Specific immunity of the mammalian host primarily consists of B and T lymphocytes that ensure specific elimination of foreign entities and establish defense memory during reinfection. Dysregulation of B and T lymphocytes does not only change susceptibility to microbial infection, but also causes a wide range of immunopathology that affects various organs and organ systems. On the other hand, antibodies generated by B cells (monoclonal and polyclonal) or antibodies derived from chimeric molecules against specific antigens have a wide range of therapeutic applications. This issue of International Reviews of Immunology describes the role of antibodies and T cell subsets in autoimmune disease pathogenesis and also describes therapeutic potential of antibodies in organ transplantation ().
Figure 1. Antibodies and T cell subsets in autoimmune disease, organ transplant, and immune-therapy. ANA: anti-nuclear antibody; ATG: antithymocytes globulins; RA: rheumatoid arthritis; SLE: systemic lupus erythematosus; Th: T helper; Threg: T helper regulatory.
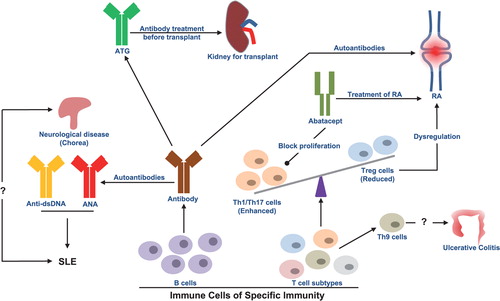
Systemic lupus erythematosus (SLE) is an autoimmune disease characterized by the presence of various autoreactive antibodies such as antinuclear, anti-dsDNA, antiphospholipid antibodies, and so on. The first review article of this issue by Athanasopoulos et al. discusses the association of SLE with the rare neurological disorder known as Chorea. The article specifically discusses the symptoms and treatment of SLE and associated Chorea. This article will be useful for clinicians treating these complex autoimmune diseases ().
Organ replacement is one of best options for patients suffering from organ failure. However, organ transplants are associated with challenges such as organ rejection due to host immunity, and the success of an organ transplant solely depends on management of host immunity. Although immense technological advancements in surgical methods and discovery of novel immunosuppressive drugs have been achieved in recent past, the success rate is still substantially low.
The second review article in this issue, written by Ducloux et al., describes the potential use of old drug antithymocytes globulins (ATG), which facilitate T cell depletion in organs to reduce graft rejection, particularly with kidney transplants. The authors highlighted the challenges linked with ATG treatment, such as dosage of ATG, nondepletive effects of ATG, and so on. This review discusses the positive and negative aspects associated with ATG. This review may benefit clinicians who are involved in organ transplantation and immunologists who are looking for a better fundamental understanding and to develop novel therapeutic interventions ().
T cell subsets play a pivotal role in immunity against infectious and noninfectious diseases and in the pathogenesis of autoimmune diseases, organ transplants, and so on. The third review article in this issue by Shohan et al. discusses the role of Th9 cells in ulcerative colitis, a new Th cell type which differentiates to Th9 in the presence of IL-4 and TGFβ and produces IL-9. IL-9 is suggested to promote disruption of the epithelial barrier in the intestine and cause inflammation leading to ulcerative colitis; however, the underlying molecular mechanism is unclear. The review article is useful to the broad reader of immunology, but is particularly useful to mucosal immunologists ().
Rheumatoid arthritis (RA) is a result of several factors such as genetic, epigenetics along with environmental factors that predispose patients to this incurable autoimmune disease. The last review article of this issue by Langdon et al. describes how a chimeric fusion protein (consisting of a portion of CTLA-4 and an Fc portion of immunoglobulin) known as Abatacept downregulates proliferation of inflammatory Th cells. The authors describe the differential effects of Abatacept in the population and discuss better strategies for the management of a different category of RA patitents ().
References
- Athanasopoulos E, Kalaitzidou I, Vlachaki G, Stefanaki S, Tzagkaraki A, Niotakis G, Tritou I, Ladomenou F. Chorea revealing systemic lupus erythematosus in a 13-year-old boy: a case report and short review of the literature. Int Immunol. 2018;37(4):177–182.
- Ducloux D, Bamoulid J, Daguindau E, Rebibou JM, Courivaud C, Saas P. Antithymocytes globulins: time to revisit its use in kidney transplantation? Int Immunol. 2018;37(4):183–191.
- Shohan M, Elahi S, Shirzad H, Rafieian-Kopaei M, Bagheri N, Soltani E. Th9 cells: probable players in ulcerative colitis pathogenesis. Int Immunol. 2018;37(4):192–205.
- Langdon K, Haleagrahara N. Regulatory T cell dynamics with Abatacept treatment in rheumatoid arthritis. Int Immunol. 2018;37(4):206–214.
