Abstract
Purpose
To compare the short-term therapeutic effects of S2-alar-iliac (S2AI) screw fixation and iliac screw fixation techniques in managing sacral fractures.
Methods
From September 2015 to May 2020, 42 patients with sacral fractures who underwent lumbopelvic fixation by a single surgeon were analyzed. The patients were divided into the S2AI screw group (19 patients) and the iliac screw group (23 patients). Operative data, reduction quality, postoperative complications, and functional outcomes were evaluated.
Results
The incidence of unplanned reoperation was significantly different between patients treated with S2AI screws than in those treated with iliac screws (0 versus 6, p = 0.02). The mean intraoperative estimated blood loss was 405.26 ± 229.67 mL in the S2AI screw group and 539.13 ± 246.32 mL in the iliac screw group (P = 0.08). No significant difference was observed in either group regarding the quality of reduction, functional outcome, or low back pain. The reduction quality based on the Matta criteria and excellent/good outcomes were 21/2 in the iliac screw group and 17/2 in the S2AI screw group. The functional outcomes based on the Majeed score and excellent/good/fair outcomes were 17/3/3 in the iliac screw group and 17/1/1 in the S2AI screw group. No complications, including implant breakage, loosening of the implant, or loss of reduction were found in either group during follow-up.
Conclusion
Both S2AI screws and iliac screws were effective in the treatment of sacral fractures. The use of S2AI screws, however, was independently associated with fewer unplanned reoperations for surgical site infection, wound dehiscence, and symptoms of screw protrusion than the use of iliac screws.
Introduction
The sacrum is the cornerstone of the spine and plays a decisive role in the stability of the pelvis [Citation1]. Longitudinal fractures of the sacrum cause pelvic ring vertical instability, and if combined with L5/S1 facet joint or medial facet joint fractures (Isler type B, C), or transverse sacral fractures (U, H, T, λ-shaped), it leads to lumbopelvic instability [Citation1–5]. Lumbopelvic fixation provides sufficient stability to accelerate the commencement of postoperative rehabilitation [Citation1, Citation3, Citation5, Citation6].
The traditional method of lumbopelvic fixation is the iliac screw technique [Citation1, Citation3, Citation6, Citation7]. Although it provides the advantage of rigid fixation, it also has disadvantages including screw prominence [Citation1, Citation3, Citation5, Citation6, Citation8], surgical site infection [Citation1, Citation3–6, Citation8], and wound dehiscence [Citation1, Citation6, Citation9]. Therefore, a better surgical approach is highly desired, one that provides the same stability as the iliac screw technique but avoids its disadvantages.
The S2AI screw technique is widely used for spinal deformity correction during spinal surgery. Since it shows strong lumbopelvic stability and few complications associated with screw prominence [Citation10–13], we introduced it into trauma surgery to treat sacral fractures. However, do these advantages still remain in the treatment of sacral fractures due to trauma? At present, few reports have compared these two kinds of fixations for traumatic sacral fractures. The purpose of this study was to compare the short-term results of these two technologies in the management of unstable posterior pelvic ring injuries resulting from sacral fractures.
Patients and methods
A retrospective analysis of unilateral sacral fractures was performed in this study between September 2015 and May 2020. The inclusion criteria were as follows: (1) unilateral sacral fractures (Denis II type, Denis III type) without neurological damage, (2) unilateral lumbopelvic fixation with S2AI screws or iliac screws, and (3) a follow-up duration of at least one year. The exclusion criteria were incomplete follow-up data, pathologic fractures, Denis I type fractures, and revision surgery for lumbopelvic fixation with iliac screws or S2AI screws.
A total of 42 patients were enrolled according to these criteria. The fixation techniques were iliac screw fixation in 23 patients and S2AI screw fixation in 19 patients. From September 2015 to June 2019, the iliac screw technique was exclusively used for lumbopelvic fixation, but from July 2019 onward, S2AI was selected preferentially.
All lumbopelvic fixation with iliac screw or S2AI screw fixation was performed by the same surgeon. Informed consent was obtained from all patients, and this study was approved by the institutional internal review board of the participating institution.
Surgical technique
When patients were stable both physiologically and hemodynamically, operative stabilization of the pelvic ring was performed.
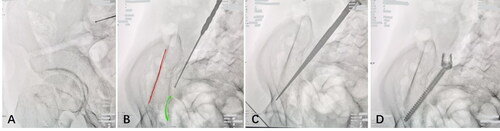
For patients treated with the S2AI screw technique, a posterior midline incision was started at the L4 or L5 spinous process and extended distally, ending proximal to the coccyx. The paravertebral muscles on the injured sides were dissected along the spinous process. Then, the L5 lamina, transverse processes, and facet joints were exposed, as well as the sacral lamina, ala sacralis, fracture sites, and S1 and S2 posterior sacral foramina. Displaced fractures were first reduced and then fixed. For fresh vertical displacement, the sacrum can be reduced by direct longitudinal distraction. If it was combined with a locked L5/S1 facet joint, unlocking by lateral distraction was performed first and then it was reduced by longitudinal distraction. Reduction can also be performed in combination with Schanz pins (introduced percutaneously into the posterior iliac crests and used as levers), ball-spike pushers, or reduction clamps. Pedicle screws were implanted at L5 and/or L4, and S2AI screws were implanted through the sacroiliac joint. The implants were lumbopelvic internal fixation systems from Double Medical Instruments (Double Medical Technology Inc., Xiamen, China). According to the freehand technique reported by Shillingford et al. [Citation14], the midpoint of the line connecting the lateral edge of the S1 and S2 foramina on the dorsal ala sacralis was selected as the guide needle insertion point. The guide needle insertion direction pointed to the anteroinferior iliac spine, with approximately 40° of abduction on the transverse plane and approximately 40° of caudal inclination on the sagittal plane. The exact trajectory was determined by intraoperative fluoroscopy. The awl was chosen to open the sacral cortex to prevent instrument migration. Then, the S2AI guide needle was passed through the sacral fenestration to perforate the sacroiliac joint, passing above the greater ischial notch and pointing in the direction of the anteroinferior iliac spine; a screw path 80–100 mm in length was drilled. A ball-tip probe was used to confirm that the screw path entered between the inner and outer plates of the ilium, the four walls were complete, and the bottom was a bony structure. The iliac oblique view was used to confirm that the guide needle was above the large sciatic notch, and the modified obturator inlet view (20°–30° examination side tilt combined with 30° inlet tilt) was used to verify that the guide needle was between the inner and outer plates of the ilium (). A screw 7.0 × 80–100 mm in size was placed along the guide needle after confirmation of satisfactory positioning on fluoroscopy.
Figure 1. Ideal fluoroscopy during surgery is one of the keys to successful surgery. (A) The ilial oblique view was used to confirm that the direction of screw insertion crossed the greater sciatic notch and pointed to the anterior inferior iliac spine. (B) The modified obturator inlet view (20°–30° examination side tilt combined with 30° inlet tilt) was used to confirm that the direction of screw insertion did not penetrate the inner and outer plates of the ilium (red line, outer plate of the ilium; green line, inner plate of the ilium). (C) After the direction of screw insertion is determined correctly, a screw path of 80–100 mm in length was made by an awl. (D) After a ball-tip probe confirmed that the four walls were intact, an S2AI screw was inserted along the screw path.
The paramedian incision was used in the iliac screw technique, but the soft tissue needed to be dissected to the posterior superior iliac spine (PSIS). The detailed surgical procedures have been reported in the previous literature [Citation15, Citation16]. Unlike the S2AI screws, the iliac screws were directly fixed to the ilium. Moreover, a small rectangular piece of the iliac crest needed to be removed at the implantation point to accommodate the height and width of the iliac screw tail. Its intraoperative and postoperative fluoroscopy and management were the same as those of the S2AI screws.
After reduction of the sacral fracture and lumbopelvic fixation, most patients with anterior pelvic ring injury (pubic ramus fracture, pubic symphysis dislocation, etc.) can be reduced spontaneously without reprocessing. If only poor or unstable anterior ring reduction can be achieved, open reduction is required.
Postoperative management
All patients were maintained on a non weight-bearing status on the affected side postoperatively. The patients were encouraged to perform isometric contraction of the lower limb muscle groups as long as the pain could be tolerated, 1–2 days after the operation. One week after surgery, the patient was gradually allowed to sit up, if it was not too painful. Four weeks after surgery, the patient could perform partial weight-bearing exercises with crutches, and if the patient had fractures in other parts of the lower extremities, the patient was instructed to perform weight-bearing training on the ground according to the fracture healing shown by the radiographs. Follow-up was conducted at 1, 2, and 3 months postoperatively and every 3 months thereafter. The implants were removed after bony union, usually 6–8 months postsurgery, unless the patients refused due to age or preference.
Patient data
Baseline characteristics were collected including age at surgery, sex, time interval from injury to surgery, mechanism of injury, injury severity score (ISS), classification of sacral fractures, and follow-up period. Operative data and clinical results were recorded including operative time, estimated blood loss, reduction quality, functional outcome, and total length of stay. The operation time was defined as the time taken for lumbopelvic fixation of the posterior pelvic ring, excluding the time for anterior ring fixation or other sites at the same stage. The estimated blood loss was defined loss during surgery in the lumbopelvic fixation, excluding the time for anterior ring fixation or other sites at the same stage. In addition, information regarding complications and morbidity was collected.
Data analysis
The Matta criteria [Citation17] were used to assess the quality of the reduction based on the anteroposterior, inlet, and outlet view X-rays. The reduction was graded by the maximal displacement measured on the 3 views of the pelvis: excellent (≤ 4 mm), good (4–10 mm), fair (10-20 mm), and poor (>20 mm). A satisfactory reduction quality was defined as meeting the excellent or good criteria.
The Majeed score [Citation18] was used to evaluate the degree of functional recovery postoperation. This score is evaluated in terms of pain (30 points), work (20 points), sitting (10 points), sexual life (4 points), and standing (36 points), with a total score of 100 points. 85–100 points is excellent, 70–84 points is good, 55–69 points is fair, and < 55 points is poor. The last follow-up functional result was included in the statistical analysis.
Unplanned reoperation refers to the following three conditions: surgical site infection requiring surgical removal of the infected tissue, wound dehiscence requiring surgical resection of necrotic tissue, and unbearable symptoms from screw protrusion requiring screw adjustment.
Statistical analysis
Statistical analysis was performed using SPSS 20.0 statistical software (IBM, USA). Measurement data following a normal distribution are presented as the mean ± standard deviation (SD), and an independent samples t-test was performed to assess significant differences between the two groups. Chi-square, Wilcoxon signed-rank, and Fisher’s exact probability tests were performed to compare categorical variables between the two groups. A value of P < 0.05 was considered to be statistically significant.
Results
As shown in , there were no statistically significant differences in the baseline data between the two groups. Neither the surgical data nor the clinical results were significantly different between the two groups. However, the estimated blood loss was slightly higher in the iliac screw group (539.13 ± 246.32 mL) than in the S2AI screw group (405.26 ± 229.67 mL, P = 0.08). All patients obtained satisfactory functional results in this study, and the excellent/good was 21/2 in the iliac screw group and 17/2 in the S2AI screw group. Most patients achieved satisfactory reduction, and the excellent/good/fair was 17/3/3 in the iliac screw group and 17/1/1 in the S2AI screw group ().
Table 1. Patient demographics.
Table 2. Operative data and clinical results.
Regarding the incidence of complications and increased morbidity, the iliac screw group had a significantly higher rate of unplanned reoperation than the S2AI screw group (26.1% versus 0.0%, P = 0.02). Among them, there were six (26.1%) unplanned reoperations, three (13.04%) due to surgical site infection, one (4.35%) due to wound dehiscence, and two (8.6%) due to unbearable symptoms of screw protrusion. The rates of low back pain and pass-out iliac plate were similar between the groups ().
Table 3. Incidence of complication and increased morbidity.
Discussion
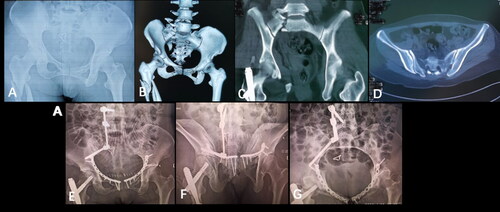
Before June 2019, lumbopelvic fixation with traditional iliac screws was widely applied to accomplish the fixation of sacral fractures in our institution (). Although the iliac screw technique provides adequate solid fixation, it has the disadvantages of screw protrusion, wound infection, and wound dehiscence. Orthopedic traumatologists are embracing and fearing the iliac screw technique. More recently, since July 2019, we achieved satisfactory short-term clinical results in managing sacral fractures using lumbopelvic fixation with S2AI screws (). The S2AI screw technique offers a new option for orthopedic traumatologists.
Figure 2. A male patient of zone II sacral fracture fixed with lumbopelvic technique was presented. (A) Preoperative anteroposterior X-ray of pelvis. (B) Preoperative three-dimensional reconstruction. (C, D) Preoperative CT scans. (E) Postoperative anteroposterior X-ray of pelvis.
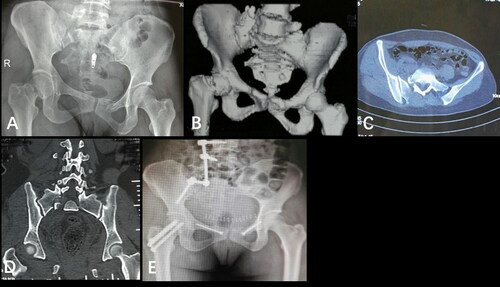
Figure 3. A female patient of zone II sacral fracture fixed with S2AI screw was presented. (A) Preoperative anteroposterior X-ray of pelvis. (B) Preoperative three-dimensional reconstruction. (C, D) Preoperative CT scans. (E-G) Postoperative anteroposterior, inlet, outlet X-ray of the pelvis.
The S2AI screw technique has few complications related to screw prominence. In our study, there were three surgical site infections, one wound dehiscence, and two unbearable symptoms of screw protrusion in the iliac screw group. However, there were no patients with wound dehiscence, infection, or screw protrusion in the S2AI group. These results are compatible with previously reported results [Citation11, Citation19], in which the characteristics of the patient populations were relatively heterogeneous. Elder et al. [Citation20] analyzed the clinical results of 161 patients (including patients with adult spinal deformity, high-grade spondylolisthesis, tumor, osteomyelitis/discitis, and trauma in the lumbosacropelvic region) who underwent iliac screw or S2AI screw fixation and found that S2AI screw fixation had lower rates of surgical site infection (1.5% versus 44.0%), and symptomatic screw prominence (0.0% versus 12.0%). We conducted a reasonable analysis of the reasons for these good results.
The depth of the insertion point of the screws under soft tissue is the root cause. The insertion point of S2AI screws is dorsal to the ala sacralis and deep under the muscle, while the insertion point of iliac screws is located in the PSIS and embedded subcutaneously. Chang et al. [Citation21] and Tavares et al. [Citation22] analyzed the trajectory of S2AI screws on computed tomography (CT) radiography. They found that the insertion point of S2AI screws was 15–20.5 mm deeper than that of iliac screws and the distance from the skin for S2AI screws versus that for iliac screws was 52–52.87 mm versus 32.46–37 mm. Due to the deep muscle and soft tissue covering, the S2AI screw tail is hidden in the body and not easily palpable on the skin surface. In addition, the good blood supply of the musculature forms the basis for surgical wound healing. In contrast, iliac screws are embedded subcutaneously and have a poor blood supply in the surrounding soft tissues. Intraoperative dissection of the fascia and soft tissue around the PSIS leads to the blood supply being further reduced. In the supine position, the compression of the skin by the protruding screws and the protruding PSIS aggravates ischemia, especially in thin patients with a limited layer of subcutaneous tissue. Although it has been reported in some studies [Citation1, Citation16] that the protrusion of the screws could be reduced by taking off part of the ilium, this operation does not eliminate the root cause, namely the superficial placement of the implants. These factors constitute the original crime of the postoperative wound infections after treatment with the iliac screw technique.
Another advantage of the S2AI screw technique is that the entry point of S2AI screws is in line with the lumbar pedicle screws. The traditional iliac screw technique requires an offset connector and multiplanar bending of the connecting rod because iliac screws are not in line with the pedicle screws. The S2AI screw technique only requires a straight rod, reducing the surgical complexity. In addition, in the iliac screw technique, longitudinal distraction reduction of the nonidentical axis between the pedicle screws and the iliac screws leads to the transverse separation of the sacral fractures. Since the S2AI screws are in the same line as the pedicle screws, longitudinal distractions do not cause fracture separation.
Interestingly, although the iliac screw technique requires additional dissection to PSIS, this extended dissection did not result in a significant increase in mean blood loss compared with the S2AI technique (539.13 ± 246.32 mL versus 405.26 ± 229.67 mL, p = 0.08). The poor blood supply of the PSIS covered only by skin and fascia is the main reason for this.
In our study, no patients experienced screw loosening or pull out. The S2AI screw group achieved the same clinical results as the iliac screw group for fixation strength. O’Brien et al. [Citation23] and Hoernschemeyer et al. [Citation19] demonstrated through biomechanical studies that there was no significant difference between S2AI screw fixation and iliac screw fixation in terms of stiffness or strength, and 65 mm S2AI screws were biomechanically equivalent to 90 mm iliac screws and 80 mm S2AI screws. Although S2AI screws are shorter than iliac screws, their 3 layers of cortex purchase make them as stable as iliac screws in the iliac cancellous bed [Citation23, Citation24].
Even though the S2AI screw technique provides these advantages, it also has shortcomings. Since it is essentially a bridging fixation (crossing the fractured sacrum, connecting the proximal lumbar spine with the distal ilium), the technique achieves the lumbopelvic stability at the expense of partial mobility of the lower back, similar to the iliac screw technique. Prolonged fixation can cause lower back stiffness, pain, and breakage of the screws [Citation25]. However, unlike the application of S2AI or iliac screws in spinal deformity correction, short-segment fixation is used in trauma. It reduces the compensatory strength of the remaining joint, which greatly reduces ankylosis and pain in the lower back. Nonetheless, a small proportion of patients still experience lower back discomfort. As in our study, there were three patients (13.0%) in the iliac screw group and one patient (5.3%) in the S2AI screw group with low back pain. Therefore, it is recommended that the implants should be removed 6–8 months postoperation after bony union, which is beneficial for lower back joint function recovery. Moreover, shorter segments of fixation have been tried by some surgeons. For example, Lee et al. [Citation26] chose to use S1 pedicle screws combined with S2AI screws for fixation. This technique does not disrupt lower lumbar mobility, however, it cannot reduce vertical displacement by distraction, so it is only suitable for patients with intact L5/S1 facet joints and intact S1 pedicles.
It is worth noting that the S2AI screw technique has the potential for destruction of the articular cartilage. An anatomical study by Xu et al. [Citation27] showed that the projection of the lateral sacral mass on the ilium was larger than that of the sacroiliac joint articular cartilage and the posterior part of that the lateral projection of the sacrum corresponded to the nonarticular area. Theoretically, S2AI screws can avoid violating the articular cartilage and preserve the integrity of the articular surface of the sacroiliac joint. However, another anatomical study by O’Brien et al. [Citation23] showed that articular violation occurred in 60% of S2AI screw techniques. Whether the destruction of sacroiliac articular cartilage is the cause of sacroiliac joint pain has not been reported in any literature. Hyun et al. [Citation25] analyzed 312 patients treated with S2AI screws and found that 3.2% had sacroiliac joint pain. Interestingly, these patients had a common feature, long-segment fixation. Rigid fixation with long-segment spinal fusion and low-strength sacroiliac joint fixation with a single S2AI screw bring about micromotion of the sacroiliac joint under high-intensity loading. Long-term compensation causes sacroiliac joint degeneration and pain. Ha et al. [Citation28] believed that fixation of the long segment led to the transmission of cantilevering forces to the sacroiliac joint, resulting in its excessive movement of the sacroiliac joint, which promoted pain, arthritis, and/or instrumentation failure. It is unknown whether the pain is caused by sacroiliac joint degeneration or sacroiliac joint cartilage destruction. However, for whatever reason, the rarity of sacroiliac joint pain is clinically acceptable.
Although the S2AI screw technique has many advantages, it is not suitable for all patients with sacral fractures. Recently, some surgeons [Citation29] reported the treatment of spinal deformity with a subcrestal iliac-screw technique, which had the same low-profile advantage as the S2AI technique and can also be considered an option for the treatment of sacral fractures. To date, the S2AI screw technique has been mainly indicated for Denis II/III sacral fractures. In addition, this study had a small sample size and a relatively short follow-up period. Therefore, other complications or some long-term complications that may have occurred may not be recorded. A prospective randomized controlled trial with a long follow-up time will be conducted in the future to further explore the treatment characteristics of the S2AI screw technique.
Conclusions
Both the S2AI screw technique and the iliac screw technique were effective in the treatment of sacral fractures. The S2AI screw technique exhibited better performance with fewer unplanned reoperations than the iliac screw technique for sacral fractures; thus, this technique is supposed to be an alternative and effective technique for sacral fractures. However, whether it can be recommended for general use for sacral fractures still requires further analysis.
Disclosure statement
The authors have no conflicts of interest to disclose in relation to this article.
References
- Yi C, Hak DJ. Traumatic spinopelvic dissociation or U-shaped sacral fracture: a review of the literature. Injury. 2012;43(4):402–408. doi:https://doi.org/10.1016/j.injury.2010.12.011.
- Backer HC, Wu CH, Vosseller JT, et al. Spinopelvic dissociation in patients suffering injuries from airborne sports. Eur Spine J. 2020;29(10):2513–2520. doi:https://doi.org/10.1007/s00586-019-05983-6.
- Bederman SS, Hassan JM, Shah KN, et al. Fixation techniques for complex traumatic transverse sacral fractures: a systematic review. Spine (Phila Pa 1976)). 2013;38(16):E1028–1040. doi:https://doi.org/10.1097/BRS.0b013e318297960a.
- Lindahl J, Makinen TJ, Koskinen SK, et al. Factors associated with outcome of spinopelvic dissociation treated with lumbopelvic fixation. Injury. 2014;45(12):1914–1920. doi:https://doi.org/10.1016/j.injury.2014.09.003.
- Sullivan MP, Smith HE, Schuster JM, et al. Spondylopelvic dissociation. Orthop Clin North Am. 2014;45(1):65–75. doi:https://doi.org/10.1016/j.ocl.2013.08.002.
- Konig MA, Jehan S, Boszczyk AA, et al. Surgical management of U-shaped sacral fractures: a systematic review of current treatment strategies. Eur Spine J. 2012;21(5):829–836. doi:https://doi.org/10.1007/s00586-011-2125-7.
- Pascal-Moussellard H, Hirsch C, Bonaccorsi R. Osteosynthesis in sacral fracture and lumbosacral dislocation. Orthop Traumatol Surg Res. 2016;102(1 Suppl):S45–S57. doi:https://doi.org/10.1016/j.otsr.2015.12.002.
- Ayoub MA. Displaced spinopelvic dissociation with sacral cauda equina syndrome: outcome of surgical decompression with a preliminary management algorithm. Eur Spine J. 2012;21(9):1815–1825. doi:https://doi.org/10.1007/s00586-012-2406-9.
- Ishida W, Elder BD, Holmes C, et al. S2-alar-iliac screws are associated with lower rate of symptomatic screw prominence than iliac screws: radiographic analysis of minimal distance from screw head to skin. World Neurosurg. 2016;93:253–260. doi:https://doi.org/10.1016/j.wneu.2016.06.042.
- Andrade NS, Okafor L, Neuman BJ. Novel technique for sacral alar-iliac (S2AI) fixation. Clin Spine Surg. 2018;31(9):373–376. doi:https://doi.org/10.1097/bsd.0000000000000574.
- Mazur MD, Mahan MA, Shah LM, et al. Fate of S2-alar-iliac screws after 12-month minimum radiographic follow-up: preliminary results. Neurosurgery. 2017;80(1):67–72. doi:https://doi.org/10.1227/NEU.0000000000001322.
- Wu B, Song K, Cheng J, et al. Second sacral sacralalar-iliac (S2AI) screw placement in adult degenerative scoliosis (ADS) patients: an imaging study. BMC Surg. 2021;21(1):181. doi:https://doi.org/10.1186/s12893-021-01139-w.
- De la Garza Ramos R, Nakhla J, Sciubba DM, et al. Iliac screw versus S2 alar-iliac screw fixation in adults: a meta-analysis. J Neurosurg Spine. 2019;30(2):253–258. doi:https://doi.org/10.3171/2018.7.SPINE18710.
- Shillingford JN, Laratta JL, Tan LA, et al. The free-hand technique for S2-alar-iliac screw placement: A safe and effective method for sacropelvic fixation in adult spinal deformity. J Bone Joint Surg Am. 2018;100(4):334–342. doi:https://doi.org/10.2106/JBJS.17.00052.
- Jones CB, Sietsema DL, Hoffmann MF. Can lumbopelvic fixation salvage unstable complex sacral fractures? Clin Orthop Relat Res. 2012;470(8):2132–2141. doi:https://doi.org/10.1007/s11999-012-2273-z.
- Qiao B, Liu J, Ni W, et al. Unilateral lumbopelvic fixation for AO/OTA Type C1 and C2 pelvic fractures: clinical efficacy and preliminary experiences in 23 patients. Injury. 2021;52(8):2333–2338. doi:https://doi.org/10.1016/j.injury.2021.05.018.
- Matta JM, Tornetta P. 3rd Internal fixation of unstable pelvic ring injuries. Clin Orthop Relat Res. 1996;329:129–140. doi:https://doi.org/10.1097/00003086-199608000-00016.
- Majeed SA. Grading the outcome of pelvic fractures. J Bone Joint Surg Br. 1989;71(2):304–306. doi:https://doi.org/10.1302/0301-620x.71b2.2925751.
- Hoernschemeyer DG, Pashuck TD, Pfeiffer FM. Analysis of the s2 alar-iliac screw as compared with the traditional iliac screw: does it increase stability with sacroiliac fixation of the spine? Spine J. 2017;17(6):875–879. doi:https://doi.org/10.1016/j.spinee.2017.02.001.
- Elder BD, Ishida W, Lo SL, et al. Use of S2-alar-iliac screws associated with less complications than iliac screws in adult lumbosacropelvic fixation. Spine (Phila Pa 1976). 2017;42(3):E142–149. doi:https://doi.org/10.1097/BRS.0000000000001722.
- Chang TL, Sponseller PD, Kebaish KM, et al. Low profile pelvic fixation: anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine (Phila Pa 1976)). 2009;34(5):436–440. doi:https://doi.org/10.1097/BRS.0b013e318194128c.
- Tavares Junior MCM, de Souza JPV, Araujo TPF, et al. Comparative tomographic study of the S2-alar-iliac screw versus the iliac screw. Eur Spine J. 2019;28(4):855–862. doi:https://doi.org/10.1007/s00586-018-5806-7.
- OʼBrien JR, Yu W, Kaufman BE, et al. Biomechanical evaluation of S2 alar-iliac screws: effect of length and quad-cortical purchase as compared with iliac fixation. Spine (Phila Pa 1976)). 2013;38(20):E1250–1255. doi:https://doi.org/10.1097/BRS.0b013e31829e17ff.
- Burns CB, Dua K, Trasolini NA, et al. Biomechanical comparison of spinopelvic fixation constructs: Iliac screw versus S2-alar-iliac screw. Spine Deform. 2016;4(1):10–15. doi:https://doi.org/10.1016/j.jspd.2015.07.008.
- Hyun SJ, Jung JM, Kim KJ, et al. Durability and failure types of S2-alar-iliac screws: An analysis of 312 consecutive screws. Oper Neurosurg (Hagerstown). 2020;20(1):91–97. doi:https://doi.org/10.1093/ons/opaa251.
- Lee H-D, Jeon C-H, Chung N-S, et al. Triangular osteosynthesis using an S1 pedicle screw and S2 alar iliac screw for a unilateral vertically displaced sacral fracture. World Neurosurg. 2020;142:57–61. doi:https://doi.org/10.1016/j.wneu.2020.06.161.
- Xu R, Ebraheim NA, Douglas K, et al. The projection of the lateral sacral mass on the outer table of the posterior ilium. Spine (Phila Pa 1976). 1996;21(7):790–794.
- Ha AS, Hong DY, Luzzi AJ, et al. Minimum 2-year analysis of S2-alar-iliac screw fixation for adult spinal deformity. Global Spine J. 2021;2192568220984478. doi:https://doi.org/10.1177/2192568220984478.
- Liu G, Hasan MY, Wong HK. Subcrestal iliac-screw: a technical note describing a free hand, in-line, low profile iliac screw insertion technique to avoid side-connector use and reduce implant complications. Spine (Phila Pa 1976)). 2018;43(2):E68–74. doi:https://doi.org/10.1097/brs.0000000000002239.
