrenaline to the anesthetic solution decreases the systemic absorption and increases local peak concentrations.Citation24 Also, addition of hyaluronidase and bicarbonate will increase permeability and hasten the onset on action of the anesthetic agent.Citation25,Citation26 Combining these agents will help decrease the total volume of anesthetic agent administered and thus decreasing the intraorbital pressure.
Surgical technique
Harvesting the graft tissue
A small nick is made in the conjunctiva-in the superonasal or superotemporal area, 2 mm behind the limbus and the underlying tenon's is exposed (). The tenon's is then dissected and excised using a conjunctival or corneoscleral scissors (). The size of the graft should be 1-2 mm larger than the size of the perforation. The conjunctiva may be reposited with fibrin glue, however this step is not essential. Use of autologous blood or simple pressure for a few minutes may also help repositing the conjunctiva back. Although the superior quadrants are preferred for harvesting the graft, in cases where this is not feasible such as in cicatrizing conjunctivitis, the donor tissue can be excised from the inferior quadrants.
Figure 3. This figure illustrates the different steps of a tenon's patch graft. a) Creation of a conjunctival bleb with balanced salt solution b) Harvesting the graft from the inferotemporal quadrant c) Plugging of the graft within the margins of the perforation with a blunt instrument d) Securing the graft with fibrin glue e-g) Placement of vertical and horizontal infinity sutures h) Gentle maneuvering with an iris repositor to release the iris adhesion. The step is being carried out under air in the anterior chamber i) A tectonically stable globe noted at the end of the procedure with a mobile air bubble in the anterior chamber.
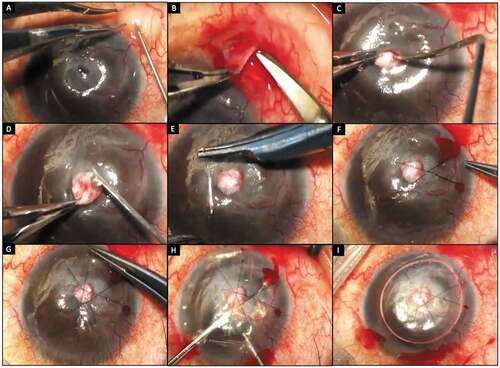
Securing the graft
Any debris over the area of perforation is cleared. Once the graft is excised, it is placed over the perforation and gently plugged into it, using the blunt end of a suture tying forceps or any other instrument (). If the graft is noted to be in excess, the surplus tissue can be cautiously excised. Once in place, the graft is secured with fibrin glue (TISSEEL kit from Baxter AG, Vienna, Austria) (). Overlay sutures are then placed using 10–0 monofilament nylon. These sutures can be placed in an infinity pattern or a box pattern (). While placing a box suture, the longer limbs of the suture must lie over the area of the perforation to ensure compression of the graft. If the limbs straddle the perforation, the sutures may compress the surrounding cornea and cause instability of the graft. Similarly, in an infinity suture, the areas of intersection of the suture must overlap the area of the perforation (). The tenon's can also be secured with interrupted 10–0 nylon sutures in case of large perforations.
Reformation of the anterior chamber
Once the graft is secured with fibrin glue and sutures, an entry into the anterior chamber is made using a microvitreoretinal blade or a 26/29-gauge needle. A small air bubble is injected initially to form the anterior chamber. This is followed by the injection of Ringer‘s lactate solution or balanced salt solution. Overhydration of the chamber must be avoided as this can dislodge the graft. As the tenon's layer is not a watertight barrier, some egress of fluid from the site of perforation is to be expected and the formation of a tight globe with repeated hydration must not be attempted. Any iris adherent to the area of perforation can be gently reposited using an iris repositor (). Once again, aggressive maneuvering during this step can destabilize the graft or extend the perforation and is strongly discouraged. Once the anterior chamber is formed, the side port is hydrated and a BCL is placed. A mobile air bubble filling less than half the anterior chamber can be left in situ (). It is not mandatory to aim to make the chamber air free or the wound watertight.
Modifications
Amniotic membrane graft
The addition of an AM layer provides additional tectonic support to the wound and also increases the stability of the graft.Citation27 The epithelium surrounding the perforation should be debrided prior to the placement of the AM. The AM is usually placed basement membrane side up and as a single layer in an overlay fashion. The membrane can be secured using fibrin glue or 10–0 monofilament nylon sutures. An additional AM can be placed over the entire cornea in case of large epithelial defects, in order to aid the healing process. The addition of the amniotic membrane also provides a watertight closure to the otherwise fluid permeable tenon's layer.
(b) Tissue adhesive
Cyanoacrylate glue can be used to secure the tenon's graft and to provide further support in case of larger perforations.Citation10,Citation11 The glue can selectively be placed at the margins of the tenon's to help adhere it to the underlying stroma. Alternatively, a thin coating can be placed over the entire perforation, over the layer of tenon's. Similar to combining an AM with TPG, when TA application is required, the host bed should be prepared prior by debriding 1–2 mm of the epithelium surrounding the perforation. Care has to be taken to avoid touching the instrument with the TA to the tenon's, to avoid complete graft displacement, as the graft may stick to the instrument itself. Concurrent use of TA with TPG may increase risk of vascularization postoperatively.
(c) Tuck-in Tenon's patch graft
Another technique to ensure that the graft is well secured, is to create a 360-degree stromal pocket within the margins of the perforation and to tuck the tenon's layer within this pocket.Citation10 Tissue adhesives can also be used in addition to this to procedure to provide an additional scaffold of support.
Postoperative care
Postoperatively the patients are started on a tapering course of topical steroids (prednisolone acetate 1%) over 4–6 weeks. Prophylactic antibiotics (moxifloxacin 0.5%) are given in the initial postoperative weeks or until the BCL is removed. The management of the underlying disease, either in the form of oral anti-virals or lubricating agents or oral immunosuppression must be continued as appropriate. The healing of the donor site must also be monitored until complete re-epithelialization occurs.
Mechainism of actoin and usual postoperative course
Mechanism of Action
The tenon's layer acts initially by plugging the area of perforation. The tissue provides a scaffold over which the surrounding epithelium migrates. Once the epithelial continuity is reestablished, the wound becomes watertight. The fibroblasts within the tenon's layer may contribute towards the corneal scarring seen following this procedure.Citation18 These fibroblasts are physiologically different from those present within the cornea.28 The corneal fibroblasts are sensitive to inflammation and produce an increased amount of pro-inflammatory cytokines in response to an inciting stimulus. In comparison, the fibroblasts within the tenon's capsule have a dampened response to inflammation and thus may help in a faster healing response.28
Usual Postoperative Course
The normal postoperative course is depicted in the representative collage in . As mentioned earlier, the tenon's layer allows egress of fluid through it. This accounts for the swelling of the graft noted in the early postoperative period (). If an additional AM layer is not placed, the wound itself will not be watertight. And so, noting a shallow anterior chamber in the initial 1 week is not uncommon and is not a cause for concern. Once epithelialization begins, the graft tissue will slowly start to undergo deturgescence (). This continues even after complete epithelialization has occurred. Since there are no large series on the postoperative follow-up of these cases, it is hard to determine how long these re-modelling changes continue. However as seen in this case and the report by Chaudhary et al, a stable anterior corneal surface is attained by the third month of the postoperative period ().Citation27 Sharma at al reported a mean duration of 13.3 ± 1.2 weeks for the formation of a stable scar.Citation10 However, changes within the stroma with further compaction of the graft tissue and corneal thinning, can continue to occur until the third postoperative year.Citation27
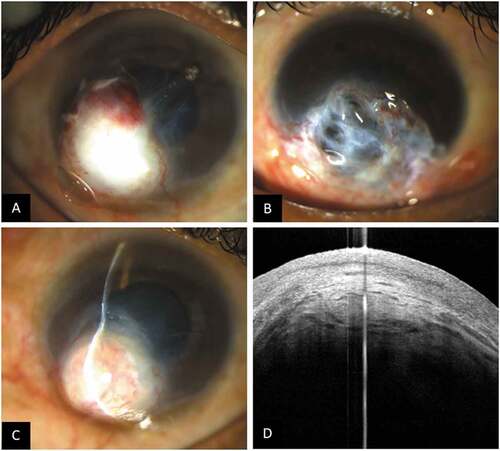
Figure 4. Representative collage of images depicting the postoperative course of healing following tenon's patch graft with the corresponding OCT images. a) Preoperative image showing a 1x2mm paracentral corneal perforation b) Postoperative day 1 image showing a well secured tenon's graft c) Day 12 image showing swelling of the graft tissue on the OCT image with early epithelialization d) Three months postoperative image showing a well epithelialized surface on OCT. The graft is compact and well-integrated within the stroma. e, f) Images from the 6 months and 1-year postoperative period showing a thinned out compact stroma with a stable ocular surface. (OCT-optical coherence tomography).
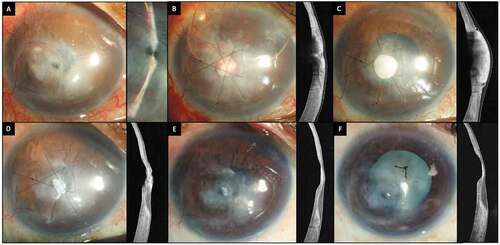
A representative image of a corneal button showing the histopathology of the corneal scar after TPG is presented in . A stable, stratified epithelial layer continuous with the normal epithelium is seen in the area of the TPG. The tenon's layer is incorporated within the stroma and is well delineated from the surrounding stromal collagen especially on the PAS stain section (). Beneath the tenon's layer an irregular deposition of collagen fibers with formation of a pseudocornea is noted (). The above findings highlight that the TPG provides a good long term tectonic support to the weakened cornea. The retention of the graft tissue along with the irregular collagen contribute to the corneal scarring seen postoperatively. If present in the visual axis this may hamper the visual acuity and has to be taken into consideration when planning the procedure in perforations in the central cornea. Lastly, despite the tissue swelling the initial postoperative period, there is significant thinning on long-term follow-up of these cases and so TPG, per se, may not be the procedure of choice if volume replacement is required. is a collage of images showing the postoperative course of eyes that have undergone a TPG.
Figure 5. Histopathological images of a section of a corneal button depicting the corneal scar following tenon's patch graft a) Hematoxylin and eosin stain; magnification 40x, b) Periodic acid–Schiff stain; magnification 40x. Stratified epithelial layer continuous with the normal epithelium is seen in the area of the tenon's graft (green arrow heads). Incorporated tenon's layer within the stroma (green arrows) with pseduocornea formation is noted beneath the tenon's layer (black arrow).
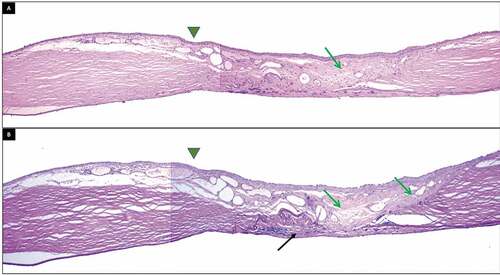
Figure 6. This collage of images depicts the healing pattern following tenon's patch graft. a) Swelling of the tenon's tissue is noted in the initial postoperative period which subsides, leaving behind a compact graft tissue with corneal thinning (b). c, d) Use of both fibrin glue and nylon sutures to secure the graft. e, f) Tenon's tissue is secured only with fibrin glue. The tissue is integrated to result in a vascularized corneal scar.
Clinical efficacy and complications
Clinical Efficacy
The parameters used to determine the efficacy of this procedure would be the re-establishment of a stable ocular surface with an organized and formed anterior chamber. Formation of an adherent leucoma would also be an acceptable outcome following TPG. In the study by Korah et al, 26/31 patients had an adherent leucoma formation.Citation11 However, in this series, no attempt was made to release the iris adhesions intraoperatively. Also, 6 of these eyes had a flat anterior chamber along with the adherent leucoma and were considered anatomical failures. One eye with Pseudomonas infection continued to have active infection after TPG and eventually underwent evisceration. And so, TPG should be reserved for those cases where the inflammation within the cornea is minimal, or a healing trend is noted.
A good anatomical outcome with a well-formed anterior chamber has been reported following TPG in other series as well (). Sharma et al. found epithelialization to occur within 26 days of the surgery while in the report by Chaudhary et al, the same process was complete within 2 weeks.Citation10,Citation27 Scarring is inevitable in these cases, and the corneal scar following TPG offers a good tensile strength despite the significant thinning as demonstrated in the report by Chaudhary et al. Further visual rehabilitation with rigid contact lens or optical keratoplasties can be performed with good visual outcomes. These grafts fare better than grafts following tissue adhesives as there is less vascularization following TPG, thus decreasing the risk of graft rejection and subsequent failure.
Table 3. This table encapsulates the salient findings of various studies on Tenon's patch graft.
Complications
There are no reported intraoperative complications or postoperative donor site complications following tenon's patch graft. Although shallowing of the anterior chamber may be noted in the initial one week of the postoperative period, this is to be expected especially when TPG is performed in isolation. If a shallow chamber is noted, it can be observed up to 7–10 days. If the shallowing persists reformation of the chamber can be attempted. In the series by Sharma et al, 4/28 patients had a flat anterior chamber with an active leak on Seidel test.Citation10 Three of these cases required keratoplasty while one eye healed with adherent leucoma formation.
Another rare complication of this procedure is graft retraction or displacement. Both Singhal et al and Sharma et al reported one case each in their respective series.Citation7,Citation10 These cases where managed with resuturing of the graft with 10–0 nylon sutures. Rarely, the graft can get completely dislodged requiring a repeat procedure of either TPG, AM grafting or a keratoplasty. In our experience, we have also observed complications such as intratenon’s hemorrhage, tenon’s melt and pseudoectasia with the use of Tenon’s patch graft. Intratenon’s hemorrhage occurs from the friable blood vessels which generally resolves on conservative treatment over a period of time. Melting of the Tenon’s graft has been observed in patients having dry eye disease. This can be managed by doing a patch graft with an AM graft, along with topical antibiotics and copious lubricants. Pseudoectasia generally occurs if the tenon’s tissue is thick and protuberant. This may be managed by guarded surface cauterization of tenon’s until the surface of tenon’s contour matches with the adjacent cornea ()
Summary
Tenon's patch graft is a simple and effective procedure that does not require the back up of an eye bank and can be performed in all cases of small to moderate-sized corneal perforations which do not have active suppuration. The surgery restores the tectonic support to the eye and re-establishes a stable ocular surface. Since the literature regarding this procedure is limited, it would be premature to comment on the efficacy of TPG versus other techniques used in the management of corneal perforations. By detailing the indications, surgical technique, and management of complications in this review the authors hope that TPG becomes more widely adopted and practiced. This in in turn will generate enough evidence on the follow-up and outcomes of the procedure and can help establish the comparative efficacy of the surgical technique.
TPG is cost-effective with a low rate of postoperative complications making it a viable option especially in areas with limited resources. The decreased risk of vascularization and lack of tissue-related rejection gives an added advantage to this procedure over other modalities in the management of corneal perforations. The resultant corneal scarring can be managed with optical keratoplasties or rigid contact lenses. With careful case selection and appropriate intraoperative technique, this procedure can be employed by all anterior segment surgeons in the management of corneal perforations with good outcomes.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Jhanji V, Young AL, Mehta JS, et al. Management of corneal perforation. Surv Ophthalmol. 2011;56(6):522–538.doi:10.1016/j.survophthal.2011.06.003.
- Hirst LW, Smiddy WE, Stark WJ. Corneal perforations: changing methods of treatment, 1960–1980. Ophthalmology. 1982;89(6):630–635. doi:10.1016/S0161-6420(82)34742-9.
- Rodríguez-Ares MT, Touriño R, López-Valladares MJ, et al. Multilayer amniotic membrane transplantation in the treatment of corneal perforations. Cornea. 2004;23(6):577–583.doi:10.1097/01.ico.0000121709.58571.12.
- Sun Y-C, Kam JP, Shen TT. Modified conjunctival flap as a primary procedure for nontraumatic acute corneal perforation. Tzu Chi Med J. 2018;30(1):24–28. doi:10.4103/tcmj.tcmj_191_17.
- Fernandes M, Vira D. Patch graft for corneal perforation following trivial trauma in bilateral terrien’s marginal degeneration. Middle East Afr J Ophthalmol. 2015;22(2):255–257. doi:10.4103/0974-9233.151873.
- Deshmukh R, Stevenson LJ, Vajpayee R. Management of corneal perforations: an update. Indian J Ophthalmol. 2020;68(1):7–14. doi:10.4103/ijo.IJO_1151_19.
- Singhal D, Sahay P, Maharana PK, et al. Clinical presentation and management of corneal fistula. Br J Ophthalmol. 2019;103(4):530–533.doi:10.1136/bjophthalmol-2018-312375.
- Morris DA, Ramocki JM, Shin DH, et al. Use of autologous Tenon’s capsule and scleral patch grafts for repair of excessively draining fistulas with leaking filtering blebs. J Glaucoma. 1998;7(6):417–419. doi:10.1097/00061198-199812000-00011.
- American Academy of Ophthalmology. Tenon patch graft for corneal perforation. https://www.aao.org/annual-meeting-video/tenon-patch-graft-corneal-perforation
- Sharma N, Singhal D, Maharana PK, et al. Tuck-in tenon patch graft in corneal perforation. Cornea. 2019;38(8):951–954.doi:10.1097/ICO.0000000000001955.
- Korah S, Selvin SST, Pradhan ZS, et al. Tenon's patch graft in the management of large corneal perforations. Cornea. 2016;35(5):696–699.doi:10.1097/ICO.0000000000000808.
- Mansour HA, Mansour AM. Autologous tenon plug and patch in phacoburn. BMJ Case Rep. 2021;14(1):e238970. doi:10.1136/bcr-2020-238970.
- Maharana PK, Singhal D, Sahay P, et al. Tenon patch graft for corneal fistula: a rare entity treated by a simple technique. BMJ Case Rep. 2017;2017: bcr-2017-222790 doi:10.1136/bcr-2017-222790.
- Cho RI, Elner VM. Closure of mid-posterior Tenon’s capsule in enucleation. Ophthalmic Plast Reconstr Surg. 2010;26(6):462–466. doi:10.1097/IOP.0b013e3181dac629.
- Kozdon K, Caridi B, Duru I, et al. A Tenon’s capsule/bulbar conjunctiva interface biomimetic to model fibrosis and local drug delivery. PLoS One. 2020;15(11):e0241569.doi:10.1371/journal.pone.0241569.
- Dutton JJ. Atlas of Clinical and Surgical Anatomy. Phila- delphia, PA: W.B: Saunders Company; 1994. 94–5.
- Jones LT. A new concept of the orbital fascia and rectus muscle sheaths and its surgical implications. Trans Am Acad Ophthalmol Otolaryngol. 1968;72:755–764.
- Roth A, Mühlendyck H, De Gottrau P. [The function of Tenon’s capsule revisited]. J Fr Ophtalmol. 2002;25:968–976.
- Doxanas MT, Anderson RL. Clinical Orbital Anatomy. Baltimore, MD: Williams & Wilkins; 1984. 108–115.
- Whitnall SE. Anatomy of the Human Orbit and Accessory Organs of Vision (Reprint). New York: Publishing Company Inc; 1979. 288–302.Krieger RE
- Kakizaki H, Takahashi Y, Nakano T, et al. Anatomy of Tenon's capsule. Clin Exp Ophthalmol. 2012;40(6):611–616.doi:10.1111/j.1442-9071.2011.02745.x.
- Gris O, Wolley-Dod C, Güell JL, et al. Histologic findings after amniotic membrane graft in the human cornea. Ophthalmology. 2002;109(3):508–512.doi:10.1016/s0161-6420(01)00969-1.
- Shanbhag SS, Patel CN, Goyal R, et al. Simple limbal epithelial transplantation (SLET): review of indications, surgical technique, mechanism, outcomes, limitations, and impact. Indian J Ophthalmol. 2019;67(8):1265–1277.doi:10.4103/ijo.IJO_117_19.
- Weinberg L, Peake B, Tan C, et al. Pharmacokinetics and pharmacodynamics of lignocaine: a review. World Journal of Anesthesiology. 2015;4(2):17–29. 10.5313/wja.v4.i2.17
- Roberts JE, MacLeod BA, Hollands RH. Improved peribulbar anaesthesia with alkalinization and hyaluronidase. Can J Anaesth. 1993;40(9):835–838. doi:10.1007/BF03009254.
- Islam MN, Chakroborty S, Bandopadhay R, et al., Sodium bicarbonate versus sodium hyaluronidase in ocular regional anaesthesia--a comparative study. J Indian Med Assoc. 2012; 110(1): 29–30. 39
- Chaudhary S, Basu S, Donthineni PR. Long term outcome of Tenon’s patch graft in corneal perforation secondary to neurotrophic keratitis: a case report on a 4-year anatomical functional outcome. Int J Surg Case Rep. 2021;83:106046. doi:10.1016/j.ijscr.2021.106046.