Abstract
Objective
To explore the correlation between neutrophil-to-lymphocyte ratio (NLR) and contrast-induced acute kidney injury (CI-AKI). To develop machine-learning (ML) methods based on NLR and other relevant high-risk factors to establish new and effective predictive models of CI-AKI. Methods: The data of 2230 patients, who underwent elective vascular intervention, coronary angiography and percutaneous coronary intervention were retrospectively collected. The patients were divided into a CI-AKI group and a non-CI-AKI group. Logistic regression was used to analyze the correlation of NLR with CI-AKI and high-risk factors for CI-AKI, and logistic regression (LR), random forest (RF), gradient boosting decision tree (GBDT), extreme gradient boosting (XGBoost), and naïve Bayes (NB) models based on NLR and the high-risk factors were established.
Results
A high NLR(>2.844) was an independent risk factor for CI-AKI (odds ratio = 2.304, p < 0.001). The area under the ROC curve (AUC) of the NB model was the largest (0.774), indicating that it had the best performance. NLR, serum creatinine concentration, fasting plasma glucose concentration, and use of β-blocker all accounted for a large proportion of the predictive performance of each model and were the four most important factors affecting the occurrence of CI-AKI.
Conclusions
There was a significant correlation between NLR and CI-AKI The NB model exhibited the best predictive performance out of the five ML models based on NLR exhibited the best predictive performance out of the five ML models.
Introduction
The increasing use of contrast medium (CM) during imaging has led to a concomitant increase in the incidence of contrast-induced acute kidney injury (CI-AKI), which is now the third most common cause of iatrogenic acute kidney injury (AKI) [Citation1]. CI-AKI can cause cells to undergo necrosis or apoptosis, resulting in oxidative stress and thus an inflammatory response. Neutrophil-to-lymphocyte ratio (NLR) is an indicator of oxidative stress-related inflammation and plays a key role in the development and progression of AKI. In particular, NLR is predictive of a high risk of sepsis-induced AKI [Citation2] and the development of AKI after cardiovascular interventions and surgery [Citation3]. Recently, NLR also proved to be a predictive marker of CI-AKI in a relatively small cohort of patients with acute coronary syndrome and myocardial infarction undergoing emergency PCI [Citation4–6]. While the predictive value is not clear when undergoing elective angiography. Moreover, the mechanism of CI-AKI is conplex. Combination of more valuable indictators may improve the predictive efficiency in clinical practice.
Machine learning (ML) is gaining increasing attention in medical biology, and some ML methods (e.g., random forests) are more accurate than traditional logistic regression models in predicting disease occurrence [Citation7,Citation8]. It can handle complex relationships between a number of variables in real-world big data. The predictive performance of ML models has been demonstrated superior to that of traditional statistical models for predicting AKI.
In this study, we aimed to retrospectively collect data from patients who had undergone elective vascular intervention, coronary angiography (CAG), and percutaneous coronary intervention (PCI) and analyze the correlation between NLR and the occurrence of CI-AKI in these patients. We also aimed to use ML methods to incorporate NLR data with other relevant high-risk factors to establish a novel preoperative CI-AKI risk-prediction model that provides early warning of patients at a high risk of developing CI-AKI, so that improved patient outcomes could be achieved.
Materials and methods
Study subjects
Patients who underwent elective CAG and PCI at the Department of Cardiology and elective vascular interventional surgery at the Department of Vascular Surgery, Ningbo NO.2 Hospital, Ningbo, China, from 1 January 2016 to 31 December 2020. Inclusion criteria: (1) age ≥ 18 years; and (2) a serum creatine (Scr) concentration test performed within 48 h of admission. Exclusion criteria: (1) had emergency surgery; (2) had an allergy to CM; (3) had been pregnant or lactating; (4) had end-stage renal disease, had received a renal transplant, or had received renal replacement therapy; (5) missing more than 30% of variables or missing a postoperative Scr concentration result (which precluded end-point event adjudication); or (6) had multiple tumors or a life expectancy of less than 1 year.
Patient informed consent was waived due to the retrospective study design. The study design was approved by the Medical Ethics Committee of Ningbo NO.2 Hospital (NBEY-2020-096-01) and adhered to the Declaration of Helsinki.
Data collection
The baseline data and clinical data of the enrolled patients were collected, comprising sex, age, body mass index (BMI), blood pressure, heart rate, chronic diseases history, the drugs before CM used. The routine laboratory measurements were also collected including NLR, hemoglobin (Hb) concentration, albumin (ALB) concentration, fasting plasma glucose (FPG) concentration, Scr concentration, blood urea nitrogen (BUN) concentration, estimated glomerular filtration rate (GFR), total cholesterol (TC) concentration, etc. All baseline laboratory tests were measured upon admission before the CAG, PCI, or vascular surgery. The postoperative Scr level was measured within 1 week after CAG, PCI, or vascular surgery and evaluated for determining the occurrence of CI-AKI.
The diagnostic criteria and staging of CI-AKI were referred to kidney disease: improving global Prognosis As defined by outcomes, KDIGO [Citation9], an increase in Scr ≥26.5 μmol/L within 48 h of CM administration) or ≥1.5 times the baseline value. (Baseline Scr: Scr within 48 h of admission.)
Statistical methods
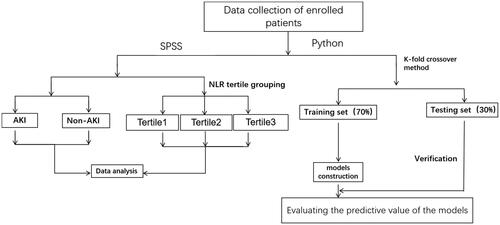
Normally distributed continuous variables are expressed as means ± standard deviations (SD), whereas non-normally distributed continuous variables are expressed as medians and quartiles (25%, 75%). Categorical variables are presented as absolute values and percentages. A t-test or Mann–Whitney U test was used to analyze continuous variables, and a chi-square test was used to analyze categorical variables. Linear trend analysis was used to evaluate the correlation between NLRs and CI-AKI risk, and the sample was then divided into tertiles according to NLR values. Logistic regression was used to analyze the association between CI-AKI and NLR. Python 3.7.6 and SPSS 23.0 software were used to perform statistical analyses. p < 0.05 was considered to indicate a statistically significant difference. A flowchart of the statistical process of this study is shown in .
Construction of ML predictive models
Five predictive models were constructed using the sample data and based on logistic regression (LR), random forest (RF), gradient boosting decision tree (GBDT), extreme gradient boosting (XGBoost), and naive Bayes (NB) ML techniques, respectively.
LR is a powerful and mature supervised classification method, the most common model for analyzing the relationship between dependent variables and one or more explanatory variables, with the advantage that it has a long-standing, easy-to-understand theoretical and computational background and can only model dichotomy variables that typically represent the occurrence or nonoccurrence of events.
Random forest (RF) is an ensemble of decision trees based on the bagging and random subspace concepts. It overcomes the primary drawback of decision trees (i.e., overfitting on the training data set) to gain better predictive results.
Gradient boosting decision tree (GBDT) is an algorithm based on boosting that integrates multiple decision trees in series and trains and learns. The core algorithm idea is based on residual learning, through multiple (low variance and high deviation) individual models. The learning method of superimposing and summing to reduce the overall deviation.
Extreme gradient boosting (XGBoost) is a tree ensemble technique based on the loss generated by weak decision tree-based learners. XGBoost was trained as the baseline model, followed by the training of the final model with optimized hyperparameters.
Naive Bayes (NB) is based on the Bayes theorem, which states that one feature’s presence is completely independent of another feature’s presence. NB proves well in multi-class predictions. It also responds better than other models when assuming autonomy holds, such as logistical regression, and less training data are required. Furthermore, it can also work easily with missing values.
Data on early-warning parameters were collected from the sample. The sample was split into a training set (70%) and a test set (30%). The synthetic minority oversampling technique (SMOTE) was used only on the training data to eliminate the imbalanced distribution of data [Citation10]. We used the RandomGridSearch to search for hyperparameters on the training set to find the best hyperparameters, and then predicted on the training set to get the predicted results. Each model has been divided into data sets for 100 times, and different random number seeds were used to train the model for each data set. To improve the accuracy of the model, we chose the one with the best performance (the highest AUC) in the training set after hyperparameter optimization.
The categorical feature inputs were extracted from sample data and used to build the ML predictive models, which were trained using fivefold cross-validation. The accuracy of the five predictive models in the prediction of CI-AKI was compared using evaluation indexes, such as accuracy, recall, area under the receiver operating characteristic (ROC) curve (AUC), etc. Using SHapley Additive exPlanations (SHAP) values, we characterized the crucial characteristics that affect mortality risk in the best ML model to study further each characteristic’s significance to the optimal model’s output.
Results
Baseline characteristics
The baseline statistical analysis was performed using data on 2230 patients. The incidence of CI-AKI was 5.38%, as there were 120 patients in the CI-AKI group, 96 patients with AKI stage 1, 18 patients with AKI stage 2, 6 patients with AKI stage 3, and 2110 patients in the non-CI-AKI group, including 671 women (30.10%). The average day to AKI onset was (2.16 ± 0.89) days. The CI-AKI group had a higher NLR [3.38 (2.60, 5.35) vs 2.79 (1.98, 4.18), p < 0.001], was older, had a larger proportion of women, had a larger proportion of patients with hypertension, and had a larger proportion of patients with diabetes mellitus (DM), atrial fibrillation (AF), coronary artery disease (CAD), heart failure (HF), or chronic kidney disease (CKD), compared with the non-CI-AKI group (all p < 0.05). Regarding the use of medications, compared with the non-CI-AKI group, the CI-AKI group exhibited more use of loop diuretics, spironolactone, angiotensin receptor blockers (ARBs), warfarin, low-molecular-weight heparin (LMWH), β-blockers, biguanides, and insulin (all p < 0.05). Compared with the non-CI-AKI group, the CI-AKI group had a significantly lower Hb concentration and GFR, higher ALB and FPG concentrations, higher serum Scr and BUN concentrations, and a higher proportion of patients with positive proteinuria and the presence of a carotid plaque (all p < 0.05). Details of these data are shown in .
Table 1. Baseline characteristics of study subjects.
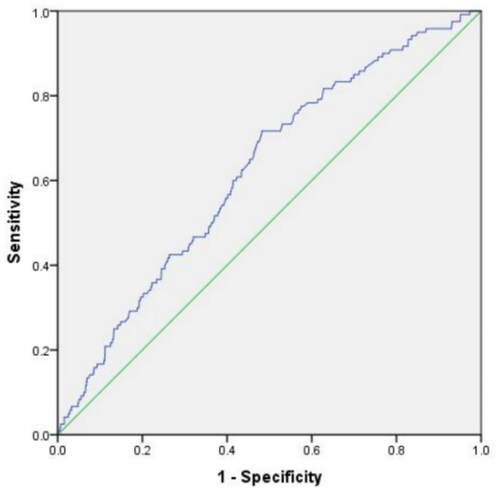
The AUC of CI-AKI predicted by NLR was 0.623 (95%CI: 0.574-0.671) (), and the sensitivity was 71.7%. the specificity was 51.8% and the critical value was 2.844
Logistic regression
Univariable logistic analysis showed that older age, female, increased systolic blood pressure (SBP), the presence of hypertension, DM, AF, CAD, HF, and CKD), the use of ARBs, loop diuretics, spironolactone, biguanides, insulin), warfarin, and LMWH, proteinuria, the presence of a carotid plaque, increased FBG concentration, Scr concentration, and NLR were risk factors for CI-AKI (all p < 0.05), whereas the use of β-blockers, increased Hb concentration, and eGFR were protective factors for CI-AKI (all p < 0.05). Details of this analysis are shown in .
Table 2. Univariable logistic regression analysis of factors associated with CI-AKI.
The above-mentioned indicators that were statistically significant in the univariable analysis logistic analysis were used as covariates in a multivariable logistic analysis (forward). The results showed that increased NLR(>2.844) and SBP, female, the presence of CKD, the use of ARBs, spironolactone, and LMWH were high-risk factors for the development of CI-AKI (all p < 0.05), whereas increased eGFR and Hb concentration was the independent protective factor for CI-AKI (all p < 0.05). Details of this analysis are shown in .
Table 3. Multivariable logistic regression analysis of CI-AKI.
Correlation between NLR and CI-AKI
The patients were next grouped into tertiles according to their NLR. NLR was significantly higher in the tertile 2 patients than in the tertile 1 patients [2.82 (2.54, 3.15) vs 1.69 (1.43, 2.00), p < 0.001] and significantly higher in the tertile 3 patients than in the tertile 1 patients [5.00 (4.25, 6.81) vs 1.69 (1.43, 2.00), p < 0.001]. NLR was also significantly higher in the tertile 3 patients than in the tertile 2 patients [2.82 (2.54, 3.15) vs 5.00 (4.25, 6.81), p < 0.001]. We also compared the tertiles’ baseline clinical data (shown in Supplementary Table 1) and found that they differed significantly (p < 0.05) in terms of age, gender, BMI, heart rate, comorbidities (hypertension, DM, AF, CAD, HF, stroke, and coronary obstructive pulmonary disease), smoking, medication use (loop diuretics, antibiotics, ARBs, β-blockers, spironolactone, and insulin), and biochemical data (Hb concentration, ALB concentration, FPG concentration, TC concentration, Scr concentration, BUN concentration, GFR, and proteinuria). An analysis of the results also showed that the percentage risk of developing CI-AKI gradually increased from tertile 1 to tertile 2 to tertile 3 (2.69% vs 5.95% vs 7.51%, p = 0.046 for trend).
ML Models
The best performance of five ML models for the prediction of CI-AKI were shown in .
Table 4. The best performance of five ML models for the prediction of CI-AKI.
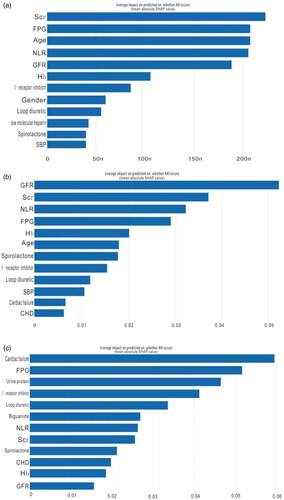
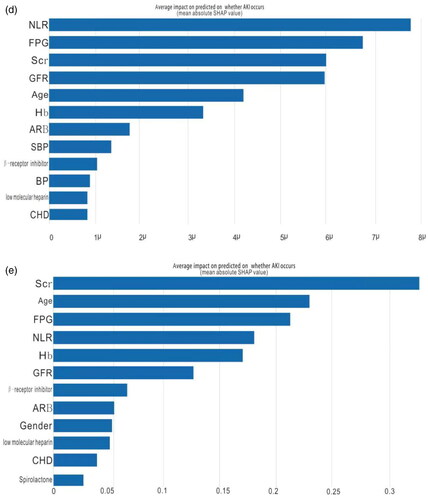
The results of the five ML models that were trained to diagnose CI-AKI showed that the highest AUC was obtained by the NB model, followed by (in order of decreasing AUC) the GDBT model, the LR model, RFt model, and the XGBoost model. All of the models exhibited well-validated performance, as shown by their AUCs (). Individual feature variable importance was calculated using the five models, ranked based on the importance of the SHAP values, and the results are given in (which shows the 12 most important feature variables). The results indicate that NLR, Scr concentration, FPG concentration, and β-blocker use were the four factors that played the most significant roles in the ML models. The other significant factors in the ML models were age, GFR, Hb concentration, gender, HF, and other indicators.
Figure 3. Receiver operator characteristic curves(ROC) of the validation sets for the (a) GBDT model, (b) XGBoost model, (c) LR model, (d) RF model, and (e) NB model.
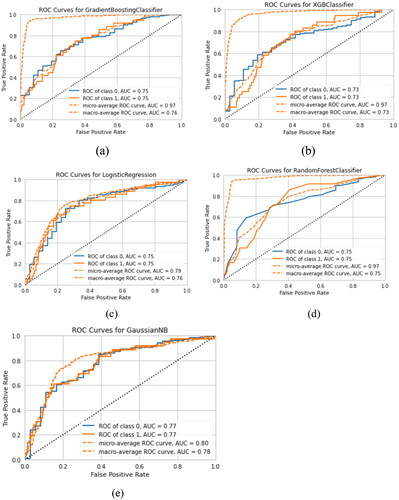
Figure 4. Variable importance distributions for the (a) GBDT model, (b) RF model, (c) NB model, (d) XGBoost model, and (e) LR model. Scr: serum creatinine; FPG: fasting plasma glucose; NLR: neutrophil-to-lymphocyte ratio; GFR: glomerular filtration rate; Hb: hemoglobin; SBP: systolic blood pressure; CHD: chronic heart disease; ARB: angiotensin receptor blocker;
Discussion
CM-induced renal injury is one of the major causes of AKI and is denoted CI-AKI. It is important to identify risk factors to enable the prediction of CI-AKI, as this could assist with the prevention and treatment of CI-AKI and improve the prognosis of patients. In our retrospective study analyzed a relatively large population of patients who received contrast medium, and confirmed NLR was an independent predictor of CI-AKI. Additionally, among the five ML models that were constructed, NB was the best model, with relatively good discriminative ability. Inflammation appears to play an important role in the pathogenesis of CI-AKI, and NLR is a relatively stable inflammatory marker that can be used to predict the occurrence of AKI [Citation11]. A study of patients undergoing coronary artery bypass graft found that those in the CI-AKI group had higher NLRs than those in the non-CI-AKI group [2.63 (1.83, 3.50) vs 2.06 (1.7, 2.56), p = 0.002]. The patients were also sorted into three groups according to their NLR, and this revealed that the groups with higher NLRs had a higher risk of developing AKI postoperatively than those with a lower NLR (30% vs 25% vs 55.8%, p = 0.003). In addition, a multivariable logistic regression analysis showed that the patients with an elevated preoperative NLR had a higher risk of developing AKI postoperatively [odds ratio (OR) = 4. 91, 95% confidence interval (CI): 1.45–16.58, p = 0.0104], thereby confirming that NLR has predictive utility independent of other recognized risk factors [Citation12]. The results of the current study are consistent with those of the study described above. Specifically, multivariable logistic regression analysis in the current study revealed that NLR is an independently associated high-risk factor for CI-AKI and that an increase in NLR was associated with an increased incidence of CI-AKI. Moreover, the five ML models demonstrated that NLR is significantly predictive of CI-AKI.
The relationship between NLR and CI-AKI has been extensively studied in myocardial infarction and acute coronary syndrome. A prospective study by Kurtul et al. of patients with non-ST-elevation myocardial infarction (NSTEMI) found that a high NLR (≥ 3.46) was independently associated with CI-AKI risk (OR = 2.631, 95% CI: 1.146–6.060, p = 0.022) and predicted CI-AKI occurrence with 73% specificity and 70% sensitivity (AUC = 0.787) [Citation13]. Kaya et al. [Citation14] investigated the correlation between NLR and CI-AKI in an ST-elevation myocardial infarction (STEMI) population undergoing PCI and found that a high NLR (> 6.35) predicted the occurrence of CI-AKI with 75% sensitivity and 65% specificity (AUC = 0.763). Compared with the above-described studies, the AUC of NLR in this study was relatively low, and the cutoff was also lower, which may be related to the elective nature of our population, which indicates that it comprised patients with the less severe inflammation than those in other studies’ samples (which comprised patients with severe inflammation). Thus, a larger sample size may be needed to obtain a result consistent with previous studies.
To improve the preoperative prediction of the risk of CI-AKI, this study used NLR with other relevant parameters and five ML methods to build five ML-based preoperative CI-AKI risk-predicting models. The results showed that the following four parameters played the most significant roles in each model: NLR, Scr concentration at admission, FPG concentration, and β-blocker use. Previous research reported that the most important risk factor for developing CI-AKI in CKD was an eGFR ≤ 60 mL/min/1.73 m2 [Citation15]. Hyperglycemia may contribute to the development of CI-AKI by triggering oxidative stress and vasoconstriction and by reducing the delivery of oxygen to the kidney and reducing kidney volume depletion via osmotic diuresis [Citation16,Citation17]. β-Blockers may enhance vasodilation by increasing the concentrations of nitric oxide, which would protect against the nephrotoxic effects of CM [Citation18].
The five ML models exhibited good predictive performance; in decreasing order of AUC magnitude, their relative performances were as follows: NB > GBDT = LR > RF > XGBoost. It is still controversial which ML method is the best. Parreco et al. [Citation19] developed three ML models (GDBT, LR, and deep learning models) to predict the occurrence of AKI based on various parameters of 151,098 patients and discovered that the GBDT model afforded the most accurate predictions (AUC = 0.834). Liu et al. [Citation20] built XGBoost, LR, support-vector machine, and RF models to predict mortality in patients with AKI admitted to an ICU and showed that the most effective model was the XGBoost model [AUC, 0.796 (p < 0.01); F1, 0. 922 (p < 0.01); and accuracy = 0.860]. A study of 1,495 acute myocardial infarction (AMI) patients found that the AUC of an RF model incorporating the 15 most relevant variables was 0.82 (95% CI: 0.76–0.87), whereas the AUC of the best LR model was 0.69 (95% CI: 0.62–0.76), demonstrating that an RF algorithm can be used to accurately identify the risk of CI-AKI in patients with AMI [Citation21–23]. Nevertheless, the above-mentioned studies have shown that ML models are superior to traditional statistical models in predicting the occurrence of CI-AKI. Moreover, the AUCs of the ML models for predicting the occurrence of CI-AKI were significantly greater than that of the univariable (NLR-based) model. However, the variation between studies in terms of which type of model was best may also be attributable to the characteristics of a given model, the absence of some data from a given dataset, and the inclusion of different indicators. To resolve the problem of class imbalance and improve the performance of the model, The SMOTE analysis was performed. To avoid its drawbacks of noise or overfitting, we oversampled only on the training data and cross-validation was used.
The study has some limitations. First, the models were established based on single-center data. Second, some patients had been discharged within 48 h after CAG or PCI, so the postoperative Scr concentrations of these patients were missing, which might have led to an underestimation of the incidence of CI-AKI. Third, more indicators need to be included in the model, and further adjustments to the test at a later stage are required to reduce the scale, to enable the use of the model for CI-AKI evaluation in clinical settings. Fourth, our study was retrospective, which was prone to confounding and bias. The models need further prospective and external validation. Fifth, all the variables were obtained after admission, without considering that indicators were dynamically changing. However, AKI takes place at hourly intervals. Recently, some new machine learning models utilized multiple time points leading up to AKI to predict AKI onset [Citation10]. It is helpful for real-time risk assessment, especially in the intensive care unit.
In conclusion, this study found that a high NLR(>2.844) was an independently predictive marker of CI-AKI in a relatively large cohort of elective vascular intervention. Constructed five ML models incorporating NLR and other important risk factors that exhibited good performance in predicting the occurrence of CI-AKI. These findings should aid the development of ML models to identify and diagnose patients at risk of CI-AKI, so they can receive rigorous preventive measures.
Supplemental Material
Download PDF (125.6 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Ramachandran P, Jayakumar D. Contrast-induced acute kidney injury. Indian J Crit Care Med. 2020;24(Suppl 3):1–10. doi: 10.5005/jp-journals-10071-23379.
- Bu X, Zhang L, Chen P, et al. Relation of neutrophil-to-lymphocyte ratio to acute kidney injury in patients with sepsis and septic shock: a retrospective study. Int Immunopharmacol. 2019;70:372–377. doi: 10.1016/j.intimp.2019.02.043.
- Koo CH, Eun Jung D, Park YS, et al. Neutrophil, lymphocyte, and platelet counts and acute kidney injury after cardiovascular surgery. J Cardiothorac Vasc Anesth. 2018;32(1):212–222. doi: 10.1053/j.jvca.2017.08.033.
- Yang Z, Qiao Y, Wang D, et al. Association between inflammatory biomarkers and contrast-induced acute kidney injury in ACS patients undergoing percutaneous coronary intervention: a cross-sectional study. Angiology. 2023:33197231185445. Online ahead of print. doi: 10.1177/00033197231185445.
- Tanık VO, Çınar T, Velibey Y, et al. Neutrophil-to-lymphocyte ratio predicts contrast-induced acute kidney injury in patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention. J Tehran Heart Cent. 2019;14(2):59–66.
- Ösken A, Öz A, Keskin M, et al. The association between neutrophil-to-lymphocyte ratio and contrast-induced acute kidney injury in patients with carotid artery stenting. Vascular. 2021;29(4):550–555. doi: 10.1177/17085381211012562.
- Samad MD, Ulloa A, Wehner GJ, et al. Predicting survival from large echocardiography and electronic health record datasets: optimization with machine learning. JACC Cardiovasc Imaging. 2019;12(4):681–689. doi: 10.1016/j.jcmg.2018.04.026.
- Ambale-Venkatesh B, Yang X, Wu CO, et al. Cardiovascular event prediction by machine learning: the multi-ethnic study of atherosclerosis. Circ Res. 2017;121(9):1092–1101. doi: 10.1161/CIRCRESAHA.117.311312.
- Kellum JA, Lameire N,. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (part 1). Crit Care. 2013;17(1):204. doi: 10.1186/cc11454.
- Sun L, Zhu W, Chen X, et al. Machine learning to predict contrast-induced acute kidney injury in patients with acute myocardial infarction. Front Med. 2020;7:592007. doi: 10.3389/fmed.2020.592007.
- Sato Y, Takahashi M, Yanagita M. Pathophysiology of AKI to CKD progression. Semin Nephrol. 2020;40(2):206–215. doi: 10.1016/j.semnephrol.2020.01.011.
- Guangqing Z, Liwei C, Fei L, et al. Predictive value of neutrophil to lymphocyte ratio on acute kidney injury after on-pump coronary artery bypass: a retrospective, single-center study. Gen Thorac Cardiovasc Surg. 2022;70(7):624–633. doi: 10.1007/s11748-022-01772-z.
- Kurtul S, Sarli B, Baktir AO, et al. Neutrophil to lymphocyte ratio predicts SYNTAX score in patients with non-ST segment elevation myocardial infarction. Int Heart J. 2015;56(1):18–21. doi: 10.1536/ihj.14-175.
- Kaya A, Kaya Y, TOPçU S, et al. Neutrophil-to-lymphocyte ratio predicts contrast-induced nephropathy in patients undergoing primary percutaneous coronary intervention. Angiology. 2014;65(1):51–56. doi: 10.1177/0003319713484789.
- Wang H, Gao T, Zhang R, et al. The intellectual base and global trends in contrast-induced acute kidney injury: a bibliometric analysis. Ren Fail. 2023;45(1):2188967.
- Parreco J, Soe-Lin H, Parks JJ, et al. Comparing machine learning algorithms for predicting acute kidney injury. Am Surg. 2019;85(7):725–729. doi: 10.1177/000313481908500731.
- Giannini F, Latib A, Jabbour RJ, et al. Impact of post-procedural hyperglycemia on acute kidney injury after transcatheter aortic valve implantation. Int J Cardiol. 2016;221:892–897. doi: 10.1016/j.ijcard.2016.07.029.
- Kumar N, Khan SI, Versha F, et al. Comparison of effect of nebivolol and bisoprolol on sexual function of hypertensive female patients. Cureus. 2021;13(5):e15062. doi: 10.7759/cureus.15062.
- Palomba H, DE Castro I, Neto AL, et al. Acute kidney injury prediction following elective cardiac surgery: AKICS score. Kidney Int. 2007;72(5):624–631. doi: 10.1038/sj.ki.5002419.
- Liu J, Wu J, Liu S, et al. Predicting mortality of patients with acute kidney injury in the ICU using XGBoost model. PLOS One. 2021;16(2):e0246306. doi: 10.1371/journal.pone.0246306.
- Lu JY, Hou W, Duong TQ. Longitudinal prediction of hospital-acquired acute kidney injury in COVID-19: a two-center study. Infection. 2022;50(1):109–119. doi: 10.1007/s15010-021-01646-1.
- He J, Lin J, Duan M. Application of machine learning to predict acute kidney disease in patients with sepsis associated acute kidney injury. Front Med. 2021;8:792974. doi: 10.3389/fmed.2021.792974.
- Fathima Begum M, Narayan S. A pattern mixture model with long short-term memory network for acute kidney injury prediction. JKing Saud Univ - CompInfor Sci. 2023;35(4):172–182. doi: 10.1016/j.jksuci.2023.03.007.