Hepatocellular carcinoma (HCC) is the fifth most common cancer worldwide [Citation1]. Screening at-risk patients aid early diagnosis and improve survival. Tumor stage, liver (dys)function, patient co-morbidity, performance status, and local resources determine the management. Liver resection (LR), liver transplantation, and local ablative therapy (LAT) are classified as curative treatment options. LAT can be performed via a percutaneous approach by interventional radiology guidance under moderate sedation. Thus, the peri-procedure risk of LAT is less as it avoids surgery and general anesthesia. Radiofrequency ablation (RFA) and microwave ablation (MWA) are commonly LAT modalities. Our group conducted a meta-analysis and reported lower procedural-related morbidity with similar oncological outcomes of RFA + transarterial chemoembolization (TACE) as LR [Citation2]. Though RFA is considered curative, there is substantial evidence that LR offers better recurrence-free survival (RFS) and overall survival (OS). A recent meta-analysis including 19 studies involving 15,071 patients reported that LR offers better long-term oncologic outcomes than RFA [Citation3]. One of the drawbacks of RFA includes higher local recurrence risk. Hence, refinements in RFA technology are required, and thus the study by Qu et al. is a crucial step forward [Citation4].
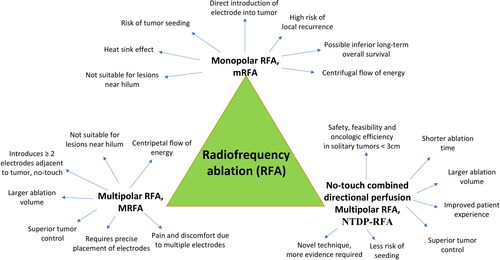
RFA uses rapidly alternating radiofrequency current through an electrode to cause marked ionic agitation and heat generation. This results in coagulative necrosis in solid abdominal organ tumors, including HCC. In addition, RFA stimulates secondary anticancer immunity due to activation of tumor-specific T lymphocytes and inducing expression of heat shock protein 70 [Citation5]. In conventional monopolar RFA (mRFA), the electrode is introduced into the tumor with centrifugal current spread. This may not achieve uniform tissue ablation, and the tumoricidal effect can be uneven. In tumors larger than 3 cm, multiple overlapping ablations may be necessary. The microbubble formed after index ablation obscures the unablated tissues and limits the accurate placement of further electrodes. Expandable needle electrodes, internally cooled electrodes, and perfusion electrodes can increase the ablation zone, but more clinical data are required. Further, the “heat-sink” effect (dissipation of thermal energy due to tumor proximity to the blood vessel) and tumor seeding are drawbacks of mRFA. The no-touch multipolar RFA (MRFA) introduces two or more electrodes adjacent to the tumor. The electrodes are placed around the periphery of the tumor, and heat conduction is from outside to within, i.e., centripetal. Thus, a more uniform thermal ablation is achieved without entering the tumor itself and thereby eliminating (or at least reducing) the risk of tumor seeding. A matched study by Hocquelet et al. on 362 patients with HCC ≤ 5 cm and cirrhosis showed superior local tumor control using MRFA compared to mRFA (p < 0.001) [Citation6]. Hirooka et al. reported three times larger ablation volume in MRFA compared to mRFA for HCC in the caudate lobe (40.0 ml vs. 13.2 ml, p < 0.0001), lower local tumor progression (LTP) rate for MRFA (12.5% vs. 22.9%; p = 0.004), and higher 2-year relapse-free survival rate for MRFA (65.1% vs. 22.7%; p = 0.004) [Citation7]. MRFA needs precise placement of electrodes and a relatively long ablation time. Also, as the coagulative tissue necrosis increases impedance, there is no guarantee of uniform temperature throughout the lesion volume. Qu et al. hypothesized that more uniform thermal conduction could be achieved by infusion of isotonic saline via the side holes of the tubing along the MRFA electrodes [Citation4]. Isotonic saline can reduce tissue carbonization, lower impedance, and increase thermo-electrical conductivity. This could achieve higher and more uniform ablation volume, with potentially reduced risk of local recurrence and improved survival outcomes.
Qu et al. report their experience using a novel no-touch combined directional perfusion RFA (NTDP-RFA) in 56 patients with a single HCC ≤3 cm on a background of cirrhosis [Citation4]. Internally cooled wet electrodes (14 G diameter) that can perform intraelectrode cooling and extraelectrode 0.9% saline perfusion (1 ml/min) were used. Two electrodes were used for tumors with a diameter of ≤ 20 mm; for tumors with a diameter between 20 and 30 mm, three electrodes were used. This is important as two electrodes create non-spherical shaped ablation zones with short transverse diameters on the plane perpendicular to the electrode insertion axis, while three electrodes can create a more spherically shaped ablation zone with a larger transverse diameter. The authors report the short-term efficacy of their innovative technique. The primary study endpoint was local tumor progression (LTP), defined as the appearance of new tumor foci within 2 cm of the edge of the ablation area by at least one follow-up imaging examination. The authors report 100% technical success. After a median ablation time of 8 (interquartile range (IQR) 6 − 8) min, the authors achieved a median ablation diameter of 49 (44.2 − 51.0) mm in HCC patients with a median tumor diameter of 26 mm (range 18.0 − 28.0). Five patients (8.9%) experienced grade A complications, and the median postoperative hospital stay was 4 (IQR 4 − 5) days. The 2-year LTP was 7.1% (n = 4). While the results are within expectations, this study endorses the safety, feasibility, and oncologic efficiency of the novel NTDP-RFA technique. summarizes the key elements of mRFA, MRFA, and NTDP-RFA.
The study is an essential milestone in HCC management, and we wish to discuss four relevant issues. First, the safety, feasibility, and oncologic efficiency of LAT in HCC management is well established. All clinical practice guidelines endorse the curative role of LAT in the multimodal management of selected HCC patients. With expanding indications, the technique has evolved. Patients prefer RFA as it is less invasive with minimal procedure-related morbidity. Despite classified as a curative modality, the survival outcomes of HCC patients managed with LR are better compared to RFA [Citation3, Citation8]. Shin et al. reported a meta-analysis comparing LR with LAT in HCC patients within Milan criteria [Citation8]. The authors included seven randomized controlled trials and eighteen matched non-randomized studies (2865 patients in the LR group and 2764 patients in the LAT group [RFA, MWA, RFA + TACE]) and concluded that LR was superior to RFA in terms of incidence of local recurrence and recurrence-free survival. Moreover, LR showed better oncologic outcomes than MWA or RFA + TACE. A meta-analysis comparing LR with RFA + TACE reported high LTP rates (OR 2.48, 95% CI 1.05–5.86, p = 0.04) in patients treated by RFA + TACE (compared to LR) [Citation2]. Thus, refinements in RFA technology are welcome to increase the pool of eligible patients for curative intent therapy, reduce local recurrence risk, and improve overall survival. MRFA results in the centripetal energy flow and ensures a good treatment effect at the periphery of the tumor. The novel NTDP-RFA technique can further improve the clinical outcomes, and further validation of this technique is necessary.
Second, with the MRFA technique, the electrodes are placed at the periphery of the tumor and not within the tumor, i.e., reduced risk of tumor seeding. A systematic review by Stigliano et al. on five cohorts with 1525 patients reported a median risk of 0.61% for seeding (range 0–5.56%) [Citation9]. However, there are technical limitations to place multiple electrodes along the periphery of the tumor via a percutaneous approach. Patients may not be able to tolerate the procedure under local anesthesia and moderate sedation. It is important to note that the authors excluded patients with lesions adjacent to the gallbladder, major blood vessels, bile ducts at the hepatic hilum, and surrounding organs. This restricts the patient pool that is suitable for treatment by this novel technique. However, Hirooka et al. demonstrated the safety of MRFA with no significant complications in 22 patients with caudate lobe HCC [Citation7]. Thus, we remain optimistic that with refinements in imaging technology and three-dimensional fusion in treatment planning, selection criteria for HCC patients deemed suitable for LAT will continue to expand.
Third, in this report, surgeons are trained in ultrasound and LAT, and the results may not be generalizable across other healthcare settings. Like other techniques or surgical procedures, NTDP-RFA should have a learning curve. Poon et al. demonstrated a learning curve of 50 patients in conventional MRFA, with morbidity of 16% in the first 50 patients compared to 0–10% in the subsequent 50 patients [Citation10]. In the report of Qu et al., the hepatobiliary surgeon has >15 years of experience in RFA. This experience likely confounds good outcomes: 100% technical success, 8.9% pleural effusion, and 3.5% ascites.
Lastly, as the authors had stringent exclusion criteria, these results cannot be generalized. More evidence is required if NTDP-RFA is effective in HCC patients with multiple nodules or solitary nodules >3 cm and tumors in proximity to critical structures. Artificial ascites creation and other means are reported to facilitate the expansion of selection criteria for LAT.
To conclude, the authors presented the use of NTDP-RFA, a novel technique using internally cooled wet electrodes with a directional injection function and demonstrated its safety with 100% technical success in solitary HCC <3 cm with improved ablation time and lower LTP compared to MRFA. This serves as an important milestone in HCC management, and the results need to be validated.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Wang B, Shelat VG, Chow JJL, et al. Prehabilitation Program Improves Outcomes of Patients Undergoing Elective Liver Resection. J Surg Res. 2020;251:119–125. doi:https://doi.org/10.1016/j.jss.2020.01.009.
- Gui CH, Baey S, D’Cruz RT, Shelat VG . Trans-arterial chemoembolization + radiofrequency ablation versus surgical resection in hepatocellular carcinoma—A meta-analysis. Eur J Surg Oncol. 2020;46(5):763–771. doi:https://doi.org/10.1016/j.ejso.2020.01.004.
- Xuan D, Wen W, Xu D, Jin T. Survival comparison between radiofrequency ablation and surgical resection for patients with small hepatocellular carcinoma: A systematic review and meta-analysis. Medicine (Baltimore). 2021;100(7):e24585. doi:https://doi.org/10.1097/MD.0000000000024585.
- Qu C, Li X-Q, Xia F, Xia F, Feng K, Ma K. The short-term efficacy of novel no-touch combined directional perfusion radiofrequency ablation in the treatment of small hepatocellular carcinoma with cirrhosis. J Invest Surg. 2021:1–8.: doi:https://doi.org/10.1080/08941939.2021.1931575.
- Pandya GJ, Shelat VG. Radiofrequency ablation of pancreatic ductal adenocarcinoma: the past, the present and the future. World J Gastrointest Oncol. 2015;7(2):6–11. doi:https://doi.org/10.4251/wjgo.v7.i2.6.
- Hocquelet A, Aubé C, Rode A, et al. Comparison of no-touch multi-bipolar vs. monopolar radiofrequency ablation for small HCC. J Hepatol. 2017;66(1):67–74. doi:https://doi.org/10.1016/j.jhep.2016.07.010.
- Hirooka M, Ochi H, Hiraoka A, et al. Multipolar versus monopolar radiofrequency ablation for hepatocellular carcinoma in the caudate lobe: Results of a propensity score analysis. Hepatol Res. 2017;47(7):658–667. doi:https://doi.org/10.1111/hepr.12791.
- Shin SW, Ahn KS, Kim SW, Kim TS, Kim YH, Kang KJ. Liver resection versus local ablation therapies for hepatocellular carcinoma within the Milan criteria: A systematic review and meta-analysis. Ann Surg. 2021;273(4):656–666. doi:https://doi.org/10.1097/SLA.0000000000004350.
- Stigliano R, Marelli L, Yu D, Davies N, Patch D, Burroughs AK. Seeding following percutaneous diagnostic and therapeutic approaches for hepatocellular carcinoma. What is the risk and the outcome? Seeding risk for percutaneous approach of HCC. Cancer Treat Rev. 2007;33(5):437–447. doi:https://doi.org/10.1016/j.ctrv.2007.04.001.
- Poon RT, Ng KK, Lam CM, et al. Learning curve for radiofrequency ablation of liver tumors: prospective analysis of initial 100 patients in a tertiary institution. Ann Surg. 2004;239(4):441–449. doi:https://doi.org/10.1097/01.sla.0000118565.21298.0a.