Abstract
Background
Smoking remains a powerful risk factor for death in end-stage renal disease (ESRD) and so is the presence of fluid overload. The relationship between smoking, blood pressure (BP) control and volume overload is insufficiently explored in patients on maintenance dialysis.
Methods
This is a retrospective cross-sectional cohort study, utilizing existing patients’ data generated during routine ESRD care, including bimonthly protocol bioimpedance fluid assessment of the volume status.
Results
We analyzed the data of 63 prevalent patients receiving thrice weekly maintenance hemodiafiltration treatments at one rural dialysis unit in Hungary. The cohort’s mean ± SD age was 61.5 ± 15.3 years; 65% male, 38% diabetic, with a mean arterial blood pressure (MAP) 99.5 ± 16.8 mmHg and Charlson score 3.79 ± 2.04. Of these, 38 patients were nonsmokers and 25 smokers. The nonsmokers’ MAP was 94.3 ± 14.0 versus smokers’ 105.9 ± 18.9 mmHg (p: .002); nonsmokers took an average 0.73 ± 0.92 antihypertensive medications vs. 1.73 ± 1.21 for smokers (p: .0001). The distribution of taking more antihypertensive medications is skewed toward a higher number among the smokers (2x5 chi square p: .004). By bioimpedance spectroscopy, nonsmokers had an average 10.93 ± 7.65 percent overhydration (OH) over the extracellular space compared to 17.63 ± 8.98 in smokers (p: .005).
Conclusions
Smoking may be a significant mediator of not only BP but also of chronic fluid overload in ESRD patents. Additional, larger studies are needed to explore the mechanistic link between smoking and volume overload.
Introduction
The cardiovascular mortality rate of dialysis patients is about 10 to 20 times higher than that of the general population based on USRDS data [Citation1]. The study by Foley reporting this excess risk [Citation1] has been cited over 1600 times ever since 1998 to justify research and to investigate the cardiovascular component of illness in ESRD simply because the degree of increase in mortality is so astounding. Smoking represents a superimposed, additional layer of risk and been found to be a major cause of mortality in the dialysis population by others [Citation2]. For patients with chronic kidney disease the risk of cardiovascular events was 36% higher among smokers than nonsmokers in a large (n: 6,245) observational study and the risk of death was increased by 48% (RR, 1.48; 95% CI, 1.30–1.70) [Citation3]. Dialysis patients who smoked had an 65% higher hazard ratio for mortality in a meta-analysis [Citation2] using the data of 26 studies. It appears, therefore, that smoking is a particularly toxic habit for those who have kidney disease.
Smoking seems to exert its deleterious effects through the acceleration of atherosclerotic disease. It is highly controversial whether hypertension as defined by high pre-HD blood pressure readings is an independent risk factor for mortality in HD patients – in fact, low pre-HD may be associated with higher mortality. The contribution of hypertension to the observed high risk in cardiovascular mortality in dialysis patients being uncertain, it is logical to look for additional mechanisms. In this study, we set out to investigate possible relationships between smoking and overhydration, an established independent predictor of increased cardiovascular mortality in this population. We devised a data review to see if smoking simply results in vasoconstriction or perhaps another mechanism may contribute to the development of hypertension and increased mortality.
Methods
This is a cross sectional study of existing clinical data obtained through the clinical practice at a for-profit chain dialysis center in a rural environment in Hungary where the overall prevalence of smoking was 28% in 2014 [Citation4]. The study was approved both by the commercial clinical provider (Fresenius Medical Care), as well as the medical Research Council of Hungary (equivalent to an independent review board), TUKEB permit number 27677-1/2019/EKU. Only aggregate data were utilized safeguards were in place to ensure patient anonymity and to prevent patient identification. All data collected were obtained as part of general practice and no additional data was used exclusively for research purposes.
We reviewed the data of 63 prevalent chronic patients receiving in-center on-line hemodiafiltration. All patients who had been dialyzed at our facility for at least 2 months were included in the study, with the only exception of those with missing demographic, bioimpedance or smoking status data. We used pre-dialysis BP’s for comparison of mean arterial BP’s of the cohorts and mid-week values for bioimpedance results. Mean arterial pressure (MAP) was calculated as MAP = 1/3 (SBP – DBP) + DBP.
We used t test to detect significance between the various parameters involving continuous data and we used Chi square test for categorical data. Multivariate regression analysis was also utilized when the associations determining fluid status and blood pressure (mean arterial pressure) were examined. Statistics were calculated using GraphPad 5.04 (San Diego, CA; USA) and figures were graphed using the same. Multivariate regression analysis was calculated by a professional mathematician to predict outcome of multiple categories using IBM SPSS (Armonk, NY; USA). We set the p value for significance to less than .05.
Results
Patients’ demographic data are displayed in . Briefly, the mean ± SD age of the smokers’ cohort was 61.5 ± 15.3 years, 65% male, 38% diabetic, MAP 99.5 ± 16.8 mmHg and Charlson score 3.79 ± 2.04. Of these, 38 patients were nonsmokers and 25 smokers. Blood pressure data and bioimpedance measurements are displayed in . The nonsmokers’ MAP was 94.3 ± 14.0 versus smokers’ 105.9 ± 18.9 mmHg (p: .002); systolic/diastolic pressures 146/68 ± 24/151 for nonsmokers 160/80 ± 15/73 mmHg for smokers (p: .02 for systolic and p: .001 for diastolic values). shows nonsmokers took an average 0.73 ± 0.92 antihypertensive medications vs. 1.73 ± 1.21 for smokers (p: .0001). The distribution of antihypertensive medications taken is skewed toward a higher number among the smokers (2 × 5 chi square p: .004). While 50% of nonsmokers took no antihypertensive medications at all, this rate was only 19% among the smokers. At the same time, only 7.9% (3 of the 38) nonsmokers took 3 antihypertensive medications and none took 4; the smokers’ proportion of taking 3 antihypertensive medication was 30.8% (8 of 25) and one patient was even on 4 antihypertensive medications in this group (). Most importantly, nonsmokers had an average 10.93 ± 7.65 percent overhydration (OH%) by bioimpedance spectroscopy versus smokers’ relative overhydration was 17.63 ± 8.98 percent over the extracellular water space (p: .005) ().
Figure 1. Pre-dialysis mean arterial blood pressure distribution between nonsmoker and smoker patients receiving thrice weekly hemodiafiltration.
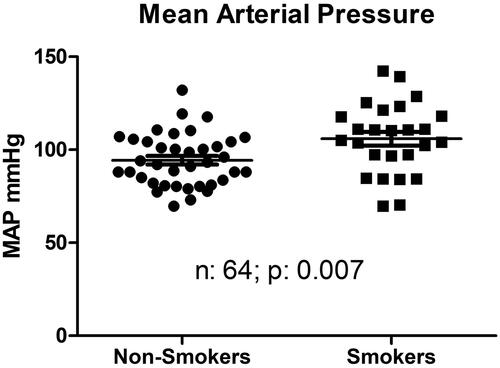
Figure 2. Histogram, depicting the percent distribution of the number of antihypertensive medications taken by nonsmoker and smoker patients receiving hemodialfiltration.
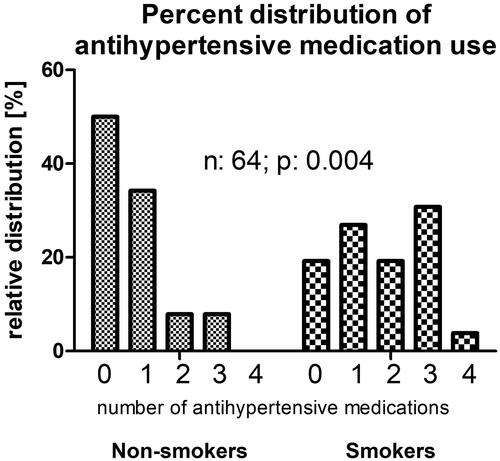
Figure 3. Percent overhydration among nonsmoker and smoker patients (n: 58) receiving hemodiafiltration.
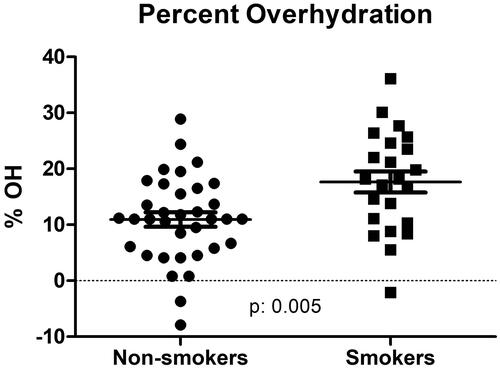
Table 1. Demographics.
Table 2. Results.
also shows that the smokers’ cohort was almost 18 years younger, 80% were male as opposed to 55% male in the nonsmoker group. Furthermore, shows that their relative muscle mass (lean tissue mass) was greater and relative fat mass was smaller. We also performed a multivariate regression analysis for the determinants of percent-overhydration and blood pressure medications. On multivariate regression analysis, smoking emerged as the sole significant factor associated with increased antihypertensive medications use while no other factors including such as age, dialysis vintage, diabetic status, Charlson score of comorbidity, hemoglobin and online-measured (OCM) Kt/V reached statistical significance. The multivariate coefficient was 1.213 to a significant degree (p: .001) for smoking. As shown in , smoking status was the only significant factor predicting overhydration. The multivariate regression coefficient for percent overhydration (OH%) () as a dependent variable was 9.905 and it was statistically significant (p: .001) while all other above-mentioned independent variables’ multivariate coefficients were not statistically significant. For the MAP only age had a statistically significant (<.0001) bearing with a coefficient of −0.605 but not smoking. For absolute lean tissue mass (LTM) smoking had not an influence and for the relative LTM the multivariate coefficient was not significant at 6.076 (p: .087). For the relative LTM% the only significant (p: .035) coefficient was for the diabetic status −7.747. For absolute fat mass the multivariate regression coefficient was of −13.321 (p: .005) and this significance remained present for percent fat mass at −6.506 (p: .02). Though these issues regarding fat and lean tissue mass were not the subject of our investigation, there may be a well-recognized association between smoking and fat mass. shows the ambulatory blood pressure monitoring (ABPM) tracing of a patient who smoked while wearing the monitor thus giving us an accidental opportunity to observe what actually happens to blood pressure while smoking compared to the rest of the time on ABPM.
Figure 4. The author’s own observation on an 8-h ABPM (Ambulatory Blood Pressure Monitoring) revealing an acute blood pressure elevation at 09:30, 13:30 and 16:00, the exact time when the patient indicated that she smoked a cigarettes, Also note, that incidentally a severe white coat effect is also observable as the initial blood systolic pressure is over 200 mmHg yet the sustained blood pressure is around 150 mmHg.
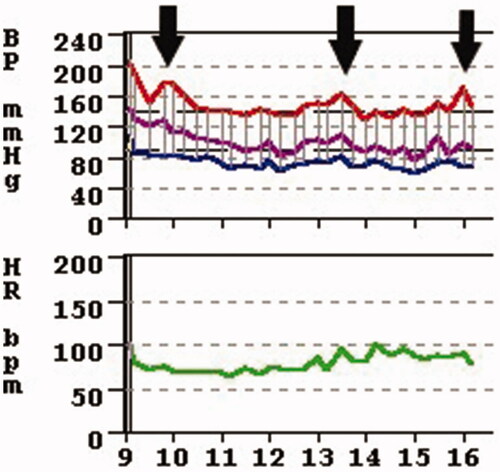
Table 3. Multivariate regression analysis results of a model for pre-dialysis percent overhydration using predictors in the first column.
Discussion
Smoking causes blood pressure elevation by several mechanisms including an impairment of endothelium-dependent vasodilation [Citation5] and endothelial injury [Citation6]. Smoking also causes acute increases in norepinephrine and epinephrine causing acute blood pressure elevation [Citation7] () and an increase of sympathetic outflow [Citation8]. Smoking also alters the vascular shear force and blood rheology thus exacerbating vascular damage [Citation9,Citation10] and a risk factor for chronic kidney disease in animal models [Citation11]. Nicotine containing chewing gums, transdermal patches and IV infusion of nicotine all cause acute blood pressure elevations [Citation10] thus nicotine can be implicated in the smoker dialysis patients’ pre-dialysis blood pressures which we found to be significantly higher than others. While nicotine may be one of the important toxins of cigarette smoking carbon monoxide may be another more important toxin [Citation12], having the greatest concentration at the time of smoking. These studies cited above and also our ABPM tracing of a non-dialysis patient in indicate that this effect of acute blood pressure elevation might be generalizable to both the dialysis and non-dialysis population. The blood pressures tallied for this study were all pre-dialysis BP’s. Furthermore, all patients on dialysis who smoke were interviewed and asked whether they did smoke a cigarette just before entering the dialysis suite’s waiting room and 100% of them gave an affirmative answer. They admitted that they always smoke before their dialysis sessions; again, indicating the possibility that a single cigarette just before dialysis may be sufficient to raise pre-dialysis blood pressure. This may actually partially explain their higher BP as well as why they are on more antihypertensive medications and ultimately more fluid overloaded. Smoking has been a well-established risk factor for congestive heart failure, one manifestation of fluid overload in the non-dialysis, general population [Citation13] as well as in the dialysis population at dialysis initiation due to refractory congestive heart failure [Citation14]. We believe there might be a different mechanism at play in this special, dialysis cohort. Our working theory is that the rounding physicians are more likely to prescribe antihypertensive medications to these more severely hypertensive patients at the beginning of their dialysis sessions. However, we have shown that escalating antihypertensive medications in the dialysis population does not ameliorate blood pressure control [Citation15] this approach may actually contribute to the preservation of hypertensive status. There may be many reasons why this happens but we speculated that antihypertensive medications prevent adequate fluid removal during. We found by bioimpedance measurements that the polypharmatized dialysis patients’ number of antihypertensive medications – including diuretics – had a strong (r: 0.54 p: <.0001) correlation with their fluid overload [Citation16]. Patients with multiple antihypertensive medications run the risk of not tolerating adequate fluid removal even though “avoiding medication-directed control of BP may enhance the opportunity to probe dry-weight, facilitate removal of volume, and limit the risk for pressure-volume overload, which may be a significant concern” [Citation17]. Thus, it seems that pre-dialysis smoking initiates a spiral of acute blood pressure elevation that prompts physicians to prescribe antihypertensive medications that prevent adequate fluid removal during dialysis because of intradialytic hypotension and pharmacological blockade of the physiological response to fluid loss. This may further exacerbate smoker dialysis patients’ hypertension because they will be more fluid overloaded. Others [Citation18] have also found that dialysis patients who smoke have more lung water when measured by lung ultrasound comets, perhaps due to the same mechanism. We examined the possibility that the phenomenon of fluid excess among smokers may simply be the result of the smokers’ demographics, namely that smaller patients, young people and males have been shown [Citation16] to have more fluid overload, however, the multivariate regression model failed to confirm this. Notwithstanding, our finding of fluid overload among smokers is somewhat of a surprise and may need further exploration as to why or by what mechanism do smokers become fluid overloaded more than nonsmokers. We acknowledge that there may be a number of other mechanisms affecting the pre-dialysis blood pressure such as increased thirst, anxiety, apprehension etc., we put forward speculation of a mechanism as above.
While it is admittedly the weakness of the study that the total number of dialysis patients is relatively low, the statistical strength of our findings with p values less well below .01 makes us confident of the validity of the study. This is an observational, retrospective study, not a trial; therefore a cause and effect association could not be stated. We still feel, however, that these observations, namely that smoking may be associated with fluid overload are clinically important findings. We conclude that smoker dialysis patients’ blood pressure may be more volume-related than that of nonsmokers in addition to the other deleterious effects of smoking.
Ethical approval
Research involving Human Participants and/or Animals: This was a non-interventional, retrospective cohort study using existing data and its analysis. No clinical data was solely produced for research purposes. Patients identity was masked and data deidentified; only cumulative data were used. The study was reviewed and approved by the Medical Research Council of Hungary (TUKEB permit number 27677-1/2019/EKU). All patients signed informed consents to use their de-identified cumulative data in clinical studies.
Disclosure statement
MT and MF are current and TF is a former employee of Fresenius Medical Care, Hungary. MT and TF is current employee of the United States Veterans Health Administration. However, the views and opinions expressed herewith do not reflect the official views or opinion or endorsed by the FMC Hungary or the United States Veteran Health Administrations.
Data availability
De-identified data used to support the findings of this study are available from the corresponding author upon request.
References
- Foley RN, Parfrey PS, Sarnak MJ. Epidemiology of cardiovascular disease in chronic renal disease. J Am Soc Nephrol. 1998;9(12 Suppl):S16–S23.
- Liebman SE, Lamontagne SP, Huang LS, et al. Smoking in dialysis patients: a systematic review and meta-analysis of mortality and cardiovascular morbidity. Am J Kidney Dis. 2011;58(2):257–265.
- Staplin N, Haynes R, Herrington WG, et al. Smoking and adverse outcomes in patients with CKD: The Study of Heart and Renal Protection (SHARP). Am J Kidney Dis. 2016;68(3):371–380.
- Cselkó Z, Kovács G, Horváth I. The smoking situation in Hungary. Tob Induc Dis. 2018;16(1):100–100.
- Yugar-Toledo JC, Ferreira-Melo SE, Sabha M, et al. Blood pressure circadian rhythm and endothelial function in heavy smokers: acute effects of transdermal nicotine. J Clin Hypertens (Greenwich). 2005;7(12):721–728.
- Pittilo RM, Bull HA, Gulati S, et al. Nicotine and cigarette smoking: effects on the ultrastructure of aortic endothelium. Int J Exp Pathol. 1990;71(4):573–586.
- Cryer PE, Haymond MW, Santiago JV, et al. Norepinephrine and epinephrine release and adrenergic mediation of smoking-associated hemodynamic and metabolic events. N Engl J Med. 1976;295(11):573–577.
- Narkiewicz K, van de Borne PJ, Hausberg M, et al. Cigarette smoking increases sympathetic outflow in humans. Circulation. 1998;98(6):528–534.
- Powell JT. Vascular damage from smoking: disease mechanisms at the arterial wall. Vasc Med. 1998;3(1):21–28.
- Benowitz NL, Gourlay SG. Cardiovascular toxicity of nicotine: implications for nicotine replacement therapy. J Am Coll Cardiol. 1997;29(7):1422–1431.
- Arany I, Taylor M, Fulop T, et al. Adverse effects of chronic nicotine exposure on the kidney: Potential human health implications of experimental findings. CP. 2018;56(11):501–506.
- Benowitz NL. The role of nicotine in smoking-related cardiovascular disease. Prev Med. 1997;26(4):412–417.
- Suskin N, Sheth T, Negassa A, et al. Relationship of current and past smoking to mortality and morbidity in patients with left ventricular dysfunction. J Am Coll Cardiol. 2001;37(6):1677–1682.
- Fabbian F, Cantelli S, Molino C, et al. Dialysis initiation and survival in patients with refractory congestive heart failure. Int J Artif Organs. 2009;32(8):492–495.
- Tapolyai M, Karim J, Fakhruddin A. Escalating antihypertensive medications in end‐stage renal disease patients does not improve blood pressure control. J Clin Hypertension. 2008;10(3):215–218.
- Tapolyai M, Faludi M, Reti V, et al. Dialysis patients’ fluid overload, antihypertensive medications, and obesity. Asaio J. 2011;57(6):511–515.
- Agarwal R, Weir MR. Dry-weight: a concept revisited in an effort to avoid medication-directed approaches for blood pressure control in hemodialysis patients. CJASN. 2010;5(7):1255–1260.
- Mallamaci F, Benedetto FA, Tripepi R, et al. Detection of pulmonary congestion by chest ultrasound in dialysis patients. JACC Cardiovasc Imaging. 2010;3(6):586–594.
