Since December 2019, there has been an increasing number of unexplained cases of pneumonia in Wuhan, a city with 11 million people in China's Hubei province, which quickly spread to other cities and also abroad. These cases with laboratory confirmed a viral infection have been detected in the world and the World Health Organization (WHO) called this virus as COVID-19 .Given the rapid spread and high mortality rate of COVID-19 with acute kidney injury (AKI), it is absolutely necessary to evaluate the clinical characteristics and possible risk factors affecting the progression of disease in COVID-19 patients with AKI.
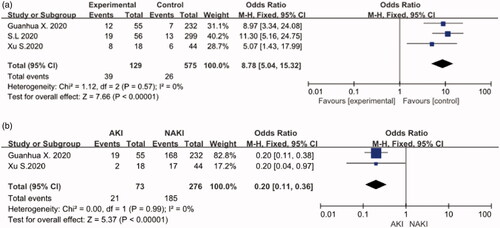
The clinical data of COVID-19 patients from 1 December 2019 to 30 June 2020 were retrieved from databases, including PubMed, Embase, Web of Science, WanFang Data, CNKI, and medrxiv. We statistically analyzed the clinical characteristics, symptoms and examination`s results of COVID-19 patients and explained the clinical features of a meta-analysis. The available data of 789 patients in four publications were included in our meta-analysis [Citation1–4]. The common clinical symptoms of COVID-19 patients with AKI were fever, cough, myalgia or fatigue which is the same as COVID-19 patients with non-AKI (NAKI). But what`s more common than general COVID-19s than the patients with AKI was hypoxia. The results of laboratory results showed that the COVID-19 patients with AKI had higher procalcitonine besides increased lymphocytopenia, C-reactive protein (CRP), lactate dehydrogenase (LDH) and leukocytopenia that represented more inflammation. Meanwhile our meta-analysis found the male with underlying disease like diabetes, chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD), cerebrovascular or cardiovascular disease were more likely to get AKI. As we can see those patients were also more likely to have lower discharge rate and higher fatality rate. The results of the meta-analysis showed that: male (OR:3.43 [1.38, 8.49], p < 0.05), diabetes (OR:2.63 [1.05, 6.58], p < 0.05), COPD (OR: 2.98 [1.27, 6.98], p < 0.05), CKD (OR:3.26 [1.03, 10.32], p < 0.05), cardiovascular disease (OR: 2.26 [1.21, 4.21], p < 0.05), and cerebrovascular disease (OR:2.95 [1.38, 6.32], p < 0.05) were independent risk factors associated with COVID-19 patients with AKI. The meta-analysis revealed no correlation between increased risk of COVID-19 and hypertension, cancer, or chronic liver disease. The discharge rate of COVID-19 patients with AKI was 0.2 [0.11,0.36], p < 0.001 and the fatality rate was 8.78 [5.04,15.32], p < 0.001.
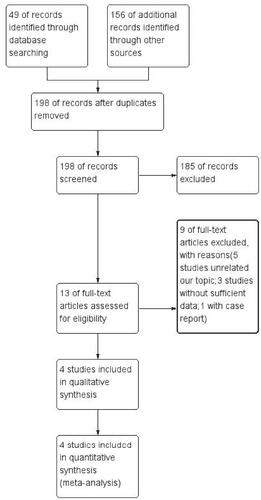
Four studies included in quantitative synthesis (). Data extraction and the evaluation of literature quality were extracted independent (). The MINORS () was used to evaluate bias risk. The Excel was used to analyze the clinical symptoms and examination results. Meta-analysis was performed using Revman5.3.5. When heterogeneity I2 < 50%, a fixed-effects model was chosen, while when I2> 50%, a random-effects model was selected. we consider p < 0.05 as statistical significance (2-sided).
Table 1. Demographics of the included studies.
Table 2. Bias risk assessment.
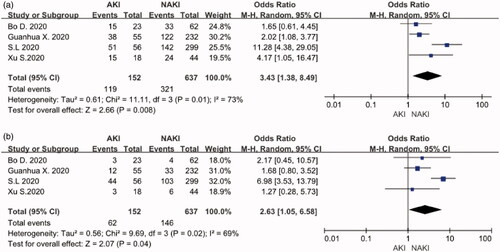
Male and diabetes
Four studies, including 152 COVID-19 patients with AKI and 637 COVID-19 patients with non-AKI (NAKI), provided the data in terms of male and diabetes. The heterogeneity test showed high heterogeneity among these studies, and random-effects model was used for the meta-analysis. The results find that COVID-19 patients with male (OR:3.43, 95%CI [1.38, 8.49], p < 0.05) () and diabetes (OR:2.63, 95%CI [1.05, 6.58], p < 0.05) () had a higher risk of AKI.
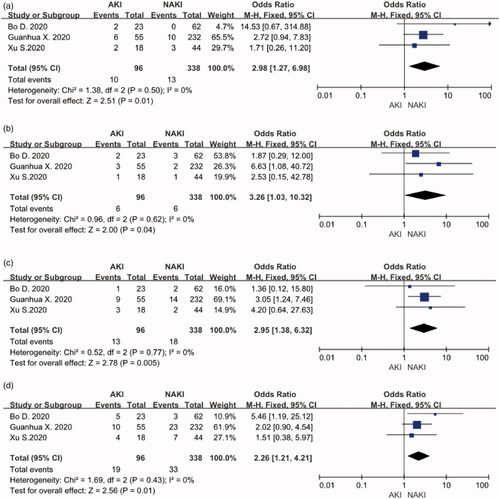
COPD, CKD, cerebrovascular disease and cardiovascular disease
Three included studies reported relationships between COPD, CKD, cardiovascular disease, and COVID-19 patients with AKI. No significant heterogeneity was found (I2 = 0) among these trials, so a fixed effect pattern was chosen. The results showed that these risk factors for patients with COVID-19 and AKI. COPD (OR: 2.98, 95%CI [1.27, 6.98], p < 0.05), CKD (OR:3.26, 95%CI [1.03, 10.32], p < 0.05), cardiovascular disease (OR: 2.26, 95%CI [1.21, 4.21], p < 0.05), and cerebrovascular disease (OR:2.95, 95%CI [1.38, 6.32], p < 0.05) are seen in these meta-analysis respectively. ()).
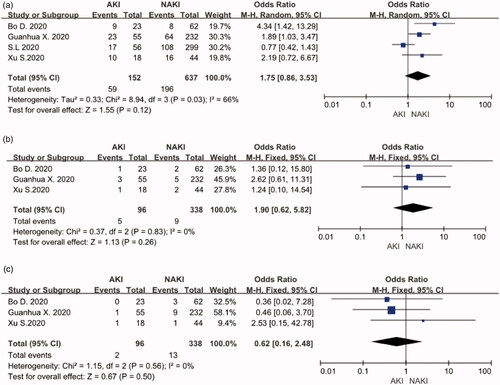
Hypertention, cancer and chronic liver disease
Four studies comprising 152 COVID-19 patients with AKI and 637 COVID-19 patients with NAKI evaluated the role of hypertension in patients with COVID-19 and AKI. The meta-analysis showed that patients with the hypertension did not increase the risk of disease progression (OR:1.75, 95%CI[0.86,3.53], p = 0.12) ().The relative risk assessments associated with cancer and chronic liver disease are presented in . The meta-analysis suggested that there was also no correlation between tumor (OR:1.9, 95%CI[0.62,5.82], p = 0.26) or hepatobiliary disease (OR:0.62, 95%CI[0.16,2.48], p = 0.5) and COVID-19 patients with AKI.
Discharge rate and fatality rate
The three studies showed results of the meta-analysis which revealed the fatality rate of the COVID-19 patients with AKI (OR:8.78, 95%CI [5.04,15.32], p < 0.001). () A fixed effect pattern was chosen because the low heterogeneity I2 = 0. The two studies showed results of the fixed effects model meta-analysis that revealed the discharge rate of the COVID-19 patients with AKI (OR: 0.2,95%CI [0.11,0.36], p < 0.001) () compared with pure COVID-19 patients, COVID-19 and AKI patients do not have much different on the symptoms [Citation5–7]. They all have a fever, cough, dizziness, etc. but according to the data in literature, we do focus hypoxia that is easier to emerge in AKI. It means that we need to give oxygen treatment early. In laboratory tests, we also notice PCT, in which many items represent inflammation, could be a effective diagnosis of COVID-19 and AKI ().
Table 3. Clinic syndrome and therapy.
Table 4. Clinic examination and result.
We made a conclusion that we need pay attention to the degree of hypoxia, inflammatory biomarkers especially PCT of COVID-19 and AKI. And we also should focus on men, diabetes mellitus, COPD, chronic kidney disease (CKD), cardiovascular disease, cerebral blood coronary disease risk factors so that accurate treatment can be made up according to the different condition [Citation8–10]. The meta has some defects: the articles gathered in this literature are all from China, and the size of the sample is not big enough. So the result needs to be further in-depth study.
Disclosure statement
None of the authors have any conflicts of interest related to this study.
References
- Xu S, Hu H, Hu Y, et al. Clinical features of 62 cases of Coronavirus Disease 2019 complicated with acute renal injury. Med J Wuhan Univ. 2020;41(4):537–541.
- Xu S, Fu L, Fei J, et al. Acute kidney injury at early stage as a negative prognostic indicator of patients with COVID-19: a hospital-based retrospective analysis. 2020. DOI:https://doi.org/10.1101/2020.03.24.20042408
- Diao B, Wang C, Wang R, et al. Human kidney is a target for novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. 2020. DOI:https://doi.org/10.1101/2020.03.04.20031120
- Xiao G, Hu H, Wu F, et al. Acute kidney injury in patients hospitalized with COVID-19 in Wuhan, China: a single-center retrospective observational study. 2020. DOI:https://doi.org/10.1101/2020.04.06.20055194
- Li LQ, Huang T, Wang YQ, et al. COVID-19 patients' clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92:577–583.
- Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623.
- Hu L, Chen S, Fu Y, et al. Risk factors associated with clinical outcomes in 323 COVID-19 hospitalized patients in Wuhan, China. Clin Infect Dis. 2020. DOI:https://doi.org/10.1093/cid/ciaa539
- Xu L, Mao Y, Chen G. Risk factors for severe corona virus disease 2019 (COVID-19) patients: a systematic review and meta analysis. 2020. DOI:https://doi.org/10.1101/2020.03.30.20047415
- Cheng Y, Luo R, Wang K, et al. Kidney impairment is associated with in-hospital death of COVID-19 patients. 2020. DOI:https://doi.org/10.1101/2020.02.18.20023242
- Xianghong Y, Renhua S, Dechang C. Diagnosis and treatment of COVID-19: acute kidney injury cannot be ignored. Chinese Med J. 2020;100(16):1205–1208.