Abstract
Purpose: Urinary biomarkers of renal injury urinary may identify loss of renal function following nephron-sparing surgery (NSS). This study was designed to evaluate whether urinary l-type fatty acid-binding protein (l-FABP) is an early biomarker of loss of renal function after NSS. Specifically, the kinetics of urinary l-FABP level after NSS and its correlation with factors related to ischemic renal injury were analyzed.
Methods: This study prospectively evaluated 18 patients who underwent NSS between July and December 2014, including 12 who underwent laparoscopic and six who underwent robot-assisted partial nephrectomy. Urinary l-FABP concentrations were measured preoperatively and 1, 2, 3, 6, 12, 24, 48, and 72 h after renal artery declamping. Loss of renal function loss was calculated by comparing the effective renal plasma flow, as determined by 99mTc-mercaptoacetyltriglycine (MAG3) clearance, on the operated and normal sides. The decrease in estimated glomerular filtration rate from before surgery to six months after surgery was also measured.
Results: Urinary l-FABP concentration peaked within 2 h of declamping, which may quantify nephron damage caused by ischemia. The decrease in MAG3 reduction ratio correlated with both the ischemia time and peak urinary l-FABP concentration. Peak urinary l-FABP concentration showed a significant correlation with MAG3 reduction ratio.
Conclusions: l-FABP is a suitable urinary biomarker for predicting the extent of ischemic renal injury.
Introduction
Nephron-sparing surgery (NSS), which aims to minimize the loss of renal function, has recently become the standard treatment for localized small renal tumors and is considered an attractive alternative to radical nephrectomy.Citation1,Citation2 However, NSS is associated with a risk of ischemic renal injury. Although serum creatinine concentration and estimated glomerular filtration rate (eGFR) are considered indicators of renal function after NSS,Citation3,Citation4 these indicators measure total renal function, and a significant increase in serum creatinine concentration may not be apparent until eGFR drops to approximately 30% of its normal rate. The precise evaluation of renal damage therefore requires split renal function tests.
Early detection of reduced renal function enables early intervention to preserve renal function. Such interventions include nutritional guidance and the measurement of complications such as hypertension and diabetes mellitus. Urinary biomarkers of acute kidney injury (AKI) may provide an earlier evaluation of the loss of renal function. One of these urinary biomarkers, l-type fatty acid-binding protein (l-FABP) concentration, may enable early detection of loss of renal function after NSS. This study therefore analyzed the kinetics of urinary l-FABP after NSS and whether urinary l-FABP level correlates with factors related to ischemic renal injury. As it was impossible to evaluate both changes in urinary l-FABP and ischemia time in the same patient, we investigated urinary l-FABP in patients exposed to ischemia times ranging from 8.1 to 52 min.
Materials and methods
Of the 18 patients who underwent NSS at our hospital from July to December 2014, 12 underwent laparoscopic partial nephrectomy and six underwent robot-assisted partial nephrectomy. shows the characteristics and surgical outcomes of all 18 patients. The protocol of this prospective study was approved by the research committee at our institute.
Table 1. Patient characteristics and surgical outcomes.
NSS at our hospital includes insertion of an ipsilateral ureteral catheter to cool the kidney and check for leakage of urine by retrograde instillation of indigo carmine. Urinary l-FABP concentrations were measured preoperatively and 1, 2, 3, 6, 12, 24, 48, and 72 h after renal artery declamping. At each time point, a spot urine sample was obtained from the ureteral catheter and l-FABP concentrations measured by enzyme-linked immunosorbent assay using the Human l-FABP ELISA Kit (CMIC, Tokyo, Japan). All patients underwent 99mTc-mercaptoacetyltriglycine (MAG3) scintigraphy before and six months after surgery. Loss of renal function was determined by comparing the effective renal plasma flow (ERPF) on the operated and normal sides using MAG3 (i.e., the MAG3 reduction ratio; presented as a percentage), using the formula:
eGFR was also measured before and six months after surgery, and the percentage decrease (i.e., eGFR reduction ratio) was calculated using the formula:
To determine whether peak urinary l-FABP concentration was predictive of renal damage, the correlations between l-FABP concentrations and ischemia time, MAG3 reduction ratio, and eGFR reduction ratio were calculated.
All statistical analyses were performed using the Statistical Package for the Social Sciences, version 21.0 (IBM, Armonk, NY). Differences in continuous variables were compared using the Mann–Whitney U test; correlations between data sets were determined by simple linear regression analysis and determining Spearman’s rank correlation coefficient. A p value <.05 was considered statistically significant.
Results
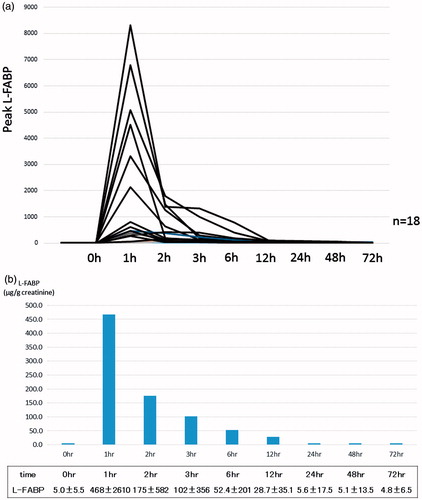
shows the temporal changes in urinary l-FABP in all patients. Urinary l-FABP concentration peaked at a mean 1434 μg/g creatinine (range, 52.7–8305.1 μg/g creatinine) 1–2 h after renal artery declamping. In all patients, urinary l-FABP returned to baseline level within 24 h. shows mean l-FABP concentrations.
Figure 1. Effects of NSS on urinary l-FABP concentrations. (a) Temporal changes in urinary l-FABP and (b) mean l-FABP concentrations.
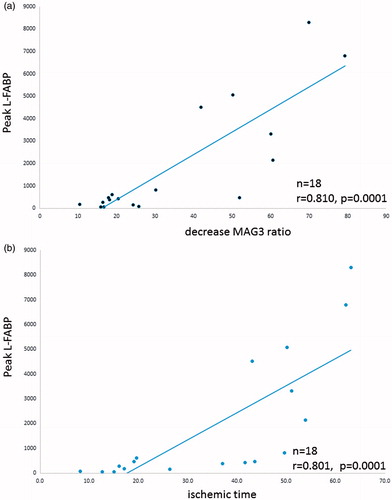
The mean eGFR was 63.9 mL/min/1.73 m2 (range, 37–97 mL/min/1.73 m2) before NSS and 59.0 mL/min/1.73 m2 (range, 34–93 mL/min/1.73 m2) six months after NSS. The mean eGFR reduction ratio was 8.4% (range, 0.0–23.1%). The ERPFs on the operated side before and six months after surgery were 180.5 and 133.8 mL/min per 1.73 m2, respectively; whereas the ERPFs on the normal side before and six months after surgery were 175.5 and 198.1 mL/min per 1.73 m2, respectively. The mean MAG3 reduction ratio was 66.0% (range, 10.5–79.3%). Peak urinary l-FABP concentrations correlated with the MAG3 reduction ratio (r = .810, p< .0001) and the period of ischemia (r = .801, p< .0001; ). In contrast, the eGFR reduction ratio did not correlate with the MAG3 reduction ratio or the period of ischemia.
Discussion
This study showed that urinary l-FABP concentration may be a useful marker in the evaluation of early renal dysfunction due to ischemia in patients undergoing NSS. The l-FABP concentration quickly peaked after the renal artery clamping procedure, returning to baseline within 24 h. The findings reported in this study indicate that these changes in l-FABP concentration can be used to quantify nephron damage caused by ischemia.
It is critical to appropriately evaluate renal dysfunction in the operated kidney after partial nephrectomy, because a decrease in renal function of this kidney can lead to hyper-filtration and damage to the non-operated kidney. However, total renal function is frequently masked by the compensating activity of the non-operated kidney. Serum creatinine concentration and creatinine clearance rate in rats with acute renal failure were found to return to baseline levels after a transient deterioration.Citation5 Histological examination showed essentially normal tubular morphology at four and eight weeks after injury, with tubulointerstitial fibrosis developing at 40 weeks. Furthermore, the urine-concentrating ability continued to be poor and urinary proteins were present for a long period of time. This indicated that renal structures on the operated side, including the glomeruli and peritubular capillaries, were permanently damaged and that this damage could not be precisely predicted using general biochemical markers such as creatinine and eGFR.
Nuclear scintigraphy with MAG3 is a valid technique for separately evaluating nephron damage caused by ischemia. Nuclear scintigraphy was found to be the only method allowing quantification of actual magnitude of renal function lost by the treated kidney.Citation6 However, nuclear scintigraphy has several drawbacks, including its cost and exposure of patients to radiation.
The increase in urinary l-FABP concentration may be caused by the development of tubular ischemia because of reduced blood flow in the peritubular capillaries. l-FABP concentration has been found to increase immediately after cardiac surgery in patients with AKI, from a baseline of 11.19 ng/mL to a peak 244.4 ng/mL, and to gradually decrease to 33.66 ng/mL after 48 h.Citation7 In patients without AKI, however, l-FABP concentrations did not change markedly. Our findings were similar, in that mean baseline l-FABP concentration was 5.0 ng/mL, peaking at 468 ng/mL at 1 h after declamping, providing evidence that l-FABP may be a rapid and sensitive marker of AKI.
Urinary l-FABP concentration is elevated not only by ischemic damage but also by exposure to agents toxic to the kidneys. For example, exposure of transgenic mice with human l-FABP to ischemia increased urinary l-FABP exponentially within 2 h, whereas blood urea nitrogen (BUN) levels were higher at 48 h.Citation8 l-FABP was elevated 100-fold at 1 h after reperfusion relative to baseline even after five minutes of ischemia. In non-diabetic patients with chronic kidney disease (CKD), urinary l-FABP strongly correlated with renal disease progression.Citation9 l-FABP may also reflect renal injury during early stages of nephropathy in diabetic patients, even in patients who are normoalbuminuric.Citation10
Recently identified urinary biomarkers of AKI include N-acetyl-d-glucosaminidase (NAG), α1-microglobulin, β2-microglobulin, neutrophil gelatinase-associated lipocalin (NGAL), l-FABP, and kidney injury molecule-1 (KIM-1). Although NGAL is a useful biomarker of AKI,Citation11,Citation12 urinary NGAL may be produced extrarenally in response to systemic stress. As NGAL is frequently detected in the urine for reasons other than renal failure, its clinical significance is unclear.Citation13 On the other hand, urinary l-FABP is not affected by urinary sediment and can therefore be measured in spot urine samples. Furthermore, urinary l-FABP measurements are highly reproducible.Citation14 Finally, rather than fluctuating with exercise,Citation15 the urinary l-FABP concentration is extremely stable. All of these reasons indicate that urinary l-FABP may be the most stable and reproducible biomarker for evaluating early renal dysfunction.
In temporal profile of urinary biomarkers in patients who develop acute injury after cardiopulmonary bypass, l-FABP was peaked earlier than KIM-1 and IL-18.Citation16 Urinary l-FABP was the only biomarker in human kidney transplant recipients that correlated with increases in reciprocal units of peritubular capillary blood flow (r = .933, p<.0001).Citation17 On the other hand, NAG (r = .513, p = .09), α1-microglobulin (r = .235, p = .46), and β2-microglobulin (r = −.007, p = .98) were not significantly correlated with it. Furthermore, urinary l-FABP was significantly correlated with ischemia times in this patients (r = .939, p<.0001). Similarly, this study found a significant correlation between peak urinary l-FABP and ischemia times (r = .801, p<.0001). From these, urinary l-FABP may be most sensitive than other markers in the evaluation of early renal dysfunction for AKI in patients undergoing NSS.
The percentage reduction in MAG3 correlated with both ischemia time and peak l-FABP concentration. Similarly, the rate of MAG3 decrease during the early postoperative period was found to correlate significantly with the logarithm of the induction l-FABP rate (r = .6337).Citation18 These findings provide further evidence that peak l-FABP concentration can predict the extent of ischemic renal injury following NSS. Unfortunately, MAG3 cannot be repeatedly measured because of its high cost. Postoperatively, the ERPF on the operated side decreased, being lower at one year than at three months after NSS and subsequently recovering in only a small percentage of patients.Citation6 Compensatory hypertrophy occurs after partial nephrectomy. Therefore, split renal function was evaluated by nuclear scintigraphy six months after NSS. Evaluating split renal function is particularly important in patients who have CKD before surgery, and in those who develop CKD after surgery. Ischemic damage and postischemic renal failure may contribute to the development of hypertension and cardiovascular disease.Citation19 As CKD is directly related to prognosis, it is important to predict residual renal function at an early stage after surgery. In the present study, the peak l-FABP concentration correlated significantly with the MAG3 reduction ratio. A higher peak l-FABP concentration would therefore be associated with a greater decrease in postoperative renal function. In such patients, it is necessary to pay close attention to the management of any complications, to provide nutritional guidance and to implement an exercise regimen. These early interventions and preventive measures are expected to inhibit the progression of CKD.
l-FABP can also be used as an index for evaluating surgical procedures in NSS. Various techniques are used to protect renal function during surgery. For example, several methods may be used to shorten the ischemia time, such as early unclamping,Citation20 gasless laparoendoscopic single port surgery,Citation21 and zero ischemia anatomical partial nephrectomy.Citation22 Additionally, intracorporeal cooling with ice slush may be used.Citation23 Although the effectiveness of these methods has been evaluated by measuring serum creatinine concentration or eGFR, our findings suggest that urinary l-FABP may accurately determine renal function after NSS.
The primary limitations of the present study are its preliminary nature and small sample size. Large-scale trials are needed to determine whether urinary l-FABP can predict the severity of ischemic renal injury following NSS.
Conclusion
The present study has shown that l-FABP concentration is an effective urinary biomarker for predicting the extent of ischemic renal injury following NSS.
Disclosure statement
The authors have no conflicts of interest to declare.
Ethical approval
This article is a retrospective study. This article does not contain any studies with human participants performed by any of the authors.
Informed consent
This article is a retrospective study. Accordance with the guidelines of the Ethical Committee in our hospital, we decided to consent by posting around the examination room.
References
- Patard JJ, Shvarts O, Lam JS, et al. Safety and efficacy of partial nephrectomy for all T1 tumors based on an international multicenter experience. J Urol. 2004;171:2181–2185.
- Leibovich BC, Blute ML, Cheville JC, Lohse CM, Weaver AL, Zincke H. Nephron sparing surgery for appropriately selected renal cell carcinoma between 4 and 7 cm results in outcome similar to radical nephrectomy. J Urol. 2004;171:1066–1070.
- Gill IS, Desai MM, Kaouk JH, et al. Laparoscopic partial nephrectomy for renal tumor: Duplicating open surgical techniques. J Urol. 2002;167:469–476.
- Bhayani SB, Rha KH, Pinto PA, et al. Laparoscopic partial nephrectomy: Effect of warm ischemia on serum creatinine. J Urol. 2004;172:1264–1266.
- Basile DP, Donohoe D, Roethe K, Osborn JL. Renal ischemic injury results in permanent damage to peritubular capillaries and influences long-term function. Am J Physiol Ren Physiol. 2001;281:F887–F899.
- Porpiglia F, Fiori C, Bertolo R, et al. Long-term functional evaluation of the treated kidney in a prospective series of patients who underwent laparoscopic partial nephrectomy for small renal tumors. Eur Urol. 2012;62:130–135.
- Matsui K, Kamijo-Ikemori A, Kimura K, Yasuda T, Kimura K. Usefulness of urinary biomarkers in early detection of acute kidney injury after cardiac surgery in adults. Circ J. 2012;76:213–220.
- Negishi K, Noiri E, Doi K, et al. Monitoring of urinary l-type fatty acid-binding protein predicts histological severity of acute kidney injury. Am J Pathol. 2009;174:1154–1159.
- Kamijo A, Kimura K, Sugaya T, Kimura K. Urinary l-type fatty acid binding protein as a new clinical marker for the progression of chronic renal disease. J Lab Clin Med. 2004;165:23–30.
- Suh JS, Kim SH, Cho KS, et al. Urinary markers in the early stage of nephropathy in patients with childhood-onset type 1 diabetes. Pediatr Nephrol. 2016;31:623–631.
- Mishra J, Ma Q, Prada A, et al. Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J Am Soc Nephrol. 2003;14:2534–2543.
- Supavekin S, Zhang W, Kucherlapati R, Kaskel FJ, Moore LC, Devarajan P. Differential gene expression following early renal ischemia/reperfusion. Kidney Int. 2003;63:1714–1724.
- Hasse M, Bellomo R, Devarajan P, Schlattmann P, Haase-Fielitz A. NGAL Meta-analysis Investigator Group. Accuracy of neutrophil gelatinase-associated lipocalin (NGAL) in diagnosis and prognosis in acute kidney injury: A systematic review and meta-analysis. Am J Kid Dis 2009;54:1012–1024.
- Kamijo-Ikemori A, Sugaya T, Obama A, et al. Liver-type fatty acid-binding protein attenuates renal injury induced by unilateral ureteral obstruction. Am J Pathol. 2006;169:1107–1117.
- Hiraki K, Kamijo-Ikemori A, Yasuda T, et al. Moderate-intensity single exercise session does not induce renal damage. J Clin Lab Anal. 2013;27:177–180.
- Devarajan P. Review: Neutrophil gelatinase-associated lipocalin: A troponin-like biomarker for human acute kidney injury. Nephrology (Carlton). 2010;15:419–428.
- Yamamoto T, Noiri E, Ono Y, et al. Renal l-type fatty acid-binding protein in acute ischemic injury. J Am Soc Nephrol. 2007;18:2894–2902.
- Takai S, Yamamoto T, Matsukawa Y, Gotoh M. Evaluation of the ischemic renal injury after nephron-sparing surgery using dynamic renal scintigraphy and 1-type fatty acid binding protein. J Urol. 2013;189:e261.
- Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305.
- Gill IS, Kamoi K, Aron M, Desai MM. 800 Laparoscopic partial nephrectomies: A single surgeon series. J Urol. 2010;183:34–41.
- Kihara K. Application of gasless laparoendoscopic single port surgery, GasLESS, to partial nephrectomy for renal cell carcinoma: GasLESS-clampless partial nephrectomy as a multiply satisfactory method. Int J Urol. 2012;19:3–4.
- Gill IS, Patil MB, Abreu AL, et al. Zero ischemia anatomical partial nephrectomy: A novel approach. J Urol. 2012;187:807–814.
- Kaouk JH, Samarasekera D, Krishman J, et al. Robotic partial nephrectomy with intracorporeal renal hypothermia using ice slush. Urology. 2014;84:712–718.