Abstract
Aim
To compare the short- and long-term treatment outcomes of open radiofrequency ablation combined with splenectomy and pericardial devascularization versus liver transplantation for hepatocellular carcinoma patients with portal hypertension and hypersplenism.
Methods
During the study period, the treatment outcomes of consecutive HCC patients with portal hypertension and hypersplenism who underwent open radiofrequency ablation, splenectomy and pericardial devascularization (the study group) were compared with the treatment outcomes of a case-matched control group of HCC patients who underwent liver transplantation.
Results
The study group consisted of 32 patients, and the control group comprised 32 patients selected from 155 patients who were case-matched by tumor size, age, gender, MELD sore, tumor location, TNM classification, degree of splenomegaly and Child–Pugh staging. Baseline data on preoperative laboratory tests and tumor characteristics were comparable between the two groups. The mean follow-up was 43.2 ± 5.3 months and 44.9 ± 5.8 months for the study and control groups, respectively. Although the disease-free survival rates of the control group were better than those of the study group (P < 0.001), there was no significant difference in the cumulative overall survival time or the incidence of portal vein thrombosis between the two groups (P = 0.670, 0.083). Compared with the control group, the study group had significantly less intraoperative blood loss, and lower incidences of postoperative pleural effusion and pneumonia (all P < 0.05).
Conclusion
Open radiofrequency ablation, splenectomy and pericardial devascularization for small HCCs with portal hypertension and hypersplenism can be an alternative therapy for a subset of carefully selected patients under the shortage of liver donors.
Introduction
Hepatocellular carcinoma (HCC) is one of the most common tumors around the world and the second leading cause of cancer-related death in China [Citation1–4]. The majority of HCC patients in China have post-hepatitis B cirrhosis [Citation4], and they are complicated with portal hypertension and secondary hypersplenism. These patients often have anemia, thrombocytopenia, coagulation dysfunction, upper gastrointestinal bleeding and other complications [Citation5]. Liver cirrhosis and hypersplenism have usually been considered a contraindication to hepatectomy in HCC [Citation6]. Liver transplantation is the optimal therapy for these patients according to the many guidelines and consensus worldwide [Citation7]. However, the inadequacy of donors prolongs the waiting time of liver transplantation for many patients, and 20–30% of cases who originally met the transplant criteria were deleted from the transplant list due to tumor progression [Citation8]. During the wait for liver transplant, some treatments, such as radiofrequency ablation, can control tumor progression so the patient can stay within the transplant criteria. This is called transition therapy, and it can also reduce tumor recurrence after transplantation [Citation9, Citation10]. Radiofrequency ablation (RFA) is a well-recognized curative method for the treatment of HCC, especially in the treatment of small hepatocellular carcinoma [Citation11–14]. However, patients with related complications due to portal hypertension and hypersplenism such as thrombocytopenia are often contraindicated to percutaneous RFA therapy. In addition, it has been widely reported that splenectomy and pericardial devascularization for the treatment of portal hypertension and its related complications can improve anemia, thrombocytopenia, and coagulation dysfunction, and reduce the risk of upper gastrointestinal bleeding [Citation5, Citation15–17]. Hence, open radiofrequency ablation combined with splenectomy and pericardial devascularization in selected patients with small liver cancer complicated with portal hypertension and secondary hypersplenism was studied. The aim of our research was to evaluate the safety and effectiveness of open radiofrequency ablation combined with splenectomy and pericardial devascularization in the treatment of HCC patients with portal hypertension and hypersplenism, and to compare the treatment outcomes with a case-matched group of patients who underwent liver transplantation in the study duration.
Patients and methods
Case-control study
From June 2012 to March 2018, 32 consecutive HCC patients with portal hypertension and hypersplenism who underwent open radiofrequency ablation combined with splenectomy and pericardial devascularization (the study group) at the Institute of Hepatobiliary Surgery of Southwest Hospital of Army Medical University, a tertiary referral hospital, were retrospectively enrolled in this study. Patients in the study group were matched at a 1:1 ratio with patients who underwent liver transplantation during the study period by age, gender, tumor size, number of tumors, hepatitis B surface antigen (HBsAg) positivity, alpha-fetoprotein (AFP) level, TNM and Child–Pugh staging from the database of patients to form the control group. All patients were diagnosed with primary HCC with cirrhosis, portal hypertension, hypersplenism and gastroesophageal varices on imaging and pathological studies and their ages ranged from 18 to 80 years. The Child–Pugh stage of the enrolled cases was A or B. The patient characteristics(including number of patients, age, gender, Child–Pugh grading, MELD sore), preoperative laboratory tests(including AFP, ICG R-15 (%), hemoglobin, white cell count, platelet count, INR, albumin, ALT, AST, serum total bilirubin, APRI, and HBV-DNA levels), and tumor characteristics (including BCLC staging, TNM classification, degree of esophageal varices, history of gastrointestinal bleeding, tumor location, number of tumors, diameter of tumor, degree of splenomegaly, and internal diameter of main portal vein) of the two groups are presented in . The peri-operative and long-term prognosis in both groups were compared and analyzed.
Table 1. Baseline data of the open radiofrequency ablation and splenectomy group and the liver transplantation group.
The study was approved by the Ethics Committee of the First Affiliated Hospital of Army Medical University, PLA (KY2021169). Because of the retrospective nature of the research, the committee waived the need for individual consent. All patients underwent the same preoperative assessment protocol which included gadoxetate disodium-enhanced magnetic resonance imaging, chest and abdomen CT scans, hepatic contrast-enhanced ultrasound, electronic gastroscopy, ECG and blood biochemistry. The Child–Pugh grading and the indocyanine green clearance test at 15 minutes (ICG-R15) were used to evaluate liver function.
Open radiofrequency ablation with splenectomy and pericardial devascularization procedure
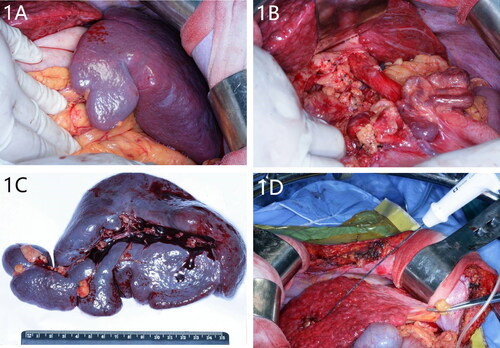
A self-retained retractor was used after an incision using a midline incision with a right horizontal extension. Splenectomy and pericardial devascularization were first performed. In all patients, the spleen enlargement extended beyond the left subcostal margin (). Pericardial vessels were then dissected proximally for more than 7 cm (). After splenectomy, intraoperative ultrasonography (IOUS) was routinely used to determine the location, size and number of tumors. Radiofrequency ablation of HCC was performed (). When the tumor was less than 3 cm, one radiofrequency needle was used to repeatedly puncture, and ablate the tumor. The RF power was 120 watts, the working time was 3 minutes (). When the tumor was larger than 3 cm and less than 5 cm, two radiofrequency ablation needles were used for repeated puncture and ablation. The RF power was 180 watts, and the working time was 5 minutes. The device used was a multipolar internally cooled-tip CelonProSurge™ (Celon—POWER System OLYMPUS Medical®).
Figure 1. (A) Intraoperative exploration revealed that the patient’s spleen was seriously enlarged. The spleen enlarged beyond the left subcostal margin. (B) The pericardia vessels were dissected upward for at least 5 cm. (C) The removed spleen was severely enlarged. (D) The RFA needle was inserted into the center of the tumor to initiate the radiofrequency ablation.
Statistical analysis
The study endpoints were tumor recurrence and death. Tumor recurrence was defined as the appearance of clinically visible or imaging evaluable lesions two months after surgery. The time from operation to recurrence was defined as recurrence-free survival (RFS). Analysis of the categorical data was performed using the chi-square test and Fisher’s exact test. Continuous data with a nonnormal distribution were analyzed using the Mann–Whitney U test. The Kaplan–Meier method was applied to generate survival curves, including those for the cumulative overall survival (OS) and RFS, for both groups. The log–rank test was performed to evaluate the significance of the differences between the two groups. All p values were two-sided, and p < 0.05 was deemed statistically significant. Statistical analyses were performed with SPSS 23.0 for Windows computer software (SPSS Inc., Chicago, IL).
Results
The patient characteristics, preoperative laboratory tests and tumor characteristics are shown in . There were no significant differences between the two groups in patient’ characteristics, tumor location, size, number of tumors, degree of splenomegaly or preoperative laboratory tests. Thus, patients in the two groups were comparable.
The intra- and postoperative results in the two groups are shown in . There were no significant differences in the intraoperative transfusion volume or the number of patients who needed blood transfusion between the two groups. However, there was significantly less intraoperative blood loss in the study group than in the control group (P = 0.017). The perioperative maximum level of platelet count in the study group was markedly higher than that in the control group (P < 0.001). The postoperative serum total bilirubin levels in the study group were markedly lower than those in the control group (P = 0.005). There were 17 and 29 patients who developed postoperative pleural effusion, respectively, and the difference was statistically significant (P = 0.001). There were 5 and 18 patients who developed pneumonia in the study and control groups, respectively, and the difference was also significant (P = 0.001). No patients in this study developed postoperative liver failure. There were 11 and 5 patients who were complicated by portal vein thrombus in the study and control groups, respectively, and there was no significant difference between the two groups (P = 0.083). Platelet filtration to avoid coagulation complications was given to two patients with platelet counts of more than 800 × 109/L postoperatively. These high platelet counts gradually resolved spontaneously. One patient in the study group developed postoperative abdominal bleeding, and this patient subsequently died from other complications arising from cirrhosis and its underlying diseases.
Table 2. Intra- and postoperative results of HCC of the open radiofrequency ablation and splenectomy group and the liver transplantation group.
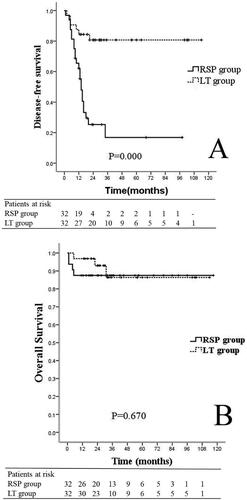
The mean durations of follow-up were 43.2 ± 5.3 months for the study group and 44.9 ± 5.8 months for the control group (P = 0.873). The DFS rates in the control group were significantly better than those in the study group (P < 0.001) (). The median DFS was 14 months for the study group and was not reached for the control group. There was no significant difference in the cumulative overall survival between the two groups (P = 0.670) (). For patients with intrahepatic tumor recurrence, repeated liver resection or radiofrequency ablation was performed if technically possible. For patients who had multiple recurrent lesions confined to the liver, TACE was used to treat them. Systemic therapies were given to treat patients with extrahepatic metastasis.
Figure 2. (A) Survival curves of DFS for patients with HCC and hypersplenism who were treated with open radiofrequency ablation combined liver splenectomy and pericardial devascularization (n = 32) and liver transplantation (n = 32), P < 0.001 (study group vs. control group; Kaplan–Meier, log–rank test). (B) OS curves of for patients with HCC and hypersplenism who were treated with open radiofrequency ablation combined with splenectomy and pericardial devascularization (n = 32) and liver transplantation (n = 32), P = 0.670 (study group vs. control group; Kaplan–Meier, log–rank test).
Discussion
Hepatocellular carcinoma is still one of most deadly malignancies, especially for patients with liver cirrhosis. However molecular targeted therapies and immunotherapies have developed rapidly in recent years [Citation18]. Therefore, predicting the prognosis of HCC patients is particularly important. Studies have shown that some inflammatory biomarkers may be effective prognostic factors for patients with HCC, such as the lymphocyte-monocyte ratio, and neutrophil-to-lymphocyte ratio [Citation19, Citation20]. These inflammatory factors can provide a basis for the postoperative treatment of patients with HCC.
Liver transplantation is the recommended treatment aiming to cure patients with HCC combined with portal hypertension and hypersplenism [Citation21]. However, many patients do not have the opportunity to receive this treatment because of the severe shortage of liver donors [Citation22, Citation23]. This study showed that an alternative surgical treatment could prolong survival in well-selected HCC patients with portal hypertension and hypersplenism, and in some patients the treatment offered the chance of cure.
Patients included in this study had small HCC with portal hypertension and hypersplenism caused by cirrhosis. Many patients in this study group had a history of gastrointestinal bleeding. Thus if they were not effectively treated, a significant proportion of them will develop further gastrointestinal bleeding which can lead to liver failure and death. Splenectomy and pericardial devascularization have been reported to raise postoperative white blood cell and platelet counts, develop blood coagulation, reduce postoperative gastrointestinal bleeding incidence, enhance immunity and improve quality of life [Citation5, Citation24, Citation25]. Most HCC patients with cirrhosis complicated by portal hypertension and hypersplenism cannot tolerate hepatectomy. Although these patients can still be treated with radiofrequency ablation, the problems resulting from portal hypertension and hypersplenism remain. This innovative surgical treatment of open abdominal radiofrequency ablation combined with splenectomy and pericardial devascularization was designed to solve all these problems, and hopefully these patients can have better long-term survival outcomes. The results of this study showed that there was no significant difference in the overall survival rates between the two groups. As this treatment did not increase postoperative complications, this treatment was shown to be safe and effective. These findings are in agreement with previously reported results [Citation25, Citation26]. However, the tumor recurrence rate in the study group was significantly higher than that in the control group. There are several reasons to explain this observation. First, patients in the liver transplant group had a healthy liver after transplantation, while the study group still had a cirrhotic liver. Second, patients in the study group can have MVI and radiofrequency ablation of HCC lesions may not be adequate to treat these patients [Citation27–29]. Third, new HCC nodules can occur on postoperative follow-up in the study group [Citation30, Citation31].
The key to success in using open radiofrequency ablation to treat HCC is accurate location of liver cancer nodules and accurate determination of the extent of radiofrequency ablation [Citation30]. If the extent of radiofrequency ablation is too small, residual active tumor cells can be left behind. However, if the extent of radiofrequency ablation is too large, the treatment can lead to severe postoperative liver dysfunction, massive ascites, or even perioperative death. In this study, for a single tumor ≤ 3 cm, the extent of radiofrequency ablation was 2 cm from the edges of the tumor. For 2 to 3 tumors with each tumor of less than 3 cm, the extent of radiofrequency ablation aimed at 1 cm. Open radiofrequency ablation was used in this study instead of hepatectomy because all patients enrolled in this study had tumors of less than 3 cm. Based on the BCLC staging guidelines, radiofrequency ablation for these patients could achieve radical cure [Citation32]. Moreover, as some of these lesions were located centrally, hepatectomy could result in acute liver failure, massive gastrointestinal bleeding, and death. Previous reports have shown that there is a significant probability of portal vein thrombosis developing after splenectomy and pericardial devascularization [Citation33]. This study showed that 11 patients in the study group developed this complication, which was treated with anticoagulation and conservative treatment. No patients developed serious complications of portal thrombosis.
There are limitations of this study. First, this is a pilot study of retrospectively collected data from a single institution. Second, the patients included in this study were mainly patients with small HCC and portal hypertension and hypersplenism. These patients were rigorously screened. Whether the conclusions of this study can be generalized to other HCC is unclear. Third, the surgeons involved in this study were experienced in radiofrequency ablation and cirrhotic liver surgery. The study’s conclusions may not be extrapolated to inexperienced surgeons. Fourth, most patients in this study had HBV-related HCC. Whether the results obtained in this study can be applicable to HCC with other etiologies is not known.
Conclusion
Open radiofrequency ablation combined with splenectomy and pericardial devascularization to treat small HCC with portal hypertension and hypersplenism was demonstrated to be safe and effective in carefully selected patients. With the current severe shortage of liver donors, this operation can be used as an alternative treatment for patients who have little chance of getting a donated liver.
CRediT authorship contribution statement
Xishu Wang: Conceptualization, Formal analysis, Investigation, Writing-original draft, Writing-review & editing, Visualization, Ximin Sun: Formal analysis, Investigation, Writing-original draft, Visualization, Yongrong Lei: Formal analysis, Investigation, Visualization. Jun Pei: Investigation, Visualization, Kuansheng Ma: Investigation, Writing—review & editing. Kai Feng: Investigation, Writing—review & editing. Wan Yee Lau: Final drafting of paper. Feng Xia: Conceptualization, Investigation, Data curation, Writing-review & editing, Supervision, Funding acquisition, Project administration.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391(10127):1301–1314. doi:10.1016/S0140-6736(18)30010-2.
- EASL-EORTC. Clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56(4):908–943. doi:10.1016/j.jhep.2011.12.001.
- Bruix J, Gores GJ, Mazzaferro V. Hepatocellular carcinoma: clinical frontiers and perspectives. Gut. 2014;63(5):844–855. doi:10.1136/gutjnl-2013-306627.
- Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians. 2021;71(3):209–249. doi:10.3322/caac.21660.
- Oh JW, Ahn SM, Kim KS, et al. The role of splenectomy in patients with hepatocellular carcinoma and secondary hypersplenism. Yonsei Med J. 2003;44(6):1053–1058. doi:10.3349/ymj.2003.44.6.1053.
- Zhang X. Synchronous splenectomy and hepatectomy for patients with hepatocellular carcinoma and hypersplenism: a case-control study. WJG. 2015;21(8):2358. doi:10.3748/wjg.v21.i8.2358.
- Llovet JM, Fuster J, Bruix J; Barcelona Clinic Liver Cancer (BCLC) Group. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology. 1999;30(6):1434–1440. doi:10.1002/hep.510300629.
- Donadon M, Solbiati L, Dawson L, et al. Hepatocellular carcinoma: the role of interventional oncology. Liver Cancer (Basel). 2017;6(1):34–43. doi:10.1159/000449346.
- Mazzaferro V, Battiston C, Perrone S, et al. Radiofrequency ablation of small hepatocellular carcinoma in cirrhotic patients awaiting liver transplantation: a prospective study. Ann Surg. 2004;240(5):900–909. doi:10.1097/01.sla.0000143301.56154.95.
- Lu DS, Yu NC, Raman SS, et al. Percutaneous radiofrequency ablation of hepatocellular carcinoma as a bridge to liver transplantation. Hepatology. 2005;41(5):1130–1137. doi:10.1002/hep.20688.
- Livraghi T, Meloni F, Di Stasi M, et al. Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: is resection still the treatment of choice? Hepatology. 2007;47(1):82–89. doi:10.1002/hep.21933.
- Cho YK, Kim JK, Kim WT, Chung JW. Hepatic resection versus radiofrequency ablation for very early stage hepatocellular carcinoma: a Markov model analysis. Hepatology. 2010;51(4):1284–1290. doi:10.1002/hep.23466.
- Cucchetti A, Piscaglia F, Cescon M, et al. Cost-effectiveness of hepatic resection versus percutaneous radiofrequency ablation for early hepatocellular carcinoma. J Hepatol. 2013;59(2):300–307. doi:10.1016/j.jhep.2013.04.009.
- Pompili M, Mirante VG, Rondinara G, et al. Percutaneous ablation procedures in cirrhotic patients with hepatocellular carcinoma submitted to liver transplantation: assessment of efficacy at explant analysis and of safety for tumor recurrence. Liver Transpl. 2005;11(9):1117–1126. doi:10.1002/lt.20469.
- Sugawara Y, Yamamoto J, Shimada K, et al. Splenectomy in patients with hepatocellular carcinoma and hypersplenism. J Am Coll Surg. 2000;190(4):446–450. doi:10.1016/s1072-7515(99)00294-x.
- Cai Y, Liu Z, Liu X. Laparoscopic versus open splenectomy for portal hypertension: a systematic review of comparative studies. Surg Innov. 2014;21(4):442–447. doi:10.1177/1553350613520513.
- Kim SH, Kim DY, Lim JH, et al. Role of splenectomy in patients with hepatocellular carcinoma and hypersplenism. ANZ J Surg. 2013;83(11):865–870. doi:10.1111/j.1445-2197.2012.06241.x.
- Abd EAM, Facciorusso A, Nayfeh T, et al. Immune checkpoint inhibitors for unresectable hepatocellular carcinoma. Vaccines (Basel). 2020;8(4):616. doi:10.3390/vaccines8040616.
- Facciorusso A, Del PV, Crucinio N, et al. Lymphocyte-to-monocyte ratio predicts survival after radiofrequency ablation for colorectal liver metastases. World J Gastroenterol. 2016;22(16):4211–4218. doi:10.3748/wjg.v22.i16.4211.
- Lin S, Hu S, Ran Y, Wu F. Neutrophil-to-lymphocyte ratio predicts prognosis of patients with hepatocellular carcinoma: a systematic review and meta-analysis. Transl Cancer Res. 2021;10(4):1667–1678. doi:10.21037/tcr-20-3237.
- Faitot F, Allard MA, Pittau G, et al. Impact of clinically evident portal hypertension on the course of hepatocellular carcinoma in patients listed for liver transplantation. Hepatology. 2015;62(1):179–187. doi:10.1002/hep.27864.
- Samuel D, Coilly A. Management of patients with liver diseases on the waiting list for transplantation: a major impact to the success of liver transplantation. BMC Med. 2018;16(1)113. doi:10.1186/s12916-018-1110-y.
- Vodkin I, Kuo A. Extended criteria donors in liver transplantation. Clin Liver Dis. 2017;21(2):289–301. doi:10.1016/j.cld.2016.12.004.
- Tomikawa M, Hashizume M, Akahoshi T, et al. Effects of splenectomy on liver volume and prognosis of cirrhosis in patients with esophageal varices. J Gastroenterol Hepatol. 2002;17(1):77–80. doi:10.1046/j.1440-1746.2002.02656.x.
- Li W, Shen SQ, Wu SM, et al. Simultaneous hepatectomy and splenectomy versus hepatectomy alone for hepatocellular carcinoma complicated by hypersplenism: a meta-analysis. Onco Targets Ther. 2015;8:2129–2137. doi:10.2147/OTT.S87580.
- Liu X, Chen Z, Yu M, et al. Safety of simultaneous hepatectomy and splenectomy in the treatment of hepatocellular carcinoma complicated with hypersplenism: a meta-analysis. Gastroenterol Res Pract. 2019;2019:9065845. doi:10.1155/2019/9065845.
- Lee S, Kang TW, Song KD, et al. Effect of microvascular invasion risk on early recurrence of hepatocellular carcinoma after surgery and radiofrequency ablation. Ann Surg. 2021;273(3):564–571. doi:10.1097/SLA.0000000000003268.
- Imai K, Yamashita YI, Yusa T, et al. Microvascular invasion in small-sized hepatocellular carcinoma: significance for outcomes following hepatectomy and radiofrequency ablation. Anticancer Res. 2018;38(2):1053–1060. doi:10.21873/anticanres.12322.
- Yamashita YI, Imai K, Yusa T, et al. Microvascular invasion of single small hepatocellular carcinoma ≤3 cm: predictors and optimal treatments. Ann Gastroenterol Surg. 2018;2(3):197–203. doi:10.1002/ags3.12057.
- Kikuchi L. Percutaneous radiofrequency ablation for early hepatocellular carcinoma: risk factors for survival. WJG. 2014;20(6):1585. doi:10.3748/wjg.v20.i6.1585.
- Ercolani G, Grazi GL, Ravaioli M, et al. Liver resection for hepatocellular carcinoma on cirrhosis: univariate and multivariate analysis of risk factors for intrahepatic recurrence. Ann Surg. 2003;237(4):536–543. doi:10.1097/01.SLA.0000059988.22416.F2.
- Forner A, Reig ME, de Lope CR, Bruix J. Current strategy for staging and treatment: the BCLC update and future prospects. Semin Liver Dis. 2010;30(1):61–74. doi:10.1055/s-0030-1247133.
- Buzelé R, Barbier L, Sauvanet A, Fantin B. Medical complications following splenectomy. J Visc Surg. 2016;153(4):277–286. doi:10.1016/j.jviscsurg.2016.04.013.
