Abstract
Aim of the Study: Immediate breast reconstruction is often applied after mastectomy. However, inappropriate surgical technique, postoperative radiotherapy and infection may lead to tissue necrosis and implant protrusion. Traditional therapies frequently fail. However, previous data suggested that capsule flaps may be appropriate for the salvage of implants. Our goal was to investigate the usefulness of capsuloplasty in patients with exposed breast implant and to monitor the blood supply of capsule flaps during the operation. Materials and Methods: Capsuloplasty was performed in 19 patients with exposed implant. After removal of necrotic tissue, capsulotomy was performed, the planned flap was dissected free, the implant was covered with the flap and the wound was then closed. During operation, the blood flow of the flap was determined by means of laser Doppler flowmetry. Moreover, tissue samples were taken for histology and immunostaining for CD34. Results: The postoperative follow-up showed that capsule flaps survived in each case: no complications were found. The blood flow of the flaps did not change significantly during the intervention as compared with the baseline values. The histology and the immunohistochemistry revealed considerable vascularization and angiogenesis in the flap. Conclusions: Capsule flaps seem to be appropriate for the salvage of exposed implants and for enhancement of implant cover in the case of thin and injured tissue.
INTRODUCTION
Immediate one-stage breast reconstruction is becoming a widely-accepted and preferred method. Implants should be covered with tissue of appropriate thickness and viability especially if patients receive postmastectomy radiation therapy. It is known that radiotherapy may be accompanied by a number of complicationsCitation1 including impaired wound healing, wound separation, infection and fistula.Citation2–4 These factors may lead to a considerable contraction of the capsule around the implant. This shrinking makes the surface of the implant irregular which therefore exerts uneven pressure on the overlying skin.
According to a hypothesis, the increased pressure affecting such areas may impair the microcirculation of the covering tissue layer potentially resulting in necrosis and exposure of the implant.Citation4 Inappropriate surgical technique may also cause insufficient local blood supply leading to necrosis and implant protrusion. Accompanying infection may contribute to this process. Although exposed implants are traditionally treated by insertion of a new one, many authors have reported successful salvage of implantCitation1–3 or alternative therapeutic strategies.Citation4–8 However, these interventions may fail in cases of previous radiotherapy or where tissue is injured or thin, necessitating implant removal.
For such cases, capsuloplasty seems to be an appropriate technique. The capsule appearing around the implant is a reaction to foreign material.Citation7,Citation9 It consists of fibroblasts and collagen fibers, has own blood supply and previous radiotherapy contributes to its development.Citation1 Bengston and coworkers described the application of capsule flap decades ago. According to their animal experiments, capsule flaps are viable and their vascular system is sufficient for the nutrition of the overlying skin graft.Citation10 In human, several areas of use of capsule flap were reported e.g., prevention of implant wrinkling,Citation7,Citation11 pharyngeal reconstruction,Citation12 shaping of inframammary foldCitation13 and cover for exposed implants.Citation5–8 However, the blood flow in capsule flaps has not yet been quantitatively determined in vivo.
Thus, the goal of our present study was to investigate the usefulness of capsuloplasty in patients with exposed breast implant and to monitor the blood supply of the capsule flaps during the operation.
MATERIALS AND METHODS
Patients
Capsuloplasty was performed in 19 females between January 2016 and November 2017. These patients underwent earlier mastectomy and immediate breast reconstruction. Their average age was 47.6 years (range: 33–72 years). The right side was affected in 10 cases and the left side in 9 cases. 4 patients underwent bilateral mastectomy. Bilateral capsuloplasty was performed in 3 of these 4 patients, the remaining 1 female underwent unilateral capsuloplasty (right side). demonstrates the localization of the defects indicating the operation. None of these patients received radiotherapy except 1 patient who underwent irradiation 1 year before mastectomy.
TABLE 1. Localization of the defects indicating the operation.
Surgical Procedures
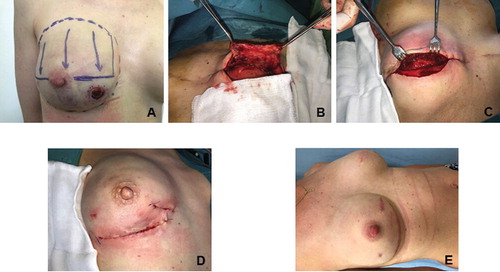
Each intervention was preceded by careful consideration of the following parameter: quality and thickness of the breast skin, presence of inflammation, discharge and fistula, previous radiotherapy, localization of tissue damage, patient requirements and the extension of necrosis and wound separation. The patients were carefully observed in order to detect visible signs of inflammation (erythema, edema). Moreover, leukocyte number, C-reactive protein and procalcitonin levels were also measured in each patient and samples were taken for microbiological examination. Signs of serious inflammation and large tissue defect were considered exclusion criteria. However, in case of the involved patients the mentioned parameters did not display elevation and pathogenic bacteria were not found. (If capsule flap is not feasible, the implant is to be removed and delayed reconstruction with a flap e.g., latissimus flap or abdominal TRAM shall be performed.) demonstrates a patient chosen for capsuloplasty. Apivotal point was the timing: the intervention should not be performed sooner than an appropriate capsule is formed around the implant. The tissue defect in our patients appeared 8–13 weeks after the mastectomy (median interval: 9 weeks). By this time, the capsule around the implant was well-developed therefore it was appropriate to be used for reconstruction. When the complication was recognized, the patients started to be prepared for the reconstruction which was performed within 3–5 days. During this period, the defect was covered with sterile dressing. Perioperative antibiotic therapy was launched that involved daily 1000 mg cefuroxime (2 × 500 mg) administered orally. This therapy lasted 10-14 days. Another important issue was the determination of the area from which capsule can be gained for reconstruction. In 3 cases, an attempt was made to close the wound primarily after removal of the necrotic tissue. The operation involved the following steps: after opening the wound the necrotic parts were excised, the implant was removed and capsulotomy was performed, the base of the flap remained intact, the planned flap was then dissected free (). After that, the implant was positioned and covered with the capsule flap (). Mentor's Cohesive III implant with anatomical shape and textured surface was applied. In most cases, new implants were used. In a minority of the cases, when the risk of infection and inflammation seemed to be low, the same old implants were applied. If the wound was able to be closed tension free after application of the capsule flap, the implant size was not reduced. If the tension free wound closure seemed to have difficulties, a smaller implant was chosen. The wound was closed with sutures (). Drainage was applied when necessary. Various capsule flaps were applied: anterior-superior medial, anterior-superior-lateral, in 1 case divided flap, and also posterior flaps from the chest wall. In 3 cases, thoraco-epigastrial fasciocutaneous flaps were used together with capsule flap in order to complete the reconstruction due to a large defect.
FIGURE 1. Photo documentation of the surgical intervention. A: A patient selected for capsuloplasty. B: The dissected capsule flap. C: The implant after positioning and covering with the capsule flap. D: The closed wound. E: The healed wound 3 month after the operation.
Patients were discharged on 3rd-5th postoperative day. An examination was performed 1 week after the surgery. The second examination and removal of the stitches were 1 week later. Following this, the patients were examined monthly once (inspection and palpation of the operated site and the above mentioned laboratory examinations were performed, too). Ultrasound imaging was performed in every 3 months (presence of capsular contracture and peri-implant fluid).
Laser Doppler Flowmetry
Microcirculation of the flaps was monitored by means of the PeriFlux System 5000 (Perimed, Järfälla, Sweden). This equipment transmits low power laser light (780 nm) to the tissue via a fiber optic probe. The returning light is processed and the relative number and velocity of the blood cells in the tissue are calculated and presented as blood perfusion. The sensor was fixed to the tissue with a sterile adhesive strip provided by the manufacturer. Measurements were performed at 4 different time points: before the incision of the intact capsule (baseline), after capsulotomy, after preparation of the capsule flap and after fixation of the flap. At each time point, recordings were made for 5 minutes. Perisoft for Windows software was used for data collection, storage and analysis. The data are presented as perfusion unit (P.U.).
Histology and Immunohistochemistry
During operation, biopsies were taken from the capsule. Tissue samples were fixed in a buffered solution of formaldehyde (4%), embedded in paraffin and 4-μm thick sections were taken. In addition to routine haematoxylin-eosin staining, sections were processed for immunohistochemical localization to highlight CD34 positive vessel density. Primary antibody to CD34 (clone QBEN/10 M7165; DAKO Glostrup, Denmark) was used at 1:200 (20 min). Antigen retrieval was performed by Bond Epitope Retrieval solution 2 at pH = 9 by BOND MAX Autostainer (Leica Biosystems, Newcastle Ltd., UK). Immuno-sections were counterstained with conventional haematoxylin.
Statistical Analysis
Data analysis was performed with SigmaStat for Windows (Jandel Scientific, Erkrath, Germany). Since the normality test (Shapiro-Wilk) failed in few cases, nonparametric test was chosen. Friedman repeated- measures analysis of variance on ranks was applied. In the Figure and Results, median values (M) with 25th and 75th percentiles (25p and 75p, respectively) are given, p < 0.05 was considered statistically significant.
RESULTS
Attempts at the primary closure of wounds after removal of necrotic tissue failed in the above mentioned 3 cases: the implants were exposed again. However, application of capsule flaps led to the healing of these patients without complication. Postoperative follow-up (ranging from 2 months to 19 months) showed that capsule flaps survived in each case. No signs of inflammation, infection, hematoma, wound separation and implant protrusion were found. Slight erythema was detected in 2 cases. In few cases, uneven surface and wrinkling were detected. However, our examinations excluded the capsular contracture and all of these signs ceased within 3 months. shows a patient in the 3rd postoperative month, a complete healing can be seen.
As concerns microcirculation of the flaps, the baseline median value in capsule flaps was 98.97 P.U. (25p = 73.56, 75p = 124.09). The perfusion in the capsule did not change after the capsulotomy (M = 106.96%, 25p = 62.82, 75p = 157.07) as referred to the baseline values. Although a slight decrease was measured after preparation of the capsule (M = 64.08%, 25p = 33.36, 75p = 135.99) and fixation of the flap (M = 51.41%., 25p = 32.7, 75p = 96.99), this change was not statistically significant ().
FIGURE 2. The blood flow of capsule flaps and thoraco-epigastrial fasciocutaneous flaps. Caps.: capsulotomy, Inc.: incision, Prep. of the flap: preparation of the flap, Fix. of the flap: fixation of the flap. Values are referred to the baseline and are given as percentage. Median values with 25th and 75th percentiles are demonstrated. A: blood flow of the capsule flaps in different stages of the operation. B: perfusion of the thoraco-epigastrial fasciocutaneous flaps during different steps of the intervention.
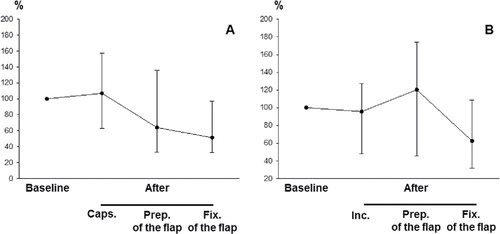
The baseline values of the thoraco-epigastrial fasciocutaneous flaps: M = 14.87 P.U., 25p = 10.37, 75p = 32.15. No decrease was found in their blood after capsulotomy (M = 95.56%, 25p = 48.14, 75p = 127.44), after preparation of the capsule (M = 120.27%, 25p = 45.32, 75p = 173.77) or after fixation of the flap (M = 62.52%, 25p = 31.58, 75p = 108.59) ().
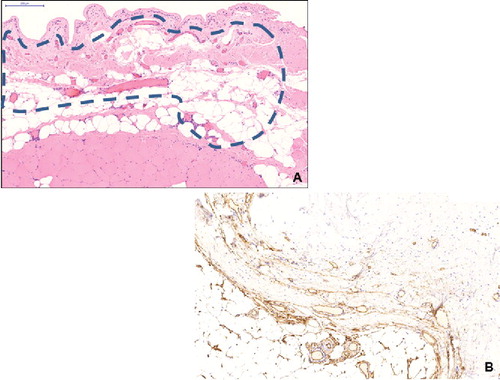
Histological analysis revealed that capsules were well-vascularized and several vessels were present in the connective tissue which may provide sufficient blood supply for the capsule (). Immunohis- tochemistry confirmed this finding: the CD34-positive structures demonstrated angiogenesis in the capsule ().
FIGURE 3. A: Low power micrograph of the capsule (haematoxylin-eosin staining, slide scanning, scale bar: 200 μm). Perforating vessels in the connecting tissue between striated muscle and capsule (dashed line). B: CD34-positive structures in the capsule (immunohistochemistry for CD34, counterstaining with haematoxylin, CD34-positive parts appear brown).
DISCUSSION
Salvage of exposed implants is a great challenge in reconstructive surgery. Different factors may lead to implant protrusion e.g., errors in planning, thermal and mechanic injuries as surgical complications, smoking in the patient’s history or previous radiotherapy. In our Institution, the ratio of immediate breast reconstruction with implant comes to 41% while local complications accompany 11.6% of these cases. Traditional therapeutic approaches involve antibiotics, drainage, rinsing, capsulotomy, change of the device and primary closing of the wound after excision of the necrotic tissue.Citation5–7 However, they may also fail in cases of decreased tissue viability and irradiation. Implant protrusion is a gradual process and its later stages require a more invasive surgical intervention.Citation14 Several techniques are used for the covering of implants e.g., deepithelialized skin,Citation15,Citation16 abdominal fascial flaps,Citation17 acellular dermal matrix (ADM),Citation18–21 autologous dermal graft22 and polyglycol mesh.Citation23 If signs of inflammation are not detected, latissimus dorsi flaps or local perforator flap can be applied.Citation24,Citation25 In cases of inflammation, the implant should be removed and later reconstruction or implantation of autologous fat can be chosen.Citation8 However, these procedures may have disadvantages. ADM is expensiveCitation26 and its application can be accompanied by seroma and infection.Citation7,Citation27 Furthermore, patients often refuse more radical surgical therapies (e.g., different flap techniques) due to the esthetic and functional damage to the donor site, and they prefer less radical methods.
Capsule flaps provide a less invasive and cost- effective solution. In animal experiments, capsules were used to support the survival of transplanted dermal graftsCitation28 as randomCitation10 or axial flaps.Citation29,Citation30 It has also been shown that capsule flaps are suitable for the correction of postimplant breast ripplingCitation31 and contour deformities of the breast.Citation7 Capsule flap can be obtained from the anterior surface and also from the tissue layer adjacent to the chest wall. Subject to localization of the defect and the viability of the tissue, superior, inferior, medial or lateral flaps can be applied.Citation10,Citation28–30
Since sufficient blood supply is a cornerstone of tissue survival, several investigations have focused on the vascularity of capsule flaps. Some evidence has already indicated the appropriate blood supply of the capsule flap. According to clinical observation, bleeding of the edges when tailoring the flap indicates a good vascularization.Citation7 Moreover, a histological examination found angiogenesis in non-expanded capsules from the 4th postoperative week on, and the peak of this process was achieved by the 8th week.Citation32 It is a further question whether expansion of the flap influences the vascularization and perfusion of the tissue. In expanded flaps, vessels of higher volume were found as compared to primer flaps, but no statistically significant difference was detected in terms of vessel density.Citation10 In another study, the radioactive microsphere technique did not reveal difference between the blood flow of expanded and non-expanded flaps.Citation33
Our results, in accordance with findings in literature, show that capsule flaps provide a well-vascularized layer which prevents protrusion of the implant and decreases tension, thereby promoting wound healing and reduced risk of inflammation and superinfection. An important novel aspect of our study is the in vivo determination of microcirculatory status during the operation. Laser Doppler flowmetry was chosen for these measurements since it is an accurate and reliable method for assessing microcirculatory function.Citation34 Our in vivo finding has confirmed that surgical stress does not decrease the blood supply of flaps which then provided an optimal ground for the healing process.
In conclusion, the capsule flap seems to be appropriate for salvage of exposed implants and for enhancement of implant cover in case of thin and injured tissue. Capsule flaps are reliable, not difficult to prepare, have good circulation and may therefore play an important role in reconstructive surgery of the breast. On the other hand, capsule flaps shall not be applied in case of serious inflammation and large tissue defect. Moreover, the number of published cases of breast reconstruction with capsule flaps is relatively low.Citation7 Hence, more experience with the technique may be needed before widespread adaptation.
DECLARATION OF INTEREST
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Behranwala KA, Dua RS, Ross GM, Ward A, A’hern R, Gui GP. The influence of radiotherapy on capsule formation and aesthetic outcome after immediate breast reconstruction using biodimensional anatomical expander implants. J Plast Reconstr Aesthetic Surg. 2006;59:1043–1051.
- Ariyan S. Radiation injury. In: Mathes SJ, ed. Plastic Surgery. Philadelphia, Pa: Saunders Elsevier; 2006:835–853.
- Forman DL, Chiu J, Restifo RJ, Ward BA, Haffty B, Ariyan S. Breast reconstruction in previously irradiated patients using tissue expanders and implant: a potentially unfavourable result. Ann Plast Surg. 1998;40:360–363.
- Abramo AC, Casas SG, Dorta AA, Mateus S, Trujillo R. Late spontaneous extrusion of a texturized silicone gel mammary implant. Aesthetic Plast Surg. 1999;23:433–436.
- Weber J Jr, Hentz RV. Salvage of the exposed breast implant. Ann Plast Surg. 1986;16:106–110.
- Planas J, Carbonell A, Planas J. Salvaging the exposed mammary prosthesis. Aesthetic Plast Surg. 1995;19:535–540.
- Persichetti P, Segreto F, Pendolino AL, Del Buono R, Marangi GF. Breast implant capsule flaps and grafts: a review of the literature. Aesthetic Plast Surg. 2014;38:540–548.
- Spear SL, Howard MA, Boehmler JH, Ducic I, Low M, Abbruzzese MR. The infected or exposed breast implant: management and treatment strategies. Plast Reconstr Surg. 2004;113:1634–1644.
- Bassetto F, Scarpa C, Caccialanza E, Montesco MC, Magnani P. Histological features of periprosthetic mammary capsules: silicone vs polyurethane. Aesthet Plast Surg. 2010;34:481–485.
- Bengtson BP, Ringler SL, George ER, DeHaan MR, Mills KA. Capsular tissue: a new local flap. Plast Reconstr Surg. 1993;91:1073–1079.
- Hobman J, Sharpe DT. Strategies forminimising palpable implant rippling in the augmented breast. In: Stone C, ed. The Evidence for Plastic Surgery. Harley, Shrewsbury, England:TFM Publishing Ltd; 2008: 263–272.
- Persichetti P, Francesco Marangi G, Gigliofiorito P, Segreto F, Brunetti B. Myocapsular pectoralis major flap for pharyngeal reconstruction after cervical necrotizing fasciitis. Plast Reconstr Surg. 2010;126:2279–2281.
- Persichetti P, Langella M, Filoni A, Cagli B, Tenna S. How to redefine the inframammary fold: the “slingshot” capsular flap. Ann Plast Surg. 2013;70:636–638.
- Fodor L, Ramon Y, Ullmann Y, Eldor L, Peled IJ. Fate of exposed breast implants in augmentation mammoplasty. Ann Plast Surg. 2003;50:447–449.
- Hammond DC, Capraro PA, Ozolins EB, Arnold JF. Use of a skin-sparing reduction pattern to create a combination skin-muscle flap pocket in immediate breast reconstruction. Plast Reconstr Surg. 2002;110:206–211.
- Ibrahim AE, Atiyeh BS, Dibo SA, Sarhane KA, Abbas JS. De-epithelialized dermal barrier for a safe immediate prosthetic breast reconstruction post circum vertical skin-sparing/reducing mastectomy (SSM/SRM). Eur J Plast Surg. 2012;35:787–793.
- Isken T, Onyedi M, Izmirli H, Alagoz S, Katz R. Abdominal fascial flaps for providing total implant coverage in one-stage breast reconstruction: an autologous solution. Aesthetic Plast Surg. 2009;33:853–858.
- Breuing KH, Colwell AS. Inferolateral AlloDerm hammock for implant coverage in breast reconstruction. Ann Plast Surg. 2007;59:250–255.
- Salzberg CA, Ashikari AY, Koch RM, Chabner-Thompson E. An 8-year experience of direct-to-implant breast reconstruction using human acellular dermal matrix (Allo-Derm). Plast Reconstr Surg. 2011;127:514–524.
- Sbitany H, Langstein HN. Acellular dermal matrix in primary breast reconstruction. Aesthet Surg J. 2011;31(7 Suppl):30S–37S.
- Nahabedian MY. AlloDerm performance in the setting of prosthetic breast surgery, infection, and irradiation. Plast Reconstr Surg. 2009;124:1743–1753.
- Hudson DA, Adams KG, Adams S. Autologous dermal graft in breast reconstruction. Ann Plast Surg. 2012;68:253–256.
- Mofid MM, Meininger MS, Lacey MS. Veritas® bovine pericardium for immediate breast reconstruction: a xenograft alternative to acellular dermal matrix products. Eur J Plast Surg. 2012;35:717–722.
- Cagli B, Manzo MJ, Tenna S, Piombino L, Poccia I, Persichetti P. Heterologous reconstruction and radiotherapy: the role of latissimus dorsi flap as a salvage. Acta Chir Plast. 2012;54:45–51.
- Unal C, Gercek H, Yasar EK, Utkan Z. Lateral intercostal artery perforator flap used in salvage of exposed tissue expander of breast: case report. Microsurgery. 2011;31:495–498.
- Jansen LA, Macadam SA. The use of AlloDerm in postmastectomy alloplastic breast reconstruction: Part II. A cost analysis. Plast Reconstr Surg. 2011;127:2245–2254.
- Parks JW, Hammond SE, Walsh WA, Adams RL, Chandler RG, Luce EA. Human acellular dermis versus no acellular dermis in tissue expansion breast reconstruction. Plast Reconstr Surg. 2012;130:739–746.
- Heymans M, Lengele B, Lahlali N, Vanwijck R. A periimplant capsule flap. Br J Plast Surg. 1993;46:456–459.
- Cariou JL, Hilligot P, Arrouvel C, Banzet P. Experimental concept of periprosthetic membrane neo-flap with axial vascular pedicle. Ann Chir Plast Esthet. 1991;36:471–479.
- Schuringa MC, Hartman EH, Ruhe’ PQ, Jansen JA, Spauwen PH. Formation of a reliable capsular flap in a rat model. J Plast Reconstr Aesthetic Surg. 2007;60:536–542.
- Massiha H. Scar tissue flaps for correction of postimplant breast rippling. Ann Plast Surg. 2002;48:505–507.
- Thomson HG. The fate of the pseudosheath pocket around silicone implants. Plast Reconstr Surg. 1973;51:667–671.
- Sasaki GH, Pang CY. Pathophysiology of skin flaps raised on expanded pig skin. Plast Reconstr. Surg. 1984;74:59–67.
- Swiontkowski MF. Laser Doppler flowmetry – development and clinical application. Iowa Orthop J. 1991;11:119–126.
