ABSTRACT
Purpose
To explore the retinal microvasculature of the optic nerve head and macula and their associations with the optic nerve head deformation in high myopia.
Methods
One hundred sixty-seven eyes from patients with high myopia (HM) were enrolled in a cross-sectional study. We have evaluated and measured characteristics like the tilt ratio of the optic disc, interpupillary vascular density (IVD), peripapillary vascular density (PVD), macular vascular density (MVD), subfoveal choroidal thickness (SFCT) and foveal avascular zone (FAZ). The subjects were classified as a non-tilt group (control group) and a tilt group based on the tilt index. The above parameters were utilized to compare the two groups. In addition, we collected the data from the subjects’ right eyes to analyze variance, the Kruskal-Wallis test, and the least significant difference.
Results
The patients were divided into the non-tilt group of ninety-one eyes and the tilt group of seventy-six eyes. We found that the IVD in the tilt group was more significant than in the non-tilt group (t = −2.794, P = .006). On the other hand, the PVD was less in the tilt group than in the non-tilt, especially in the NS, NI and IN directions (tNS = 3.782; tNI = 3.07; tIN = 2.086; P < .05). Interestingly, the values of PVD were the highest in temporal, second in superior and inferior and lowest in nasal. Concerning the fovea-DMVD (including fovea, parafovea and perifovea), we characterized them as more minor in the tilt group when compared to those in the non-tilt group (P < .05).
Conclusion
Herein, we discovered that the retinal microvasculature differed significantly in patients with HM according to the ONH morphology. In this population, lower PVD and thinner SFCT were associated with higher odds of the tilted optic disc. In addition, the other two characteristics, the IVD and DMVD, were affected by the ONH deformation. Finally, we showed that PVD demonstrated better predictability of rapid myopic progression than MVD.
INTRODUCTION
Myopia has been considered one of the major causes of correctable visual impairment worldwide. Sources have indicated a continuously increasing prevalence of myopia and high myopia (HM), especially in the Asian populations.Citation1 Their prevalence globally has been estimated to increase to 49.8%, corresponding to 4.758 billion for myopia and 9.8% and 938 million for HM, respectively, by 2050. The latter represents a significant economic and social burden,Citation2 as it will bring posterior scleral staphyla, paint cracks, chorioretinal atrophy, choroidal neovascularization, macular hole, optic neuropathy. Many studies, in the past, on the morphology of the optic nerve head (ONH) have focused on glaucoma.Citation3–5 However, with the progression of myopia, the ONH deformation is often exhibited by aggravation, especially by the optic disc tilt.Citation6 In such cases, the optic disc tilt appears first, followed by the formation of posterior staphyloma and chorioretinal atrophy.Citation6,Citation7 A general phenomenon in HM, as numerous reports support, is the decrease of retinal microvasculature and blood. This indicates the close relationship between vascular density (VD) and axial elongation.Citation8–10
However, the impact of ONH deformation on microcirculation in these patients is yet to be clarified. Therefore, the present study aims to evaluate the microvasculature of ONH and macula in HM patients and investigate the correlation between ONH deformation and vascular parameters. This article will give us a deep understanding of the internal factors in the morphology of ONH in HM and contribute to the early diagnosis and monitoring of HM.
PATIENTS AND METHODS
The study adhered to the Declaration of Helsinki and was approved by the Ethics Committee of Aier Eye Hospital, Central South University, Changsha, China. The university’s refractive department reviewed the medical records of 167 consecutive myopia patients obtained from May 2020 until January 2021. In addition, on all participants, comprehensive examinations were performed such as slit-lamp biomicroscopy, mydriatic indirect ophthalmoscopy, intraocular pressure (IOP), axial length (AL) (IOL Master 700; Carl Zeiss Meditec, Germany), ultra-widefield fundus imaging (Optos; Daytona P200T, Nikon, Japan), OCTA (RTVue-XR Avanti; Optovue, Fremont, CA, USA), visual acuity and refractive error.
The inclusion criteria were: (1) the spherical equivalent (SE) > −6.00 Diopter Sphere (DS) and the AL > 26 mm; (2) IOP ≤ 21 mmHg; (3) OCTA signal strength index ≥ 50. Conversely, these patients with hypertension, diabetes, systemic connective tissue disorder, any other ophthalmic disease (such as cataract, glaucoma, macular hole, retinal hole, retinal haemorrhage etc.), history of ophthalmic trauma and surgery were excluded from the study.
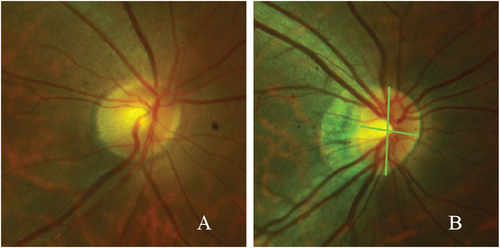
The definitions of the optic disc tilt and their measurements were adopted, as explained by Yarmohammadi et al.Citation11 Briefly, the optic disc tilt was confirmed by the tilt ratio, defined as the ratio between the longest and shortest diameters of the optic disc. In the case of a tilt index > 1.30, the optic disc was considered tilted ().
PARAMETERS FROM OPTOS AND OCTA
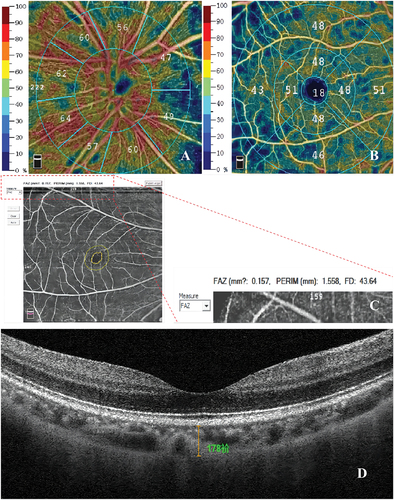
We used Optos to perform digital photography, and the images were exported to the Image-pro Plus (version 6.0) to measure the radian of PPA. The OCTA system automatically enabled the measurement of the PVD, IVD, MVD and FAZ, as illustrated in . It further employed a 6 × 6 mm and a 4.5 × 4.5 mm centred cube scan on the fovea and ONH, respectively. ONH was divided into 8 directions (1-superonasal, SN; 2-nasosuperior, NS; 3-nasoinferior, NI; 4-inferonasal, IN; 5-inferotemporal, IT; 6-temporoinferior, TI; 7-temporosuperior, TS; 8-superotemporal, ST). On the other hand, we divided the macula into 3 sub-districts: fovea, parafovea (nasal, inferior, temporal, superior), and perifovea (nasal, inferior, temporal, superior). Moreover, we measured the following parameters like the FAZ area, a circularity index (AI), and fovea density 300 μm (FD) with the “FAZ” option in the OCTA system. In addition, SFCT was acquired using a manual measurement method. illustrates the acquisition of parameters in detail.
Figure 2. Parameters by OCTA. A) Illustrations of the PVD and IVD; B) Illustration of the MVD. Fovea, parafovea and perifovea (central circle with 0.5 mm radius, around the fovea with inner and outer diameters of 1 mm and 3 mm); C) FAZ area, AI, FD; D. The value of SFCT was measured manually.
Statistical analysis
The statistical analysis was performed with the use of SPSS22.0 software. The obtained data were presented as mean ± standard deviation (X± SD), whereas the analysis of variance (ANOVA) and the least significant difference (LSD) was applied for the evaluation of differences between the groups. The recorded differences were considered statistically significant when P-value was <0.05.
RESULTS
Patients’ demographic data
We analyzed 167 right eyes from patients who met the inclusion and exclusion criteria. Among them, 59 participants were males and 108 females, averaging 25.60 ± 6.04. Furthermore, the SE was measured at −8.81 ± 2.36 DS, whereas the AL was at 26.77 ± 1.19 mm. The division of the patients was the following: the non-tilt group composed of 91 eyes and the tilted disc group of 76 eyes. As shown in , we detected significant differences in parameters like age, AL, SE and tilt index between the two groups (t = 3.828, −3.384, −2.726, −15.151; P = .000, 0.001, 0.007, 0.000; P < .05).
Table 1. Demographic data.
Comparison of the onh microcirculation parameters between the two groups
Our findings, illustrated in and , demonstrated that the highest values of PVD were in temporal, followed by superior and inferior, and the lowest were observed in nasal. Furthermore, we retrieved 26.49 ± 1.22 mm and 27.1 ± 1.07 mm concerning the AL. Moreover, the tilted disc group showcased a bigger IVD than the non-tilt group (t = −2.794; P = .006). On the other hand, the PVD in the tilted disc group was found to be smaller than that in the non-tilt group (t = 3.489; P = .001), especially in the NS, NI and IN directions (t = 3.782, 3.070, 2.086; P = .001, 0.003, 0.039; P < .05).
Figure 3. Microcirculation parameters of PVD.
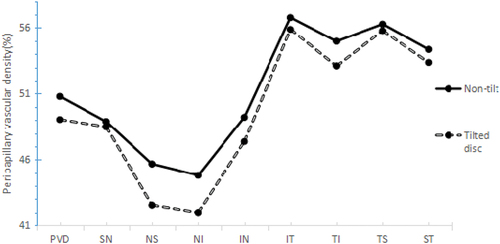
Table 2. Microcirculation parameters of ONH.
Macular microcirculation parameters between the examined patients’ groups
From and , the MVD was the highest in parafovea and perifovea and lowest in the fovea. Yet, we did not detect significant differences in SMVD (fovea, parafovea and perifovea), FAZ area, FD, AI and SFCT between the two groups (P > .05). However, the DMVD (fovea, parafovea and perifovea) in the tilt group were smaller than those in the non-tilt group (t = 2.795, 2.277, 2.007, 2.716; P = .006, 0.024, 0.046, 0.007; P < .05).
Figure 4. Microcirculation parameters of the macula.
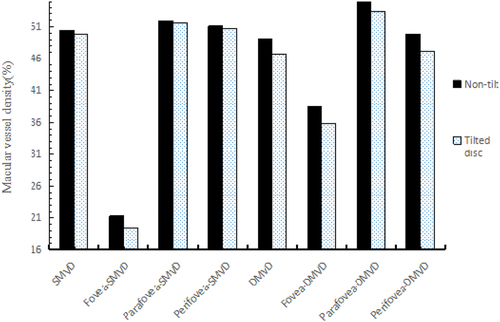
Table 3. Macula microcirculation parameters of macula.
Correlation analysis
The PVD and SFCT were negatively correlated with the tilt index (r = −0.293; P < .05). Similarly, parameters like PVD, DMVD, SFCT had a negative correlation with AL (r = −0.298, −0.219, −0.171, P < .05). Nevertheless, the recorded differences between microcirculation parameters and age or SE were insignificant. The results are demonstrated in , .
Figure 5. Correlation of PVD with AL and tilt index.
Figure 6. Effect of ONH morphology on the retina microcirculation; A) illustration of the fundus; B) OCTA picture of the IVD and PVD; C) OCTA picture of the MVD; A1, B1 and C1 illustrate pictures of the non-tilted disc group; A2, B2 and C2 pictures of the tilted disc group.
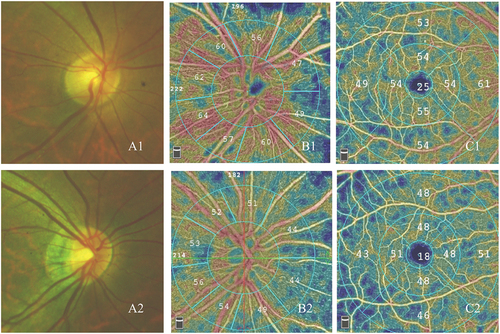
Table 4. Correlation of retinal microcirculation with age, SE, AL and tilt index.
Effect of the tilt disc on the retina microcirculation
The normal ONH without tilt disc is presented in A1, B1 and C1. ONH and macular are rich in non-deficient microvessels. The abnormal ONH with the tilted disc is depicted in A2, B2 and C2. The results confirm a slight decrease in the sub-districts of PVD and MVD.
DISCUSSION
The tilted optic disc has been considered a common characteristic of the ONH morphological changes in HM. Herein we have analyzed the ONH and macular microcirculation in HM and found an increase in IVD, whereas PVD and DMVD were reduced in the tilted disc group. We have also demonstrated strong correlations between tilt index and vascular parameters, such as PVD and SFCT. Considering what has been discovered until now, it can be speculated that ONH deformation can lead to the redistribution of retinal microvessels.
TILTED DISC AFFECTED THE ONH MICROCIRCULATION
Our results have demonstrated that reduced PVD is associated with higher odds of tilted optic discs’ development. Notably, the PVD value in the tilt group was smaller than that in the non-tilt group, even more in the NS, NI and IN directions. The latter could provoke direct mechanical damage to the peripapillary microvessels during the development of the ONH deformation. ONH capillary is vital in supplying optic nerves or axons of retinal ganglion cells with blood. Based on the evidence, it has been suggested an association between peripapillary hemoperfusion loss with PRNFL thinning. The authors report a significantly positive correlation between PRNFL thickness and PVD. They further claim that thinning of PRNFL may affect oxygen demand or vascular supply in the peripapillary, thereby triggering vascular adjustment of the retina via autoregulatory mechanisms.Citation12,Citation13 Notably, changes in microcirculation perfusion have critical impacts on HM optic neuropathy. In addition, Sawada et al. discovered that the recorded visual field damage was associated with the ONH deformation in myopia combined with glaucoma.Citation14 Yet, it was not associated with any diopter in myopia. Thus, the peripapillary capillary perfusion reduction may be an intrinsic cause of augmenting the susceptibility to HM optic neuropathy. However, in contrast to PVD, the tilt group showcased a significantly higher IVD than the non-tilt group. Therefore, we assumed that the arterial circle of Zinn-Haller mainly supplied the IVD with abundant collateral circulation, while the PVD was derived from the central retinal artery.
Furthermore, Ishida et al. confirmed Zinn-Haller’s role as the leading vascular supplier for the ONH at the lamina cribrosa. At the same time, the IVD was found to be located in the anterior lamina cribrosa.Citation15 The latter means that the arterial circle of Zinn-Haller could maintain rich blood perfusion after the loss of the peripapillary choroidal capillary. Therefore, the increased IVD might explain the non-occurrence of the pathology of optic nerve degeneration in all high myopic patients.
TILTED DISCS AFFECTED THE MACULA MICROCIRCULATION
It is widely accepted that retinal microcirculation in myopic eyes has degenerated before the apparent retinopathy while the AL increases. Similarly, the obtained data demonstrated that the tilt group’s DMVD (fovea, parafovea and perifovea) was smaller than the non-tilt group. Further, we did not find significant changes in parameters such as SMVD, FAZ and SFCT. The underlying association mechanism between the tilted disc and macular microcirculation is yet to be clarified. A reasonable explanation may be the different blood microcirculation of the SMVD and DMVD.
On the other hand, the choroidal capillary provides the main vascular supply for the DMVD, while the SMVD is derived from the central artery of the retina. We further discovered that reduced SFCT values were associated with higher odds of the tilted optic discs’ occurrence, but there were not as such observations as with FAZ and MVD. So FAZ remained stable during the realization of this study. Also, it contains photoreceptors responsible for visual sensitivity and central visual acuity. Its size and shape partly reflect the status of the macular microcirculation, which is most likely associated with maculopathy.Citation16 Other reports have shown that altered retinal degeneration caused by HM can lead to FAZ enlargement, shedding capillaries, and reduction of macular microcirculation.Citation17 As previously described, most of the oxygen supplied to the FAZ comes from the choroid rather than the retinal circulation. We found small changes in the SFCT. Perhaps FAZ significantly changes when the choroid occurs with extreme atrophy. Therefore, it can be inferred that the choroid’s structure and functional stability have a critical effect on FAZ. In that sense, Sun et al. also found that FAZ were not noticeable in the early phase of HM.Citation18 In another report, Yilmaz et al. l discovered a significantly negative correlation between AI and age.Citation19
Additionally, and from a clinical point of view, there is an increasing tendency to observe myopic maculopathy in older patients. FAZ has an individual variability in young people,Citation20 and various factors such as gender, AL, retinal thickness and macular blood flow may impact to a different extent on FAZ,Citation21 unlike to suggest that ONH deformation and mechanical stretching could be the only mechanism for FAZ changes. Other factors, such as age, maybe more involved, but the last allegation requires further investigation.
We assume that the primary focus on the peripapillary microcirculation parameter would allow better predictability of high myopic progression than the macular microcirculation parameter. First, the blood supply of the ONH and macula was different. Secondly, the metabolism of the macula is primarily active in the retina, and its blood supply may be more stable than that of the peripapillary region.Citation22 Last, it may be associated with the onset region of the pathological changes in HM, and from there to speculate that the ONH microcirculation changes can predate those of macula.
Our study has some limitations. First, since the current investigation is a retrospective study, the longitudinal data were unavailable, leaving the conclusion’s causality unclear. Then, the age distribution of the subjects was biased in the range between 18 and 39 years, leaving a slight probability of congenital tilted disc not being completely ruled out. Subsequently, it might not reflect the true representative of the entire population with HM. Finally, the tilted optic disc was measured in two dimensions, which might not exactly present the shapes of the three-dimensional optic disc. Hence, developing a three-dimensional method for measuring the tilt ratio is very important.
CONCLUSION
In conclusion, after the investigation of the retinal microcirculation distribution that included ONH and macula area in young high myopic patients with different shapes of ONH, we discovered, for the first time, the presence of tilted optic discs correlated positively with a higher IVD and lower PVD values (especially in NS, NI and IN directions). Moreover, PVD showed better predictability of high myopic progression compared to MVD. We also demonstrated strong correlations between tilt index and vascular parameters, such as PVD and SFCT. Our findings indicated that young patients with HM, especially those with tilted optic discs, should be regarded as a high priority and that long-term and regular follow-up is essential. As a result, the findings establish a good foundation for proceeding with the research on following trends in tilt ratio and other retinal vascular parameters.
AUTHORS’ CONTRIBUTIONS
WT & XD designed the research study; WT wrote the paper; WT, & YL analyzed and interpreted the data; XD &YL contributed to critical revision of the article; XD & YL obtained and provided administrative, technical or logistic support. All authors approved the manuscript.
DISCLOSURE STATEMENT
No potential conflict of interest was reported by the author(s).
Additional information
Funding
REFERENCES
- Wong YL, Saw SM. Epidemiology of pathologic myopia in Asia and worldwide.[J]. Asia Pac J Ophthalmol (Phila). 2016;5(6):394–402. doi:10.1097/APO.0000000000000234.
- Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042.doi:10.1016/j.ophtha.2016.01.006.
- Lee JE, Sung KR, Park JM, et al. Optic disc and peripapillary retinal nerve fiber layer characteristics associated with glaucomatous optic disc in young myopia. Graefes Arch Clin Exp Ophthalmology 2017;255(3):591–598. 10.1007/s00417-016-3542-4
- Lee KM, Choung HK, Kim M, et al. Positional change of optic nerve head vasculature during axial elongation as evidence of lamina cribrosa shifting: boramae myopia cohort study report 2. Ophthalmology. 2018;125(8):1224–1233.doi:10.1016/j.ophtha.2018.02.002.
- Shoeibi N, Moghadas SN, Daneshvar R, et al. Visual field assessment in high myopia with and without tilted optic disc.[J]. Clin Exp Optom. 2017;100(6):690–694.doi:10.1111/cxo.12511.
- Kim T-W, Kim M, Weinreb RN, et al. Optic disc change with incipient myopia of childhood.[J]. Ophthalmology. 2012;119(1):21–26.doi:10.1016/j.ophtha.2011.07.051.
- Chen Q, He J, Yin Y, et al. Impact of the morphologic characteristics of optic disc on choroidal thickness in young myopic patients. Invest Ophthalmol Vis Sci. 2019;60(8):2958–2967.doi:10.1167/iovs.18-26393.
- Avetisov ES, Savitskaya NF. Some features of ocular microcirculation in myopia.[J]. Ann Ophthalmol. 1977;9:1261–1264.
- Azemin MZ, Daud NM, Ab HF, et al. Influence of refractive condition on retinal vasculature complexity in younger subjects.[J]. ScientificWorldJournal. 2014;2014:783525. doi:10.1155/2014/783525.
- Shimada N, Ohno-Matsui K, Harino S, et al. reduction of retinal blood flow in high myopia.[J]. Graefes Arch Clin Exp Ophthalmol 2004;242(4):284–288. 10.1007/s00417-003-0836-0
- Nie F, Ouyang J, Tang W, et al. Posterior staphyloma is associated with the microvasculature and microstructure of myopic eyes. Graefes Arch Clin Exp Ophthalmol 2021;259(8):2119–2130. 10.1007/s00417-020-05057-0
- Yarmohammadi A, Zangwill LM, Diniz-Filho A, et al. Relationship between optical coherence tomography angiography vessel density and severity of visual field loss in glaucoma. Ophthalmology. 2016;123(12):2498–2508.doi:10.1016/j.ophtha.2016.08.041.
- Lee EJ, Lee KM, Lee SH, et al. OCT angiography of the peripapillary retina in primary open-angle glaucoma. Invest Ophthalmol Vis Sci. 2016;57(14):6265–6270.doi:10.1167/iovs.16-20287.
- Sawada Y, Hangai M, Ishikawa M, et al. Association of myopic deformation of optic disc with visual field progression in paired eyes with open-angle glaucoma. PLoS One. 2017;12(1):e170733.doi:10.1371/journal.pone.0170733.
- Ishida T, Jonas JB, Ishii M, et al. Peripapillary arterial ring of zinn-Haller in highly myopic eyes as detected by optical coherence tomography angiography.[J]. Retina. 2017;37(2):299–304.doi:10.1097/IAE.0000000000001165.
- Scarinci F, Varano M, Parravano M. Retinal sensitivity loss correlates with deep capillary plexus impairment in diabetic macular ischemia. J Ophthalmol. 2019;2019:7589841. doi:10.1155/2019/7589841.
- He J, Chen Q, Yin Y, et al. Association between retinal microvasculature and optic disc alterations in high myopia.[J]. Eye (Lond). 2019;33(9):1494–1503.doi:10.1038/s41433-019-0438-7.
- Sun J, Wang J, You R, et al. Is the retinal vasculature related to beta-peripapillary atrophy in nonpathological high myopia? an optical coherence tomography angiography study in Chinese adults. J Ophthalmol. 2018;2018:7895238. doi:10.1155/2018/7895238.
- Yilmaz H, Karakurt Y, Icel E, et al. Normative data assessment of vessel density and foveal avascular zone metrics using angioscan software. Curr Eye Res. 2019;44(12):1345–1352.doi:10.1080/02713683.2019.1639769.
- Falavarjani KG, Shenazandi H, Naseri D, et al. Foveal avascular zone and vessel density in healthy subjects: an optical coherence tomography angiography study. J Ophthalmic Vis Res. 2018;13(3):260–265.doi:10.4103/jovr.jovr_173_17.
- Zhou Y, Zhou M, Gao M, et al. Factors affecting the foveal avascular zone area in healthy eyes among young Chinese adults. Biomed Res Int. 2020;7361492. doi:10.1155/2020/7361492.
- Wang X, Kong X, Jiang C, et al. Is the peripapillary retinal perfusion related to myopia in healthy eyes? A prospective comparative study. BMJ Open. 2016;6(3):e10791.doi:10.1136/bmjopen-2015-010791.