ABSTRACT
Purpose
This review aims to evaluate and simplify the recent literature on preoperative surgical planning, intraoperative considerations, postoperative surprises, and their management in patients with keratoconus undergoing cataract surgery.
Methods
A review of the literature was done to analyze all the pertinent articles on Keratoconus and cataract surgery.
Results
The surgical planning of cataracts in eyes with keratoconus needs a multifaceted approach. Preoperatively, techniques such as cross-linking or the use of intra-corneal rings help stabilize the progression. Unreliable biometric measurements are a significant problem in keratoconus patients, especially in an advanced stage of the disease. It is better to consider actual K readings if the K value is less than 55D but for a K value, more than 55D using standard K values will prevent postoperative refractive surprises. For calculation of K values, an elevation-based device like pentacam gives better repeatability in mild to moderate cases whereas for advanced keratoconus none of the keratometers is reliable. Recently, the Kane keratoconus formula performed better in all stages of disease whereas previous studies showed good results with SRK/T formula is a mild and moderate disease. Monofocal intraocular lenses are a better choice in these patients. Toric lenses can be used in mild and stable keratoconus. Intraoperatively, the use of a customized RGP lens can overcome the challenge of image distortion and loss of visual perspective. Despite taking necessary measures, postoperative refractive surprise can occur and can be managed with IOL exchange or Secondary IOLs.
Conclusion
There is a spectrum of challenges in managing cataracts in keratoconus which makes thorough preoperative planning important for good surgical outcomes. Despite the measures, there might be post-operative surprises and the patients need to be informed regarding the same.
INTRODUCTION
Keratoconus (KC) is a bilateral ectasia of the cornea due to noninflammatory thinning.Citation1 This corneal thinning causes mild to severe visual impairment by inducing myopia or astigmatism (Regular or irregular).Citation2 About 1 in every 2000 people are estimated to develop keratoconus,Citation2 with its onset in early adolescence, and the possibility of progression up to about 30 or 40 years of age, after which it generally stabilizes.Citation3 It is commonly associated with allergic eye disease. Keratoconus patients tend to have a cataract in the younger age group and the most common type of cataract seen in these patients is nuclear sclerosis(83%)Citation4 The surgical planning of cataracts in eyes with keratoconus brings into perspective several unique considerations such as determination of progression of the disease, preoperative planning, biometry, choice of the intraocular lens (IOL), intra-operative surgical challenges due to poor visibility, image distortion and tackling the postoperative refractive surprises and visual outcomes. In this context, we aim to review the recent practice patterns and literature to help plan cataract surgery in keratoconus more effectively.
METHODOLOGY
For this review, a comprehensive search of databases was done on PubMed and Google Scholar. The keywords used were: keratoconus, astigmatism, toric lens, multifocal lens, intraocular lens, IOL calculation formula, keratometry, cataract surgery, phacoemulsification, and rigid gas permeable lenses. No restriction was applied on the age, gender, language, or type of journal. Inclusion criteria for the study selection were patients with keratoconus, who have undergone or undergoing cataract surgery and an artificial lens is implanted in their eyes. The formulas and the measurement device used for calculating the IOL power are mentioned along with intraoperative challenges and postoperative problems. Exclusion criteria were studies that lacked information related to IOL power calculation. A higher priority was given to newer publications from 2015 until October 2021. A few studies published before 2015 were also reviewed based on the inclusion criteria. Initially, 320 articles were selected and their abstracts were assessed by one of the authors and later reviewed by the other author. After this initial assessment 130 articles were included, out of which 73 had maximum relevance concerning the purpose of this review.
PREOPERATIVE CHALLENGES
Keratometry
The IOL power calculation is challenging in patients with keratoconus for multiple reasons. The simulated keratometry (SimK) value is taken which is derived by taking the radius of anterior corneal curvature and a standard keratometry index of 1.3375. The SimK assumes a fixed ratio between the anterior and posterior corneal curvature. In Keratoconus patients, however, this ratio is altered.Citation5–7
Kamiya et al calculated total corneal refractive power (TCRP) using the Ray tracing method which considers both anterior and posterior corneal surface and compared it with SimK value. The degree of variation between the Sim K and TCRP values in keratoconus eyes was markedly high compared to normal eyes, and this difference became even more evident as the disease progressed. The authors suggested that the likely cause of hyperopic refractive error post-cataract surgery in KC patients is due to the overestimation of TCRP.Citation8 Also a decentered cone not coinciding with the visual axis will have an impact on the keratometry readings.Citation9
Effective Lens Position
The predicted effective lens position by vergence formula depends on Axial length and Anterior chamber depth. Both these parameters are higher in KC patients in comparison with normal eyes and hence will affect the effective lens position.Citation10 Axial length is a very strong predictor of the final refractive outcome when compared to other variables like anterior chamber depth, keratometric value etc.Citation11 Obtaining a repeatable and accurate K value, is difficult in these patients because of irregular tear film reflex.Citation12
Intraocular Power Calculations
The routine methods use manual and automated keratometry using Placido disk-based corneal topography devices. They assess only the anterior surface of the cornea whereas an elevation-based Scheimpflug imaging device like PentacamTM(Oculus) will calculate the total corneal refractive power by assessing the anterior as well as the posterior corneal curvatures.Citation13,Citation14 The importance of using an elevation based topography device was seen by Kamiya et al. when they documented that the K values measured with IOL master 500 had a higher chance of residual hyperopia, especially in cases of advanced Keratoconus whereas when K values from Pentacam were used the postoperative refractive error showed a myopic trend.Citation15 summarises the recent studies on various Intraocular lens formulas in Keratoconus.
Table 1. Review of recent studies on various Intraocular lens formulas in Keratoconus.
Hashemi et al. showed that the repeatability with a Pentacam device to measure K value was best if the value was 55D or less. Javal Keratometer was next best to Pentacam in documenting repeatability of K values however, this was not seen when maximum K value was more than 55 D. The devices which were used in this study were Placido topographer (Eyesys), Scheimpflug pachymeter (Pentacam), partial coherence interferometry device (IOLMaster), Scanning-slit corneal topographer (Orbscan), and Javal manual keratometer.Citation16 Similar results were seen in patients with posterior keratoconus as well.Citation17
Watson et al (2013) retrospectively reviewed 92 eyes in 64 patients of keratoconus, in whom a non-aspheric intraocular lens was implanted during cataract surgery. They concluded that for eyes with a mean K of ≤55 D, a suitable option is taking actual K value and keeping a target of low myopia of −1.0D or −1.50D depending on the stage of Keratoconus, but if the K value is >55D, the actual K values can result in a large hyperopic shift despite taking a post-op target of −5.4D, therefore, it is better to use standard K values (43.25D) in such cases with a mean target of low myopia(−1.8D).Citation18
The largest case series of cataract surgery in keratoconus eyes was published by Kane et al in 2020. The purpose was to evaluate the precision of IOL formulas which are used routinely in normal eyes, (Haigis, Barrett Universal 2, Holladay 1 and 2, Hoffer Q, SRK/T, and Kane) compared to IOL formulas which are made exclusively for Keratoconus patients (Kane Keratoconus formula and Holladay 2 with Keratoconus Adjustment). A total of 147 eyes of 147 keratoconus patients who had preoperative biometry were included in the study. The Prediction error was calculated by comparing the true refractive outcome with the predicted refraction which was derived by the above formulas. The authors concluded that the Kane Keratoconus formula performed best in all stages of KC followed by SRK/T. The authors emphasized that in stage 3 Keratoconus Kane keratoconus formula did very well when compared to other formulas with the least prediction error. To avoid hyperopic refractive results Kane et al suggested that in stage 1 Keratoconus patients there should be no adjustment to target refraction, for stage 2 a myopic target of −0.75 to −1.5 should be aimed for, and for stage 3 a myopic target of −2.0 to −3.0 should be aimed. This is the only study that has compared normal IOL formulas with IOL formulas specially designed for keratoconus patients.Citation19
Few other studies on Keratoconus patients in whom normal IOL formulas like SRK II, SRK/T, Holladay 1 and 2, Haigis, Hoffer Q and Barretts universal II were used, SRK/T formula showed remarkably better prediction error when compared to other formulasCitation11,Citation15,Citation20
Whereas another study by Wang et al showed that Barretts Universal II formula has the lowest error in Stages 1 and 2 of Keratoconus. The IOL formulas taken in this study were Holladay 1 and 2, Hoffer Q, Haigis, Barrett Universal II, and SRK/T formulas. For stage III eyes Barrett’s Universal II formula could not be used as the online calculator of this formula accepts a limited span of input variables and for these patients, Haigis formula performed best when compared to others, though all six formulas evaluated in the study resulted in hyperopic predicted errors.Citation14
Intraocular Lens Choice
The choice of IOL to be implanted, monofocal or toric is an important consideration in planning cataract surgery in KC. Assessment of progression of the disease is very important before considering a Toric IOL. Risk factors like young age, eye rubbing, changes in refractive error, and baseline steep keratometric values should be documented in these patients.Citation21
Stable and mild-to-moderate keratoconus patients in whom toric IOL was implanted during cataract surgery had shown to have significant improvement in postoperative uncorrected and best-corrected visual acuityCitation16Citation22–25 without significant induction of corneal high-order aberrations.Citation23 Therefore, it was advised to consider Toric IOL in mild keratoconus patients if they are RGP intolerant.Citation23 The option of Toric diffractive lens in mild stable keratoconus patients is studied by Farideh et al. Patients were evaluated at 1,3 and 6 months and the authors concluded that the toric diffractive lens provided appropriate distance, near and intermediate vision. The contrast sensitivity and aberration values both preoperatively and postoperatively were comparable whereas the defocus curve obtained postoperatively was good mainly due to the specific design of IOL.Citation26
Patients with irregular astigmatism that improves with refraction and have topographic and refractive stability for a minimum of 1 year before planning surgery can be considered for Toric IOL implantation.Citation22,Citation27
Rotation of Toric IOL greatly depends on capsular bag size, axial length, and associated myopia.Citation28 Theoretically the patients with keratoconus should be prone to IOL rotation due to high axial length and high myopia but the studies of toric IOL in KC have not reported this complication. Residual astigmatism can be produced due to rotation of the toric IOL post-surgery.Citation28 Many studies have shown that the hydrophobic acrylic Toric IOLs have good rotational stability and give a good result.Citation29–31 Another option is using a capsular tension ring as it has been shown to prevent early post-op rotation in patients with high myopia.Citation32
Toric IOL should not be considered in patients with progressive disease, difficult refraction, or in whom there is a high difference between preoperative RGP lens corrected visual acuity and spectacle-corrected visual acuity.Citation27,Citation33
CORNEAL STABILIZING PROCEDURE
Intrastromal Corneal Ring Segment (ICRS)
The studies discussed above have shown that correct power and type of IOL will help in getting a good visual outcome in patients with mild or moderate KC but the corneal abnormality leading to the component of irregularity persists and hence will cause a decrease in visual acuity. It is seen in many studies that if ICRS is implanted in patients with keratoconus the abnormalities in the cornea are significantly reduced causing an improvement in the visual acuity of the patients.Citation34–49
Alfonso et al. reported a case series of 47 keratoconus patients (70 eyes) with cataracts in whom monofocal IOL was implanted post-ICRS in a gap of 6 months. The patients were followed up for a 5-year duration. Authors compared the corrected distance visual acuity (CDVA) in their study with the earlier studies, in which cataract surgery alone was performed with either monofocal or toric IOL implantationCitation11,Citation16,Citation24,Citation25 and found that the CDVA in their study was better with no significant refractive surprise. The likely reason can be that ICRS implantation will improve the shape of the cornea, regularizing the surface and therefore a more precise central corneal power and effective lens position could be attained.Citation39
All the earlier studies were done using either monofocal or toric IOL but Lisa et al. studied 17 eyes of 11 patients in whom extended range of vision IOL was implanted after, the implantation of Ferrara-type intrastromal corneal ring segments. According to the authors, there were two reasons for using extended depth of focus IOLs, firstly it improves the visual acuity from intermediate to far distances, and secondly, it increases tolerance for defocus which is helpful in keratoconus patients as the residual refractive surprise is a common postoperative complication in these patients. The results seen in this study were very encouraging with a significant improvement in Uncorrected distant visual acuity.Citation44
Collagen Cross-Linking
Stability in refraction after collagen cross-linking is achieved at around 6 months and there is not much change in refraction up to 12 months.Citation50 Spadea et al. evaluated two patients with age more than 50 years with high myopia, KC progression, and cataracts. A gap of 6 months was taken between CXL and IOL implantation. The authors opted for a target small myopic shift when choosing the IOL power for patients with staphyloma, as the measurement of accurate axial length was difficult and a reduction of myopia was possible because of the corneal flattening induced by CXL. The authors concluded that a 2-stage procedure of corneal CXL with cataract surgery and IOL implantation is safe and effective and it gives time to achieve good vision.Citation51
INTRAOPERATIVE CHALLENGES
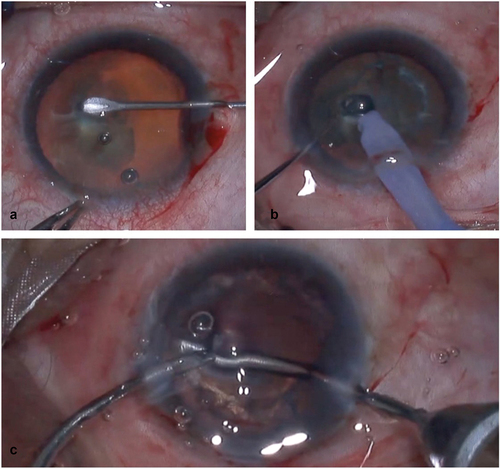
Usual methods which are used to avoid corneal dryness are Balanced salt solution (BSS) irrigation or application of viscoelastic agents on the corneal surface.Citation52 However, in highly irregular corneas BSS may be ineffective in improving surgeon’s visualization needing continuous application by an assistant and viscoelastic agents may easily slip off the corneal surface.Citation53 In severe stage disease, ectatic corneas lead to image distortion and the lack of visual perspective during intra-operative steps which can be challenging during capsulorhexis, nucleus management, irrigation, and aspiration as seen in .
Figure 1. Intraoperative distortion in viewing the instruments in the anterior chamber seen through the steep cone in Keratoconus during Phacoemulsification. Figure 1(a, b): Distorted broad appearance of cystitome during capsulorhexis and phacoemulsification instrument probe respectively. Figure 1c: Falsely curved appearance of irrigation and aspiration cannulas.
Oie et al for the first time used a rigid gas permeable contact lens (Hoya Hard Ex, Hoya Corp.) of 7.8 mm base curve and 8.8 mm diameter with 0 diopter power, placed over the cornea to perform phacoemulsification cataract surgery in 2 patients with severe keratoconus. Viscoelastic was placed over the cornea and the lens was placed stably over it despite corneal irregularity. The group concluded by saying that this technique facilitated in gaining depth perception and information along the Z-axis. The authors also pointed out that a larger visual field can be obtained by a large diameter lens, hence for future studies, a lens of size 11 diameter or more can be used.Citation54 Chanbour et al. did a study on six patients intending to use a modified customized RGP contact lens to improve visualization during all stages of phacoemulsification in irregular corneas and to avoid the open sky technique for cataract removal during penetrating keratoplasty. In these cases without RGP fitting, the surgery was extremely challenging. The flat Keratometric reading was used to decide on the base curve of the lens, this helped the formation of a thin layer of the tear film and hence prevented bubbles from being trapped under the lens. A −6.00D or −9.00 D power lens was used depending on corneal steepness and a 12 mm diameter lens could attain total corneal coverage. Two manual notches of approximately 2 mm in depth were fashioned at 2 and 10 o’clock for insertion of corneal incisions. First, viscoelastic was placed over the cornea above it RGP lens was placed, which maintained good stability of the lens during surgery. The authors concluded that the distortions were less, depth was well appreciated, the manipulation of the instruments was reported to be easier through all the stages and the operations were non-complicated in all six cases.Citation53
Another important point to consider is wound creation. According to Bourges J et al., Young’s modulus deteriorates in Keratoconus patients so they are advised to suture the incisions. This will also help in regularizing astigmatism and hence improving refraction. Although in most cases, the cornea is stable at the time of planning the cataract surgery but the surgical procedure might increase the probability of progression of keratoconus.Citation55 In multiple studies where cataract surgery is done in keratoconus patients it was been seen that clear corneal incisions are safe and do not need suturing.Citation11,Citation16,Citation23,Citation26,Citation39
POSTOPERATIVE
Residual Refractive Error
Very few studies or reports have highlighted management options for residual refractive error in keratoconus patients but many studies have shown that residual refractive error is common in keratoconus patients especially in advanced disease primarily due to erroneous IOL power calculation due to various challenges in these patients including high irregular astigmatism.Citation15,Citation16,Citation19,Citation20 Different options which can be tried in these patients are:
1) Spectacle correction and contact lenses
Spectacle correction can provide acceptable vision in patients with mild residual error.Citation56,Citation57 Contact lens covers the anterior corneal abnormalities and hence should be opted in patients with irregular astigmatism in whom spectacles are not of much benefits. Since most of the keratoconus patients are already using rigid contact lenses they are very comfortable going back to that. The type of contact lens will depend on the refractive error of the patient.Citation58 Soft lenses can be used in patients with low refractive error, regular astigmatism, or mild irregular astigmatism. Soft toric or custom toric can also be tried in these patients. RGP lenses or different exclusive lenses like scleral, piggyback or hybrid lenses can be tried in patients with a higher value of error.Citation58,Citation59,Citation60
2) Surgical options:
i) IOL based approaches
a) IOL exchange: This can be opted as one of the options but it is a challenging procedure and has more chances of complications like posterior capsular dehiscence, zonular dialysis etc. Citation61,Citation62 It is advised to perform the lens exchange in first 4-6 weeks as fibrosis around the IOL will generally start beyond this period.Citation63
b) Secondary IOL: Secondary IOL can be either an anterior chamber Iris claw lens or a Piggyback lens in the sulcus. Anterior chamber iris-claw lens provides a sufficient amount of spherical correction but the astigmatic correction is only possible in the lower range. Few studies have shown that phakic anterior chamber Iris claw lens is an effective, safe, and predictable method in patients with KC and can significantly improve the visual function therefore these lenses can be explored as an option for patients with refractive surprise.Citation64,Citation65,Citation66,Citation67,Citation68 The piggyback technique involves the placement of a second intraocular lens in the sulcus to correct the residual error. There exists extensive literature to suggest that the implantation of Implantable Collamer lens (ICLs) into KC eyes is a safe and effective procedure Citation42,Citation69,Citation70,Citation71 more so than for AC phakic IOLs but Kurian et al have found in their work that the associated aberrations due to secondary IOL have an impact on the visual quality.Citation72 Some individual case reports have shown piggyback IOL being used for residual error after cataract surgery and the outcomes reported are favorable. Nevertheless, it still needs further studies to understand long term behaviour and visual outcomes.
Corneal Ectasia Post-Cataract Surgery
According to the authors’ knowledge till now only one case report is published in the literature which shows corneal ectasia following cataract surgery. Labiris et al reported a 38 yr old male patient who had keratoconus in both his eyes and has undergone both eyes collagen cross-linking 5 years back. The cataract surgery in the right eye was uneventful but after 3 months he reported an increase in myopic astigmatism. Scheimplflug imaging was suggestive of post-op ectasia, significantly reducing corneal hysteresis. The other eye was stable and did not show any signs of post-op ectasia. The likely explanation authors suggested was that the incision in phacoemulsification will result in mechanical stress in the cornea, mainly at the time of implantation of IOL and also increases ocular surface disease by destabilizing the tear film. Although the topography and corneal hysteresis in this patient improved after 6 months, the ectasia persisted.Citation61
SUMMARY AND CONCLUSION
The surgical planning of cataracts in eyes with keratoconus brings into perspective several unique considerations such as determination of stability of the keratoconus, pre-operative planning, biometry, choice of the intraocular lens (IOL), intra-operative surgical challenges, and tackling the postoperative refractive surprises. For stabilizing the progression of the disease, techniques like collagen cross-linking or the use of Intracorneal ring segment have been discussed in the literature. The preoperative challenge faced by many surgeons in keratoconus is unreliable biometry. While calculating the IOL formula a fixed ratio between the anterior and posterior corneal curvature is assumed and based on this simulated K value is obtained from the anterior corneal curvature and standard keratometric index. Since the Anterior and posterior curvature is altered in keratoconus there will be an overestimation of total corneal refractive power and hence a post-operative hyperopic refractive error is likely.
For this reason, it is recommended to use an elevation-based device like pentacam which performs well in these patients especially in mild to moderate forms as it takes into account both anterior and posterior curvature though in severe forms none of the keratometers gives a reliable result.Citation13–17 For IOL power calculation it is recommended to use standard K (43.25D) in patients with K values more than 55 whereas in patients with K values equal to or less than 55 taking real K value and keeping a target of low myopia depending on the stage of keratoconus is advised.Citation18 According to recent literature, the Kane keratoconus formula performs well in all the stages of keratoconus whereas SRK/T did well in mild-to-moderate forms of keratoconus.Citation11,Citation15,Citation19,Citation20
When selecting the type of Intraocular lenses it is better to opt for monofocal lenses through toric can be tried in patients with mild and stable keratoconus. Toric lenses should be avoided in patients who are willing to use contact lenses post-surgery or those who might go for keratoplasty in the future.Citation21–25
Intraoperative use of customized RGP lenses is discussed in a few studies to decrease the complication of image distortion and loss of visual perception during surgery.Citation53,Citation54 Since only a few studies have talked about these lenses this needs further studies to analyze their wide usage.
About wound creation, few earlier studies have advised performing sutured incision rather than self-sealing but many recent studies have shown that clear corneal incisions are safe for cataract surgery in Keratoconus patients.Citation11,Citation16,Citation23,Citation26,Citation39
Despite taking all the above measures, a few cases might end up in refractive surprise post-surgery. For such cases, an option of spectacles or contact lenses can be given in lower ranges but if there is a significant amount of refractive surprise then IOL exchange or secondary IOL can be tried in these patients for better visual outcomes.Citation62–73 There is no consensus about which IOL formula to use, which biometric device to opt for, or which K value to use especially in advanced keratoconus. In these cases, most of the studies have shown unreliable outcomes. This set of patients needs more research and should be focused on in future studies. Until then we should always counsel the patients that there is a certain amount of uncertainty in results despite all the preoperative planning and if any such thing happens postoperatively further intervention might be needed.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297–319. doi:10.1016/S0039-6257(97)00119-7.
- Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28(4):293–322. doi:10.1016/0039-6257(84)90094-8.
- Romero-Jiménez M, Santodomingo-Rubido J, Wolffsohn JS. Keratoconus: a review. Contact Lens Anterior Eye. 2010;33(4):157–166. doi:10.1016/j.clae.2010.04.006.
- Thebpatiphat N, Hammersmith KM, Rapuano CJ, Ayres BD, Cohen EJ. Cataract surgery in keratoconus. Eye Contact Lens. 2007;33(5):244–246. doi:10.1097/ICL.0b013e318030c96d.
- Tomidokoro A, Oshika T, Amano S, Higaki S, Maeda N, Miyata K. Changes in anterior and posterior corneal curvatures in keratoconus. Ophthalmology. 2000;107(7):1328–1332. doi:10.1016/S0161-6420(00)00159-7.
- Piñero DP, Camps VJ, Caravaca-Arens E, Pérez-Cambrodí RJ, Artola A. Estimation of the central corneal power in keratoconus: theoretical and clinical assessment of the error of the keratometric approach. Cornea. 2014;33(3):274–279. doi:10.1097/ICO.0000000000000048.
- Camps VJ, Piñero DP, Caravaca E, De Fez D. Preliminary validation of an optimized algorithm for intraocular lens power calculation in keratoconus. Indian J Ophthalmol. 2017;65(8):690. doi:10.4103/ijo.IJO_274_16.
- Kamiya K, Kono Y, Takahashi M, Shoji N. Comparison of simulated keratometry and total refractive power for keratoconus according to the stage of Amsler-Krumeich classification. Sci Rep. 2018;8(1):1–5. doi:10.1038/s41598-018-31008-1.
- Tan B, Baker K, Chen Y-L, et al. How keratoconus influences optical performance of the eye. J Vis. 2008;8(2):13. doi:10.1167/8.2.13.
- Kovács I, Miháltz K, Németh J, Nagy ZZ. Anterior chamber characteristics of keratoconus assessed by rotating Scheimpflug imaging. J Cataract Ref Sur. 2010;36(7):1101–1106.doi:10.1016/j.jcrs.2009.12.046.
- Alió JL, Peña-García P, Guliyeva FA, Soria FA, Zein G, Abu-Mustafa SK. MICS with toric intraocular lenses in keratoconus: outcomes and predictability analysis of postoperative refraction. British J Ophthalmol. 2014;98(3):365–370. doi:10.1136/bjophthalmol-2013-303765.
- McMahon TT, Anderson RJ, Roberts C, et al. Repeatability of corneal topography measurement in keratoconus with the TMS-1. Optometry Vision Sci. 2005;82(5):405–415. doi:10.1097/01.OPX.0000162667.22303.76.
- Kim SW, Kim EK, Cho B-J, Kim SW, Song KY, Tae-im Kim M. Use of the pentacam true net corneal power for intraocular lens calculation in eyes after refractive corneal surgery. J ref sur. 2009;25(3):285.
- Wang KM, Jun AS, Ladas JG, Siddiqui AA, Woreta F, Srikumaran D. Accuracy of intraocular lens formulas in eyes with keratoconus. Am J Ophthalmol. 2020;212:26–33. doi:10.1016/j.ajo.2019.11.019.
- Kamiya K, Iijima K, Nobuyuki S, et al. Predictability of intraocular lens power calculation for cataract with keratoconus: a multicenter study. Sci Rep. 2018;8(1):1–7. doi:10.1038/s41598-018-20040-w.
- Hashemi H, Heidarian S, Seyedian MA, Yekta A, Khabazkhoob M. Evaluation of the results of using toric IOL in the cataract surgery of keratoconus patients. Eye Contact Lens. 2015;41(6):354–358. doi:10.1097/ICL.0000000000000136.
- Tamaoki A, Kojima T, Hasegawa A, Nakamura H, Tanaka K, Ichikawa K. Intraocular lens power calculation in cases with posterior keratoconus. J Cataract Ref Sur. 2015;41(10):2190–2195.doi:10.1016/j.jcrs.2015.11.001.
- Watson MP, Anand S, Bhogal M, et al. Cataract surgery outcome in eyes with keratoconus. British J Ophthalmol. 2014;98(3):361–364. doi:10.1136/bjophthalmol-2013-303829.
- Kane JX, Connell B, Yip H, et al. Accuracy of intraocular lens power formulas modified for patients with keratoconus. Ophthalmology. 2020;127(8):1037–1042. doi:10.1016/j.ophtha.2020.02.008.
- Savini G, Abbate R, Hoffer KJ, et al. Intraocular lens power calculation in eyes with keratoconus. J Cataract Ref Sur. 2019;45(5):576–581. doi:10.1016/j.jcrs.2018.11.029.
- Gordon MO, Steger-May K, Szczotka-Flynn L, et al. Baseline factors predictive of incident penetrating keratoplasty in keratoconus. Am J Ophthalmol. 2006;142(6):923–30. e1. doi:10.1016/j.ajo.2006.07.026.
- Visser N, Gast ST, Bauer NJ, Nuijts RM. Cataract surgery with toric intraocular lens implantation in keratoconus: a case report. Cornea. 2011;30(6):720–723. doi:10.1097/ICO.0b013e31820009d4.
- Kamiya K, Shimizu K, Miyake T. Changes in astigmatism and corneal higher-order aberrations after phacoemulsification with toric intraocular lens implantation for mild keratoconus with cataract. Jpn J Ophthalmol. 2016;60(4):302–308. doi:10.1007/s10384-016-0449-x.
- Jaimes M, Xacur-García F, Alvarez-Melloni D, Graue-Hernández EO, Ramirez-Luquín T, Navas A. Refractive lens exchange with toric intraocular lenses in keratoconus. J Ref Sur. 2011;27(9):658–664.doi:10.3928/1081597X-20110531-01.
- Nanavaty MA, Lake DB, Daya SM. Outcomes of pseudophakic toric intraocular lens implantation in keratoconic eyes with cataract. J Refract Surg. 2012;28(12):884–890.doi:10.3928/1081597X-20121106-02.
- Farideh D, Azad S, Feizollah N, et al. Clinical outcomes of new toric trifocal diffractive intraocular lens in patients with cataract and stable keratoconus: six months follow-up. Medicine (Baltimore). 2017;96(12):e6340. doi:10.1097/MD.0000000000006340.
- Navas A, Suárez R. One-year follow-up of toric intraocular lens implantation in forme fruste keratoconus. J Cataract Refract Surg. 2009;35(11):2024–2027.doi:10.1016/j.jcrs.2009.05.043.
- Zhu X, He W, Zhang K, Lu Y. Factors influencing 1-year rotational stability of AcrySof Toric intraocular lenses. British J Ophthalmol. 2016;100(2):263–268. doi:10.1136/bjophthalmol-2015-306656.
- Anja Viestenz MD, F NSM, Behrens-Baumann W, Viestenz MD F A. Toric intraocular lenses-theory, matrix calculations, and clinical practice. J Refract Surg. 2009;25(7):611.
- Holland E, Lane S, Horn JD, Ernest P, Arleo R, Miller KM. The AcrySof Toric intraocular lens in subjects with cataracts and corneal astigmatism: a randomized, subject-masked, parallel-group, 1-year study. Ophthalmology. 2010;117(11):2104–2111. doi:10.1016/j.ophtha.2010.07.033.
- Zarranz-Ventura J, Moreno-Montañés J, Caire J, de Nova Fernández-Yáñez E, Sadaba-Echarri LM. Acrysof® toric intraocular lens implantation in cataract surgery. Archivos de la Sociedad Española de Oftalmología (English Edition). 2010;85(8):274–277.doi:10.1016/S2173-5794(10)70046-3.
- Safran SG. Use of a capsular tension ring to prevent early postoperative rotation of a toric intraocular lens in high axial myopia. JCRS Online Case Rep. 2015;3(2):41–43. doi:10.1016/j.jcro.2015.02.001.
- Visser N, Nuijts RM, de Vries NE, Bauer NJ. Visual outcomes and patient satisfaction after cataract surgery with toric multifocal intraocular lens implantation. J Cataract Refract Surg. 2011;37(11):2034–2042.doi:10.1016/j.jcrs.2011.05.041.
- Coskunseven E, Kymionis GD, Tsiklis NS, et al. One-year results of intrastromal corneal ring segment implantation (KeraRing) using femtosecond laser in patients with keratoconus. Am J Ophthalmol. 2008;145(5):775–9. e1. doi:10.1016/j.ajo.2007.12.022.
- Torquetti L, Berbel RF, Ferrara P. Long-term follow-up of intrastromal corneal ring segments in keratoconus. J Cataract Refract Surg. 2009;35(10):1768–1773.doi:10.1016/j.jcrs.2009.05.036.
- Kubaloglu A, Cinar Y, Sari ES, Koytak A, Ozdemir B, Ozertürk Y. Comparison of 2 intrastromal corneal ring segment models in the management of keratoconus. J Cataract Refract Surg. 2010;36(6):978–985.doi:10.1016/j.jcrs.2009.12.031.
- Piñero DP, Alio JL. Intracorneal ring segments in ectatic corneal disease–a review. Clin Exp Ophthalmol. 2010;38(2):154–167. doi:10.1111/j.1442-9071.2010.02197.x.
- Alfonso JF, Fernández-Vega Cueto L, Baamonde B, Merayo-Lloves J, Madrid-Costa D, Montés-Micó R. Inferior intrastromal corneal ring segments in paracentral keratoconus with no coincident topographic and coma axis. J Refract Surg. 2013;29(4):266–272.doi:10.3928/1081597X-20130318-06.
- Alfonso JF, Lisa C, Cueto LF-V, Poo-López A, Madrid-Costa D, Fernández-Vega L. Sequential intrastromal corneal ring segment and monofocal intraocular lens implantation for keratoconus and cataract: long-term follow-up. J Cataract Refract Surg. 2017;43(2):246–254.doi:10.1016/j.jcrs.2016.11.044.
- Alfonso JF, Lisa C, Fernández-Vega L, Madrid-Costa D, Montés-Micó R. Intrastromal corneal ring segment implantation in 219 keratoconic eyes at different stages. Graefes Arch Clin Exp Ophthalmol. 2011;249(11):1705–1712. doi:10.1007/s00417-011-1759-9.
- Alfonso JF, Lisa C, Fernández-Vega L, Madrid-Costa D, Poo-López A, Montés-Micó R. Intrastromal corneal ring segments and posterior chamber phakic intraocular lens implantation for keratoconus correction. J Cataract Refract Surg. 2011;37(4):706–713.doi:10.1016/j.jcrs.2010.10.060.
- Fernández-Vega Cueto L, Lisa C, Poo-López A, Madrid-Costa D, Merayo-Lloves J, Alfonso JF. Intrastromal corneal ring segment implantation in 409 paracentral keratoconic eyes. Cornea. 2016;35(11):1421–1426. doi:10.1097/ICO.0000000000000978.
- Sánchez JFA, Cueto LF-V, Costa DM, Micó RM. Intrastromal corneal ring segment and intraocular lens implantation in patients with keratoconus and cataract. J Emmetropia Cataract Refract Corneal Surg. 2012;3(4):193–200.
- Lisa C, Zaldivar R, Fernández-Vega Cueto A, Sanchez-Avila R, Madrid-Costa D, Alfonso J. Clinical outcomes of sequential intrastromal corneal ring segments and an extended range of vision intraocular lens implantation in patients with keratoconus and cataract. J Ophthalmol. 2018;2018:1–7. doi:10.1155/2018/8328134.
- Fahd DC, Jabbur NS, Awwad ST. Intrastromal corneal ring segment SK for moderate to severe keratoconus: a case series. J refract surg. 2012;28(10):701–705.doi:10.3928/1081597X-20120921-05.
- Fahd DC, Alameddine RM, Nasser M, Awwad ST. Refractive and topographic effects of single-segment intrastromal corneal ring segments in eyes with moderate to severe keratoconus and inferior cones. J Cataract Refract Surg. 2015;41(7):1434–1440.doi:10.1016/j.jcrs.2014.10.037.
- Carballo J, Puell MC, Cuiña R, Vázquez JM, Benitez-del-Castillo JM. Changes in visual function under mesopic and photopic conditions after intrastromal corneal ring segment implantation for different stages of keratoconus. J Cataract Refract Surg. 2013;39(3):393–402.doi:10.1016/j.jcrs.2012.09.025.
- Torquetti L, Ferrara G, Almeida F, et al. Intrastromal corneal ring segments implantation in patients with keratoconus: 10-year follow-up. J Refract Surg. 2014;30(1):22–26. doi:10.3928/1081597X-20131217-02.
- Ziaei M, Barsam A, Shamie N, et al. Reshaping procedures for the surgical management of corneal ectasia. J Cataract Refract Surg. 2015;41(4):842–872. doi:10.1016/j.jcrs.2015.03.010.
- Asri D, Touboul D, Fournié P, et al. Corneal collagen crosslinking in progressive keratoconus: multicenter results from the French National reference center for Keratoconus. J Cataract Refract Surg. 2011;37(12):2137–2143. doi:10.1016/j.jcrs.2011.08.026.
- Spadea L, Salvatore S, Verboschi F, Vingolo EM. Corneal collagen cross-linking followed by phacoemulsification with IOL implantation for progressive keratoconus associated with high myopia and cataract. Int Ophthalmol. 2015;35(5):727–731. doi:10.1007/s10792-015-0107-1.
- Giardini P, Hauranieh N, Gatto C, Tóthová JDA. Tripolymeric corneal coating gel versus balanced salt solution irrigation during cataract surgery: a retrospective analysis. Cornea. 2018;37(4):431. doi:10.1097/ICO.0000000000001480.
- Chanbour W, Harb F, Jarade E. A modified customized rigid gas permeable contact lens to improve visualization during phacoemulsification in ectatic corneas. Med Hypo Disc Inn Ophthalmol. 2020;9(1):1.
- Oie Y, Kamei M, Matsumura N, et al. Rigid gas-permeable contact lens–assisted cataract surgery in patients with severe keratoconus. J Cataract Refract Surg. 2014;40(3):345–348. doi:10.1016/j.jcrs.2014.01.001.
- Bourges J-L. Cataract surgery in keratoconus with irregular astigmatism. Astigmatism-optics, physio manage Croatia Tech. 2012:93–103.
- Andreanos KD, Hashemi K, Petrelli M, Droutsas K, Georgalas I, Kymionis GD. Keratoconus treatment algorithm. Ophthalmol Ther. 2017;6(2):245–262. doi:10.1007/s40123-017-0099-1.
- Mohammadpour M, Heidari Z, Hashemi H. Updates on managements for keratoconus. J Curr Ophthalmol. 2018;30(2):110–124. doi:10.1016/j.joco.2017.11.002.
- Katsoulos C, Karageorgiadis L, Vasileiou N, Mousafeiropoulos T, Asimellis G. Customized hydrogel contact lenses for keratoconus incorporating correction for vertical coma aberration. Ophthalmic Physiol Opt. 2009;29(3):321–329. doi:10.1111/j.1475-1313.2009.00645.x.
- Rathi VM, Mandathara PS, Dumpati S. Contact lens in keratoconus. Indian J Ophthalmol. 2013;61(8):410. doi:10.4103/0301-4738.116066.
- Picot C, Gauthier A, Campolmi N, Delbosc B. Quality of life in patients wearing scleral lenses. J francais d’ophtalmologie. 2015;38(7):615–619. doi:10.1016/j.jfo.2014.10.018.
- Labiris G, Panagiotopoulou E-K, Ntonti P, Taliantzis S. Corneal ectasia following cataract extraction surgery in a patient with keratoconus: a case report. J Med Case Rep. 2019;13(1):1–6. doi:10.1186/s13256-019-2238-x.
- Mamalis N, Brubaker J, Davis D, Espandar L, Werner L. Complications of foldable intraocular lenses requiring explantation or secondary intervention—2007 survey update. J Cataract Refract Surg. 2008;34(9):1584–1591.doi:10.1016/j.jcrs.2008.05.046.
- Leysen I, Bartholomeeusen E, Coeckelbergh T, Tassignon M-JB. Surgical outcomes of intraocular lens exchange: five-year study. J Cataract Refract Surg. 2009;35(6):1013–1018.doi:10.1016/j.jcrs.2009.01.024.
- Oshika T, Inamura M, Inoue Y, et al. Incidence and outcomes of repositioning surgery to correct misalignment of toric intraocular lenses. Ophthalmology. 2018;125(1):31–35. doi:10.1016/j.ophtha.2017.07.004.
- Budo C, Bartels MC, van Rij G. Implantation of Artisan toric phakic intraocular lenses for the correction of astigmatism and spherical errors in patients with keratoconus. Slack Incorporated Thorofare. 2005; NJ.
- Moshirfar M, Grégoire FJ, Mirzaian G, Whitehead GF, Kang PC. Use of Verisyse iris-supported phakic intraocular lens for myopia in keratoconic patients. J Cataract Refract Surg. 2006;32(7):1227–1232.doi:10.1016/j.jcrs.2006.02.017.
- Venter J. Artisan phakic intraocular lens in patients with keratoconus. J Refract Surg. 2009;25(9):759–764.doi:10.3928/1081597X-20090813-01.
- Kato N, Toda I, Hori-Komai Y, Sakai C, Arai H, Tsubota K. Phakic intraocular lens for keratoconus. Ophthalmol. 2011;118(3):605–. e2. doi:10.1016/j.ophtha.2010.08.043.
- Sedaghat M, Ansari-Astaneh M-R, Zarei-Ghanavati M, Davis SW, Sikder S. Artisan iris-supported phakic IOL implantation in patients with keratoconus: a review of 16 eyes. J Refract Surg. 2011;27(7):489–493.doi:10.3928/1081597X-20110203-01.
- Alfonso JF. Myopic phakic STAAR collamer posterior chamber intraocular lenses for keratoconus. J refract surg. 2008;24(9):867.
- Kazutaka Kamiya M, Kimiya Shimizu M, COT WA, Yoshimori Asato M, Tadatoshi Fujisawa M. Phakic toric implantable collamer lens implantation for the correction of high myopic astigmatism in eyes with keratoconus. J refract surg. 2008;24(8):840.
- Kamiya K, Shimizu K, Ando W, Igarashi A, Iijima K, Koh A. Comparison of vault after implantation of posterior chamber phakic intraocular lens with and without a central hole. J Cataract Refract Surg. 2015;41(1):67–72.doi:10.1016/j.jcrs.2014.11.011.
- Kurian M, Nagappa S, Bhagali R, Shetty R, Shetty BK. Visual quality after posterior chamber phakic intraocular lens implantation in keratoconus. J Cataract Refract Surg. 2012;38(6):1050–1057.doi:10.1016/j.jcrs.2011.12.035.
