Abstract
Introduction
Hip fractures have several adverse effects on patients’ morbidity and mortality. Postoperative Acute kidney injury (AKI) is one of the complications that have a significant impact on the patient’s overall prognosis. We aimed to identify AKI risk after hip fracture surgery and the preoperative and intraoperative risk factors.
Methodology
We conducted a retrospective cohort study in a tertiary care hospital on adult patients who underwent surgery for hip fractures between January 2015 and August 2021. All clinical data were reviewed.
Result
A total of 611 patients were included (age = 76.44 ± 9.69 years). 126 (20.6%) of them developed AKI postoperatively. In multilinear logistic regression analysis, factors associated with postoperative AKI included eGFR [odds ratio (OR): 0.98; 95% confidence interval (CI): 0.97–0.99 with a p value .01], spinal anesthesia [OR: 1.78; 95% CI: 1.1–2.9 with a p value .01], and partial hip replacement (PHR) type of surgery [OR: 0.56; 95% CI: 0.32–0.96 with a p value .036]. The development of postoperative AKI was the strongest factor that increase mortality of the patients as the (HR = 2.42, CI 95% [1.57–3.74]; p value <.001).
Conclusion
In this study, we highlight that lower eGFR, and spinal anesthesia were associated with a higher risk of AKI, and PHR surgery has lower odds to develop AKI. Postoperative AKI is associated with a higher mortality rate after hip fracture surgery.
1. Introduction
Hip fracture incidence is gradually increasing worldwide, with an estimated 4.5 million cases by the end of 2050, compared to the 1.26 million cases in 1990. Furthermore, 18% of females and 6% of males are at risk of sustaining a hip fracture each year [Citation1,Citation2]. Hip fractures have numerous negative effects on patients’ quality of life, according to one study, patients who undergo surgical treatment more than 24 h after a hip fracture have a higher risk of complications and mortality in the following 30 days [Citation3,Citation4]. Therefore, the main goal of treatment is to perform an emergent surgery for those patients to reduce the risk of complications and mortality, which puts them at risk of increased postoperative complications when compared to those who undergo elective surgeries. Common postoperative complications include deep vein thrombosis, pulmonary embolism, acute kidney injury (AKI), and myocardial infarction among others [Citation5]. One of these complications is acute kidney injury, which has a debilitating impact on morbidity and mortality after hip fractures [Citation6]. While tracking the risk factors of postoperative AKI, multiple factors were observed that play a major role in developing AKI, such as gender, and age. The intraoperative course is also critical in these types of surgeries. Furthermore, preoperative factors such as diabetes, hypertension, other comorbidities, and polypharmacy all have a significant impact on the development of AKI in those patients postoperatively [Citation7–10].
Thus, the purpose of our study is to determine the risk of development of AKI postoperatively and to identify preoperative and intraoperative risk factors associated with increased incidence of postoperative AKI in hip fracture patients. Furthermore, gaining a better understanding of the situation will decrease morbidity and mortality rates in future hip fracture surgery.
2. Methodology
2.1. Study design
This retrospective study included 611 patients aged over 18 years who were admitted to Jordan university hospital (JUH), a tertiary medical center in the country, after sustaining hip fractures and surgery. Included patients underwent either intramedullary nailing, dynamic hip screw (DHS) fixation, or hip arthroplasty for a femoral neck, an intertrochanteric, or a subtrochanteric hip fracture.
The patients were identified from the hospital database using the ICD code between January 2015 and August 2021, and patients with end-stage renal disease were excluded from the study which defines as patients who have an eGFR below 15 mL/min/1.73 m2. This study was approved by our Jordan university Institutional Review Board and the inform consent wasn’t required as result of the retrospective approach of the study, and all procedures performed were following the ethical standards of the institutional and/or national research committee and the principles of the World Medical Association Declaration of Helsinki. Informed consent was not required owing to the retrospective nature of the study.
2.2. Patient population and selection criteria
The electronic records were reviewed, and AKI was defined according to the KDIGO criteria and the severity of the AKI has been categorized to either stage 1, 2, or 3 [Citation11]. Serum creatinine was used as a criterion for diagnosing AKI as patients’ urine output was not available in our records. This includes an increase in serum creatinine levels by ≥0.3 mg/dl (≥26.5 μmol/L) within 48 h or an increase in serum creatinine levels by ≥1.5 times of the baseline level within the previous seven days.
2.3. Data collection
2.3.1. Demographics and past medical history
From each patient, the following data were collected (): age, gender, type of fracture, comorbidities (diabetes maleates, hypertension, cardiovascular, neurological disease, and malignancy), estimated GFR (eGFR) using CKD-epi, the last HB1C, and drug history (non-steroidal anti-inflammatory drugs (NSAIDs), angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers and diuretics.
Table 1. Patients characteristics.
2.3.2. Perioperative characteristic
The eGFR before the surgery was noted along with preoperative hemoglobin (HB) level, prophylactic antibiotics, type of anesthesia (general (GA) or spinal anesthesia), type of fracture, and type of surgery.
2.3.3. Postoperative characteristics
Serum creatinine level, post-operative Hb, the incidence of AKI using KIDGO criteria, highest serum creatinine (sCr) level, days of hospital stay, ICU admission, and mortality were documented.
2.4. Statistical analysis
All analyses were carried out using R software. For categorical variables, the comparison was performed using the chi-square test and Fisher’s exact test, whereas continuous variables were performed using the t-test. In addition, the Shapiro-Wilks test was used to determine if variables were normally distributed; for non-normally distributed variables, logarithmic convergence was used for adjustment to a normal distribution. The multivariant logistic regression model was used to assess all potential predictors and to determine the Variable With the predictive value of the development of postoperative AKI development with a p value lower than .05 was determined as a cutoff point to be statistically significant. The final model included age, pre-operative Hb level, pre-operative estimated GFR, type of fracture, type of surgery, and type of anesthesia. Kaplan Meier analysis was used to assess the survival rate by using the survminer R package. Cox regression model was used to assess the effect of variables on the overall survival where the result was presented as a hazard ratio (HR) with a p value lower than.05 determined as a cutoff point to be statistically significant.
3. Results
3.1. Baseline characteristics
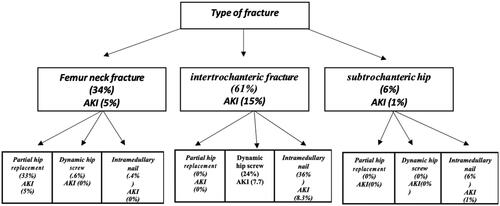
A total number of 611 patients were included in the study. The mean age was 76.44 ± 9.69 years 52.54% were females, regarding the fracture type, 206 (33.71%) had a femur neck fracture (FN), 371 (60.72%) had an intertrochanteric fracture (IT), and 34 (5.56%) had a subtrochanteric fracture (ST). 203 (33.22%) underwent partial hip replacement (PHR), 257 (42.06%) underwent fixation by an intramedullary nail (IMN), and 151 (24.71%) underwent fixation by a dynamic hip screw (DHS) (). 411(67.27%), 301(49.26%), and 212(34.7%) have been previously diagnosed with, hypertension, diabetes mellitus, and cardiovascular diseases, respectively. 418 (68.41%) patients underwent spinal anesthesia, and 187 (30.6%) had CKD preoperatively. The preoperative Hb level was 11.89 ± 2.37 on average whereas the length of hospitalization was 8.19 ± 5.55 and Postoperatively AKI development was reported in 126 (20.62%). the result has shown a significant association was found between the development of postoperative AKI and higher age (p= .012), lower preoperative level of hemoglobin and eGFR (p = .02, .033, respectively), the use of spinal anesthesia (p = .015), IT fracture and DHS surgery (p = .022, .03, respectively).
In terms of blood transfusions, it was observed that 5.57% of the non-AKI group received blood transfusions, while 10.3% of the AKI patients had received blood transfusions. However, this difference was not statistically significant, with a p value of .9. Similarly, the use of vasopressors was reported in 2.29% of patients, but it was not found to be associated with the development of AKI following surgery. Specifically, 3.97% of the AKI group had received vasopressors, while only 1.86% of the non-AKI group had received it, and the difference was not statistically significant with a p value of .319. See for more details.
Based on the staging of the AKI patients, 104 (83.5%) patients were classified as Stage 1, 18 (14.3%) patients as Stage 2, and 4 (3.2%) patients as Stage 3. We found significant differences between AKI stages and mortality and ICU admission with a p value of .01 and .003, respectively. For further details, see Table 1S.
Our data also showed that patients who underwent intramedullary nailing (IMN) were more likely to have general anesthesia compared to spinal anesthesia 46.6% and 40.0% respectively with a p value .008. for further details, see Table 2S.
3.2. AKI risk factors
The result of the multivariate logistic analysis showed that spinal anesthesia, preoperative eGFR, and PHR type of surgery were significant predictors for the development of postoperative AKI (OR = 1.78, 0.988, and 0.56; CI 95% [1.11–2.87, 0.97–0.99, and 0.32–0.96]; p value = .016, .015, and .036, respectively), whereas age, preoperative hemoglobin level, types of fracture or surgery was predictable of the development of the age as shown in . The logistic regression model has established accuracy of 79.44, sensitivity of 0.79, and precision of 100.00.
Table 2. Factors affecting the development of postoperative AKI.
3.3. Development of postoperative AKI
The development of postoperative AKI was associated with a higher rate of ICU admission, longer hospitalization, and death, (OR = 2.07, [CI95%=1.37–3.15]; p value < .001), (OR = 1.09, [CI95%=1.05–1.13]; p value < .001), and (OR = 3.27, [CI95%=2.01–5.32]; p value<.001) (), respectively.
Table 3. Result of development postoperative AKI.
3.4. Survival analysis
The overall cumulative survival after 180-days follow-up was (86%, CI 95% [0.83–0.89]). The following parameters: age (HR =1.04, CI95% [1.01–1.07]; p value = .003), male gender (HR = 1.79, CI 95% [1.12–2.69]; p value = .013), preoperative hemoglobin level (HR = 0.83, CI 95% [0.74–0.93]; p value <.001), eGFR (HR= 0.9879, CI95%[0.98–0.9976]; p value=.015] and AKI (HR =2.42, CI 95% [1.57–3.74]; p value <.001), were shown to have a significant effect survival on multivariate COX regression ().
Table 4. Factors affecting the mortality postoperatively.
During 180 days of follow-up, the overall cumulative survival was 72.2% in patients who developed AKI post-operatively, whereas the overall cumulative survival in the patients who didn’t develop AKI post-operatively was 89.5% log-rank test between the two groups (p < .001). The detailed survival analysis is shown in and presented in the Kaplan–Meier analysis curve ().
Figure 2. Kaplan Meier curve; AKIPostOP: acute kidney injury postoperatively; N: no; Y: yes; the red line represent the survival of the patients who didn’t develop postoperative AKI; the blue one represent the survival of the patients who developed postoperative AKI.
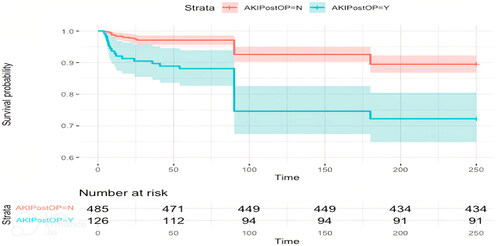
Table 5. Survival table.
4. Discussion
In our study, the mean age of the sample is (76.44 years) which is younger than previous studies that have looked at the risk factors for the development of postoperative AKI as the mean age was ranging between 77 and 85 years [Citation12–14]. Previous studies have reported that the incidence of AKI in high-energy trauma patients ranged from 15 to 40% [Citation15–17]. Whereas according to a few numbers of studies, the incidence of AKI in hip fracture patients was 15–24% [Citation12–15], which is consistent with our result of AKI incidence of 20.6%. A newer study has reported a lower incidence of AKI in those patients (8.4%) [Citation6]. This difference in the results might be related to the variations in the standard of care among hospitals, as well as the heterogeneity of the included patient population in some studies. On the other hand, in our study, there was homogeneity in race, treatment type, and preoperative and postoperative care.
Numerous studies have evaluated the possible factors that could predict the development of AKI following surgeries, including male gender, vascular disease, hypertension, diabetes, body mass index (BMI), chronic obstructive pulmonary disease, congestive heart failure, chronic kidney disease, and pre-morbid use of nephrotoxic drugs [Citation18–20]. However, our research is underscored by the fact that our study population hails from low- to middle-income countries (LMICs), where prior research has shown that patient outcomes differ significantly from those in high-income countries (HICs) for several different factors [Citation21]. Although the risk of developing AKI after hip and knee replacement surgeries has been studied on several occasions in prior research, it’s important to note that these studies have been conducted in HICs [Citation22]. This meta-analysis of more than 72,000 patients, however, describes AKI in patients undergoing elective knee and hip surgeries, patients with hip fractures are a much more fragile group of patients. Also applying the results of these studies to different populations may raise concerns due to disparities in the incidence rates of non-communicable diseases such as diabetes, hypertension, and cardiovascular disease between HICs and LMICs, as supported by various studies.
For instance, a study conducted by Lam and his colleagues found that the prevalence of diabetes complications was significantly higher in LMICs, but limited availability of cohort studies from these countries hindered their ability to establish associations between diabetes and specific comorbidities [Citation23]. Similarly, another study by Schutte and his colleagues observed a significant increase in blood pressure levels in LMICs, which could contribute to the development of postoperative complications, including AKI [Citation24].
Furthermore, AKI has been recognized as a significant factor contributing to morbidity and mortality in LMICs, and the lack of data from these countries poses challenges in estimating the prevalence of the disease in these regions [Citation25,Citation26]. This discrepancy may be attributed to differences in healthcare infrastructure, availability of resources such as dialysis facilities and medications, lack of awareness regarding AKI, and limited access to specialized care for AKI management in LMICs compared to HICs [Citation26].
These findings underscore the impact of healthcare infrastructure, resources, and access to specialized care on the development and outcomes of AKI in different income settings. The resulting strain on the healthcare system in LMICs, due to increased hospital days and ICU admissions for AKI patients after surgery, emphasizes the need to identify factors that influence patient outcomes in LMICs. This knowledge is crucial for improving patient management and outcomes in these regions, alleviating pressure on the healthcare system, and enhancing overall patient care in LMICs.
In our study, age, pre-and post-operative hemoglobin levels, type of surgery, type of anesthesia, and pre-and post-operative estimated GFR, were significantly associated with a higher incidence of AKI, whereas after multiple logistic regression analysis, only lower preoperative eGFR and spinal anesthesia were predictors for the development of AKI post hip fracture surgeries, which is in contrast to previous studies in the literature suggesting that general anesthesia is more associated with the development of post-operative AKI compared to spinal anesthesia [Citation27]. This indicates an associated higher risk with certain surgeries, such as DHS, as presented in our study, as well as spinal anesthesia, which could be a result of hypotension during the procedure [Citation28]. On the other hand, there was no statistical difference in the incidence of AKI between the two genders and DM as reported in other studies [Citation12,Citation13], which might be explained by the difference in the population background and different levels of activity between the two genders, as well as the difference in the level of DM control. The six-month follow-up period in this study revealed a higher survival rate in patients who did not develop AKI postoperatively. This finding is supported by other studies, as AKI is one of the most common complications with a significant impact on a patient’s prognosis [Citation29–31]. According to various studies, mortality after hip fracture surgeries is highest in the first few months, with the greatest increase in mortality occurring in the first three months. The survival rate for patients who developed AKI postoperatively ranged between 43 and 86.5%, while for patients who did not develop AKI postoperatively the survival rate ranged between 94.2 and 97.7% [Citation12,Citation13,Citation32]. In our study, the development of AKI is one of the factors that could predict the postoperative survival rate. The six-month survival in our patient cohort was shown to be higher compared to other studies, 74.5% compared to 65% at three months, the difference between the two results might be related to the difference in the age between the two samples as our sample have younger age (76.44) compared to (81) year [Citation6]. The highest drop in the survival rate was recorded three months after the surgery which has also been reported by other studies as well [Citation33–35]. Cement is not known to be linked directly with kidney injury; the incidence of bone cement syndrome is significantly rare [Citation36].
Limitations of this study: first, it is retrospective, single-center study, the unavailability of the preoperative and postoperative urine output and volume status, and the inability to assess fluid management strategies appropriately secondary to deficient data. Second, the sample size in this study may affect the ability to generate accurate conclusions. Hence, a larger dataset is necessary to draw proper conclusions. Third, Due to some challenges in data collection, we were not able to evaluate all aspects of intra and postoperative complications and interventions such as infections and intraoperative blood loss among others. However, we acknowledge the importance of investigating these factors in future research, given their potential impact on postoperative outcomes, and the need for a larger number of patients for more accurate results. Finally: this study did not investigate the precise mechanism of the development of AKI post operatively.
The strengths of this study include that it is large and first retrospective cohort studies examining the preoperative and postoperative risk factors for developing acute kidney injury in patients undergoing hip fracture surgery in LMICs in way to improve the management of those patients in these areas. Additionally, our use and analysis of a variety of pre-and postoperative factors, and that only a few data were missing during patients’ hospital stay.
5. Conclusion
In conclusion, the incidence of developing AKI postoperatively in hip fracture patients was 20.6%. Postoperative AKI was associated with an increase in mortality rates. Estimated GFR and anesthesia type predicted the development of postoperative AKI. Further studies could elucidate more on the prevention and treatment of postoperative AKI in order to decrease complications and mortality rates in this fragile subset of patients.
Ethical approval
University of Jordan Hospital local institutional review boards reviewed the study and determined that the study met the criteria for exempt status and the requirement for informed consent was waived.
Supplemental Material
Download PDF (92.1 KB)Supplemental Material
Download PDF (97.6 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Cooper C, Campion G, Melton L. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2(6):1–7. doi: 10.1007/BF01623184
- Cooper C, Cole Z, Holroyd C, et al. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011;22(5):1277–1288. doi: 10.1007/s00198-011-1601-6
- Peeters C, Visser E, Van de Ree C, et al. Quality of life after hip fracture in the elderly: a systematic literature review. Injury. 2016;47(7):1369–1382. doi: 10.1016/j.injury.2016.04.018
- Pincus D, Ravi B, Wasserstein D, et al. Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA. 2017;318(20):1994. doi: 10.1001/jama.2017.17606
- Fields AC, Dieterich JD, Buterbaugh K, et al. Short-term complications in hip fracture surgery using spinal versus general anaesthesia. Injury. 2015;46(4):719–723. doi: 10.1016/j.injury.2015.02.002
- Rantalaiho I, Gunn J, Kukkonen J, et al. Acute kidney injury following hip fracture. Injury. 2019;50(12):2268–2271. doi: 10.1016/j.injury.2019.10.008
- Wang Y, Bellomo R. Cardiac surgery-associated acute kidney injury: risk factors, pathophysiology and treatment. Nat Rev Nephrol. 2017;13(11):697–711. doi: 10.1038/nrneph.2017.119
- Yuan SM. Acute kidney injury after cardiac surgery: risk factors and novel biomarkers. Braz J Cardiovasc Surg. 2019;34(3):352–360. doi: 10.21470/1678-9741-2018-0212
- Chen J, Kuo G, Hung C, et al. Risk factors and prognosis assessment for acute kidney injury: the 2020 consensus of the Taiwan AKI task force. J Formosan Med Assoc. 2021;120(7):1424–1433. doi: 10.1016/j.jfma.2021.02.013
- Yasin M, Farah R, Hammad Y, et al. Determining the risk of acute kidney injury in patients who underwent total joint replacement: a retrospective study. J Orthop Sci. 2020;25(6):1029–1034. doi: 10.1016/j.jos.2019.12.007
- Khwaja A. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:S1–S138. doi: 10.1159/000339789
- Bennet SJ, Berry OMB, Goddard J, et al. Acute renal dysfunction following hip fracture. Injury. 2010;41(4):335–338. doi: 10.1016/j.injury.2009.07.009
- Ulucay C, Eren Z, Kaspar EC, et al. Risk factors for acute kidney injury after hip fracture surgery in the elderly individuals. Geriatr Orthop Surg Rehabil. 2012;3(4):150–156. doi: 10.1177/2151458512473827
- Azevedo VLF, Silveira MAS, Santos JN, et al. Post-operative renal function evaluation, through rifle criteria, of elderly patients who underwent femur fracture surgery under spinal anesthesia. Ren Fail. 2008;30(5):485–490. doi: 10.1080/08860220802060398
- Skinner DL, Hardcastle TC, Rodseth RN, et al. The incidence and outcomes of acute kidney injury amongst patients admitted to a level i trauma unit. Injury. 2014;45(1):259–264. doi: 10.1016/j.injury.2013.07.013
- Eriksson M, Brattstrom O, Martensson J, et al. Acute kidney in- jury following severe trauma: risk factors and long-term outcome. J Trauma Acute Care Surg. 2015;79(3):407–412. doi: 10.1097/TA.0000000000000727
- Bihorac A, Delano MJ, Schold JD, et al. Incidence, clinical predictors, genomics, and outcome of acute kidney injury among trauma patients. Ann Surg. 2010;252(1):158–165. doi: 10.1097/SLA.0b013e3181deb6bc
- Abelha FJ, Botelho M, Fernandes V, et al. Determinants of postoperative acute kidney injury. Crit Care. 2009;13(3):R79. doi: 10.1186/cc7894
- Noor S, Usmani A. Postoperative renal failure. Clin Geriatr Med. 2008;24(4):721–729, ix. doi: 10.1016/j.cger.2008.07.004
- Rahmanian PB, Kwiecien G, Langebartels G, et al. Logistic risk model predicting postoperative renal failure requiring dialysis in cardiac surgery patients. Eur J Cardiothorac Surg. 2011;40(3):701–707. doi: 10.1016/j.ejcts.2010.12.051
- James MT, Bhatt M, Pannu N, et al. Long-term outcomes of acute kidney injury and strategies for improved care. Nat Rev Nephrol. 2020; 16(4):193–205. doi: 10.1038/s41581-019-0247-z
- Filippone EJ, Yadav A. Acute kidney injury after hip or knee replacement: can we lower the risk? Cleve Clin J Med. 2019;86(4):263–276. doi: 10.3949/ccjm.86a.18044
- Lam A, Lepe A, Wild S, et al. Diabetes comorbidities in low- and middle-income countries: an umbrella review. J Glob Health. 2021;11:04040. doi: 10.7189/jogh.11.04040
- Schutte AE, Srinivasapura Venkateshmurthy N, Mohan S, et al. Hypertension in low- and middle-income countries. Circ Res. 2021;128(7):808–826. doi: 10.1161/circresaha.120.318729
- Rewa O, Bagshaw SM. Acute kidney injury—epidemiology, outcomes and economics. Nat Rev Nephrol. 2014;10(4):193–207. doi: 10.1038/nrneph.2013.282
- Li PK, Burdmann EA, Mehta RL. Acute kidney injury: global health alert. Kidney Int. 2013;83(3):372–376. doi: 10.1038/ki.2012.427
- Kim H-J, Park H-S, Go Y-J, et al. Effect of anesthetic technique on the occurrence of acute kidney injury after total knee arthroplasty. JCM. 2019;8(6):778. doi: 10.3390/jcm8060778
- Bell S, Dekker FW, Vadiveloo T, et al. Risk of postoperative acute kidney injury in patients undergoing orthopedic surgery-development and validation of a risk score and effect of acute kidney injury on survival: observational cohort study. BMJ. 2015;351(v11 19):h5639. doi: 10.1136/bmj.h5639
- Mathis M, Naik B, Freundlich R, et al. Preoperative risk and the association between hypotension and postoperative acute kidney injury. Anesthesiology. 2020;132(3):461–475. doi: 10.1097/ALN.0000000000003063
- Gaieski DF, Edwards JM, Kallan MJ, et al. Benchmarking the incidence and mortality of severe sepsis in the United States. Crit Care Med. 2013;41(5):1167–1174. doi: 10.1097/CCM.0b013e31827c09f8.
- Wohlauer MV, Sauaia A, Moore EE, et al. Acute kidney injury and posttrauma multiple organ failure: the canary in the coal mine. J Trauma Acute Care Surg. 2012;72(2):373–380. doi: 10.1097/TA.0b013e318244869b
- Uchino S, Kellum JA, Bellomo R, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294(7):813–818. doi: 10.1001/jama.294.7.813
- Brandt MM, Falvo AJ, Rubinfeld IS, et al. Renal dysfunction in trauma: even a little costs a lot. J Trauma. 2007;62(6):1362–1364. doi: 10.1097/TA.0b013e318047983d
- Haentjens P, Magaziner J, Colón-Emeric CS, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152(6):380. doi: 10.1059/0003-4819-152-6-201003160-00008.Meta-analysis
- von Friesendorff M, McGuigan FE, Wizert A, et al. Hip fracture, mortality risk, and cause of death over two decades. Osteoporos Int. 2016;27(10):2945–2953. doi: 10.1007/s00198-016-3616-5
- Mudgalkar N, Ramesh KV. Bone cement implantation syndrome: a rare catastrophe. Anesth Essays Res. 2011;5(2):240. doi: 10.4103/0259-1162.94796